What is included in the life history. V
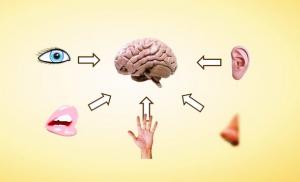
Anamnesis vitae (life history) is information about the life of an individual, which allows us to understand some of the characteristics of the body, and is also important for establishing the nature of the pathology and determining the factors of its occurrence. The doctor collects information about the patient's life history by interviewing him, following a specific plan.
Plan for collecting information about the patient's life
Let's look at a schematic example of how to write a life history. All information received from the patient is entered into the medical history in a certain order, including several mandatory sections.
Biographical information:
- place of birth - is of particular importance, since specific diseases are common in some areas;
- what age were the parents when the patient was born;
- how the pregnancy proceeded - the use of medications during gestation, past infectious diseases, threat of miscarriage, etc.;
- delivery - degree of full term, what kind of child is in the family and from what birth;
- natural, mixed or artificial feeding;
- living conditions in childhood and adolescence - region, living conditions, family circumstances, nutrition;
- physical and mental development - what are the features;
- puberty - the time of onset;
- factors that caused the pathology and conditions affecting the course and outcome of the disease - poor nutrition, poor care, violation of sanitary standards, poor physical development, etc.
Past infections:
- diphtheria, chicken pox, scarlet fever, rubella, measles, mumps, their clinical picture and the presence of consequences;
- colds;
- congenital infectious diseases and chronic foci of infection (for example, caries, sinusitis), in addition, it is determined whether there were trips to countries with unfavorable epidemiological conditions.
Information about previous diseases.
Data on work in hazardous industries.
Addictions - substance abuse, alcoholism, tobacco smoking, drug addiction.
Family and hereditary history - find out the closest relatives. For example, if there is a person with tuberculosis in the family, then there is a possibility that all family members will become infected. In addition, a predisposition to phenotypic diseases is revealed. In case of existing hereditary pathologies that are passed on to each new generation, the type of carriage and the degree of expression of the gene, as well as the type of inheritance, are determined.
Allergy history - whether the patient or his relatives are allergic to medications, foods, etc.
Each section is described in detail by the doctor.
Collecting information about life
Giving an example of a child’s life history, it is worth noting that it has some features that are associated with its age. The doctor’s task is to ask the baby’s mother in great detail about the following periods:
- prenatal - intrauterine development;
- intrapartum - from the onset of labor to birth;
- early postnatal - from birth to independent feeding;
- information about life in infancy.

All the smallest details are important, indicating how the baby developed. It is especially important to analyze all of the above stages of development when writing a medical history. Using the example of the life history of children under three years of age, let’s look at what other information is collected:
- about the peculiarities of upbringing;
- about diseases that the baby suffered at an early age, as well as about hereditary pathologies;
- living conditions in which the child grows and develops;
- feeding - artificial, natural or mixed;
- what vaccinations were given and the reaction to them;
- epidemiological situation.
Collecting information about the lives of young children
An example of a life history of a young child:
- How old is the baby and from what pregnancy? All previous ones are described and how they ended.
- The course of pregnancy - whether there were toxicoses, how they manifested themselves. The presence of chronic diseases, previous infections, occupational hazards in the mother, treatment in a hospital, taking medications.
- Nutrition and daily routine while expecting a baby. Was the woman on maternity leave?
- Duration and complications during childbirth, as well as: when and how the baby cried, weight, height, when they were applied to the breast for the first time and how often they were applied, how they sucked, on what day they were discharged home and weight at discharge.
- Development in the first three years of life - physical, static and motor skills, mental.
- Baby's behavior in home and unfamiliar surroundings. Attitude towards adults and children around him.
- Duration of sleep.
- Type of feeding, feeding regimen, timing of complementary foods. Diet at the onset of the disease.
- Was vitamin D prescribed and when?
- When did the first tooth appear, how did the others emerge and in what order. Number of teeth by the end of the first year of life.
- What operations and diseases occurred and when.
- Vaccination - what vaccinations and reaction to them. Mantoux and the result.
- Allergic reactions.
- Infectious contacts.
Collecting information about the lives of older children
An example of a life history of a child 12 years of age and older:
- What kind of child is there in the family?
- Development in early childhood.
- Behavior at home and in a group. School performance, aptitude for which academic subjects.
- Addictions.
- Past surgical interventions and illnesses.
- Vaccine prevention.
- Allergy history.
- Infectious contacts.
Family history
Above are examples of the life history of a child at different ages. However, this also includes collecting information about the family. The doctor finds out the following information:
- Age and passport information of both parents.
- The health status of official guardians and close relatives on both sides.
- The presence of infectious, oncological, mental, allergic, nervous, endocrine pathologies in the family.
- Bad habits of parents - smoking, alcoholism.
- Occupational hazards.
- A genealogical map is being compiled. The scope of this study is determined by the doctor.

Some features of filling out a medical history
The child’s medical history is kept from the beginning of the patient’s admission to an inpatient healthcare facility. This is the so-called protocol for examining a sick child. Which reflects the main types of research, expert opinions, preliminary, main, differential and final diagnoses, various information about the patient, including the child’s life history. An example of filling out this part of the medical history is as follows. Information for this section is available in the referral issued at the outpatient clinic, an extract from the baby’s outpatient card or the child’s development history, or in the doctor’s notes upon admission to the hospital, which reflect the results of the initial examination. To collect a medical history of a child under three years of age, the doctor interviews his parents:
- The number of pregnancies, how they ended, the health status and age of the children. If there are deceased, the cause of death and age are determined.
- Antenatal period - the state of health of the expectant mother during the period of bearing the baby, past illnesses, pharmacotherapy.
- Course of labor - premature, urgent, its duration, complications.
- The baby's reaction is when he screams, a loud or weak cry.
- Weight and height at birth.
- When they put the newborn to the breast, how he sucked, how he took the breast.
- On what day were the mother and baby discharged? Baby's body weight at discharge.
- Diseases during the neonatal period.
- Development: physical in the first year of life, statics and motor skills, mental.
- Feeding, frequency of breastfeeding. At what age is complementary feeding introduced? Nutritional pattern at the time of the present illness.
- When the first teeth appeared, their number increased by the beginning of the second year of life.
- Past illnesses, surgeries, injuries, complications and consequences.
- Vaccinations, the age at which the vaccination was given and the reaction to its administration are indicated.
- Having allergies.
- Infectious contacts.

An example of a life history of a patient older than three years:
- Which child is in the family?
- Development in early childhood.
- Behavioral characteristics.
- Past illnesses, injuries, surgeries.
- Vaccinal prophylaxis and tuberculin tests.
- Allergic reactions.
- Infectious contacts.
An example of a life history in therapy
When collecting information from an individual with suspected kidney pathology, pay attention to the following information:
- The risk factors for kidney pathology are reduced - long-term living in an unheated room, regular hypothermia, working in a draft or outdoors.
- Past genital diseases, diabetes, tuberculosis.
- It is being determined whether work is associated with heavy lifting, long walking, or driving, as this negatively affects the course of kidney disease and provokes attacks of renal colic.
- Heredity - whether there were kidney abnormalities, amyloidosis, urolithiasis in relatives. They ask women about pregnancy, because it can be a provocateur of nephropathy or exacerbation of chronic pathology.
Information about the dental patient
The patient's life history is important for the doctor, as it allows him to more reliably assess the patient's current condition and make a prognosis for therapy. An example of a life history of a patient admitted to dental surgery:
- The doctor interviews the individual about living conditions, rest, work, diet, and physical activity.
- Information about the health of parents.
- The course of pregnancy and delivery.
- Bad habits.
- Hereditary pathologies in terms of congenital malformations of the maxillofacial region.
- Development in childhood, type of feeding, past infectious and other diseases, results of therapy.
- Obstetric history is taken into account.
- Previous diseases, their course, treatment and outcome are also taken into account.

When obtaining information about family history, the presence of autoimmune and allergic pathologies, malignant tumors, mental disorders, syphilis, and tuberculosis in relatives is analyzed.
Completing medical documentation
Taking an anamnesis, or in other words, interviewing a patient begins with questions that are necessary to fill out a medical history. Using a life history as an example, let’s look at what information the doctor is interested in:
- Some biographical information about the patient.
- Diseases suffered during previous periods of life.
- Addictions.
- Hereditary factors.
In all of the above points, the doctor will be interested in those issues that are directly related to the present pathological process. Therefore, depending on the profile of the disease, the list of questions may differ.
History collection scheme
Thanks to a clearly developed scheme, each doctor, when compiling a medical history, can use an example of an adult’s life history:
- Where he was born.
- Parents' age at birth.
- The nature of pregnancy.
- Information about childbirth.
- Type of feeding.
- Permorbid conditions: rickets, malnutrition, etc.
- Physical and mental development.
- Timing of puberty.
- The reasons that resulted in the disease, the conditions influencing its course, and the outcome.
- Children's infectious diseases.
- Frequency of colds.
- Congenital pathologies, including infectious ones.
- Working conditions and the presence of occupational hazards.
- Harmful addictions.
- Well-being of close relatives.
Information about the lives of male patients
What questions does a doctor ask during a survey to the stronger half of humanity? Let’s look at the example of a man’s life history. Plan for collecting information for completing a medical history:
- Biography - place and year of birth, what family he was born into, what age the child was, how he developed and grew.
- Education.
- Military service, participation in hostilities.
- Have you been in prison?
- Do you have intimate problems?
- Family status.
- Work history - at what age and where did you start working, working conditions and modes, night shifts, occupational hazards.
- Housing conditions, how many people live together.
- Being in environmentally unfavorable areas.
- Diet, diet.
- Addictions - at what age does one smoke, drink alcohol-containing drinks or their counterfeits and in what quantities, take narcotic and toxic substances.
- Diseases that were previously diagnosed, injuries, contusions, operations and wounds are listed in chronological order and indicating the age when they occurred. The duration of treatment and the presence of complications are also described. If blood or its components were transfused, describe whether there was a reaction to this procedure.
- Vaccine prevention - what vaccinations were given, when, last date. Past infectious and venereal diseases, tuberculosis, hepatitis.
- Was there an allergy and to what allergen, seasonality if any.

- Information on temporary disability certificates and their duration for the current year. Whether there is a disability and what group, its cause and date of establishment.
- Well-being of close relatives. Is there a burdened heredity, the presence of cancer, cardiovascular, endocrine pathology, mental illness, alcoholism. A history of suicide attempts, mental health problems, tuberculosis or syphilis.
- An example of an epidemiological life history - a possible source of infection, route of infection, immune status. Contacts with infectious patients are identified. Staying in an epidemically disadvantaged area. Participation in hunting, care and contact with wild animals.
- Sexual history - casual relationships, lack of protected sex, frequency of changing partners. Sexually transmitted and infectious pathologies in partners.
- Were methods of alternative medicine, acupuncture, Tibetan medicine, treatment by healers and shamans used in the treatment, and the effectiveness of such an alternative method of treatment.
An example of a woman's life history
Collecting information about a woman’s life has some features and is collected according to the following scheme:
- Biography, starting from infancy.
- Pathological conditions that an individual has suffered from since childhood, including mental, venereal, oncological, viral, nervous, endocrine.
- Operations and injuries.
- Gynecological history - how many pregnancies, births, abortions there were, when menstruation began, their regularity, date of last menstruation, time when menopause began.
- Presence of allergies and type of allergen.
- Whether you were on sick leave during the current year, their duration, whether there was a disability and for what disease.
- Have there been blood transfusions and when, the reason.
- Family status.
- Working and living conditions.
- Bad habits - drinking alcoholic beverages, drugs, smoking.
- Hereditary pathologies.

As can be seen in this example, the woman’s life history covers a wider range of issues.
Conclusion
Life history is a kind of disease history that gives a socio-biological characteristic of an individual. The result of its analysis is a diagnosis, as well as a prognosis. It contains information about both work activity and living conditions. And if they occur in an environmentally unfavorable region or in an infectious focus, then this will help the doctor quickly determine the diagnosis and identify the impact of negative factors (stressful, chemical, etc.) on the individual’s body. The doctor will primarily be interested in information that is in any way related to the development of the disease. For example, working in hazardous industries reduces the resistance of the individual’s body and significantly weakens the immune system. Thus, a life history makes it possible to assess the individual characteristics of the body, which is undoubtedly important for choosing treatment methods and preventing complications.
| Parameter name | Meaning |
| Article topic: | ANAMNESIS VITAE |
| Rubric (thematic category) | Medicine |
ANAMNESIS MORBI
From the age of three, after registration in preschool children, frequent acute respiratory infections, non-recurrent obstructive bronchitis, not always with an increase in body temperature. Almost always there is high eosinophilia in the blood up to 20%. During light periods, the symptoms of rhinitis are mainly congestion, observed by an ENT doctor, and received courses of treatment.
I was sick with ARVI on March 25-26, 2013. There was a fever, cough, and runny nose. Worsening since April 4-5. At home in the evening we did about 18 inhalations with Berodual. Subsequently, the wheezing stopped.
On the evening of April 5, 2013, shortness of breath and difficulty breathing appeared. She was taken to the hospital by ambulance, accompanied by her father.
In the hospital, ward mode, table No. 15, Berodual - 20 drops, Pulmicort 0.25 mg 2 times a day, ECG, spirography, OAK, OAM, biochemical blood test, stool test for worm eggs were performed.
Antenatal period:
The child was born from the 1st pregnancy of the 1st birth. There is no information about previous pregnancies and the duration of the interval between the current and the previous one. There are no threatening factors regarding the parents' profession. The birth proceeded without complications. In the first half of pregnancy - nausea.. During this pregnancy, the woman in labor ate healthy food: vegetable salads, fruits, fermented milk products (kefir, cottage cheese), lightly salted fish, liver, chicken, buckwheat, rice porridge. I didn’t have ARVI.
Conclusion: the pregnancy proceeded without complications.
Intranatal period:
The course of labor is urgent. There is no information about amniocentesis and the nature of amniotic fluid.
Conclusion: obstetric and gynecological history is not burdened.
Newborn period:
The baby is full term. Apgar score: 8 points. The child screamed immediately, the scream was loud. There is no information on the degree of asphyxia. There are no birth injuries.
Body weight at birth - 2750 g, body length at birth - 51 cm. Mass growth coefficient MRI = 2750 (g) / 51 (cm) = 53.9
The remainder of the umbilical cord fell off on the 3rd day. The umbilical wound healed without complications. Attached to the breast after birth.
BCG vaccination in the maternity hospital was done on July 13, 2001 0.1*0.05 intravenously with 221/5037 3 mm.
Information on physiological weight loss is not available. By the time of discharge, physiological weight loss had not been restored. She was discharged home on the third day in satisfactory condition,
Isiological jaundice of newborns and erythema of newborns occurred. There is no information about group incompatibility and Rh incompatibility of mother and child, diseases of the skin and navel, respiratory and digestive organs, and septic diseases.
Conclusion: the child’s development during the newborn period is not burdened.
Feeding:
The time for the first breastfeeding is after birth. Feeding is regular, with an interval of 3-4 hours at night (feeding at the request of the child). Natural feeding up to 11.5 months. The reason for weaning is not indicated in the outpatient card. There is no information on the prevention of hypolactia. From 7 months, the introduction of vegetable purees and cereals. From 8 months the introduction of porridge, soups, juices, fruits. There is no information about getting vitamin D.
The child's current diet:
Breakfast: tea with sugar, sandwich with sausage.
Lunch: soup, salad, tea.
Dinner: soups, potatoes, pasta, meat. Likes: sweets and fruits.
Conclusion: the baby was put to the breast on time, complementary foods were introduced according to age standards. There is little fruit in the diet.
Dynamics of the child’s physical and psychomotor development:
Fixation of gaze on an object begins at 1 month, holding head at 3 months, turns head from 4 months, from 4 months turns from back to stomach, from 5 months from stomach to back, sat from 6.5 months, crawls from 7 months, I've been walking by the hand since I was 11 months old. From 2 months she walked, smiled, from 3 months she recognized her own people, from 4 months she recognized her mother and relatives, she babbled from 7 months, first words at 10 months, vocabulary by the first year of life - 8 words.
Conclusion: the main anthropometric parameters are in the area of “very low” and “average” values. RF below average, microsomatotype, disharmonious development.
The first teeth erupted at 8 months - 2 lower central incisors. By the age of 11, the dental formula looked like this:
6 5 4 3 2 1 1 2 3 4 5 6
6 5 4 3 2 1 1 2 3 4 5 6
The child's psychomotor development during the epicrisis period corresponds to his age.
Conclusion: CPD is age appropriate.
INFORMATION ABOUT PREVENTIVE VACCINATIONS:
1. BCG vaccination in the maternity hospital it was done on July 13, 2001 0.1*0.05 intravenous with 221/5037 3 mm.
2. Mantoux reaction:
03/13/02 – 2 TV. Neg.
4.10.03 – doubtful
02/18/05 – p – 17 mm.
03/14/06 – p – 12 mm.
10/19/07 – p – 15 mm.
5.09.08 – p – 15 mm.
5.05.09 – doubtful
05/19/10 – negative
3. DPT:
9.10.01 – 0.5 s 238-7
11/12/01 – 0.5 s 238-7
01/11/02 – 0.5 s 249-4
01/20/03 – 0.5 v/m from 271-2
13.05.08 – 0,5 ? 32-04
4. Poliomyelitis:
10/19/01 – 44 from 601
11/12/01 – 44 from 601
11.01.02 – 44 from 601
01/20/03 – 44s 644
5. Hepatitis:
11/12/01 – 0.5 s 04/04/01
01/11/02 – 0.5 s 04/03/01
06/11/02 – 0.5 s 04/16/02
6. Measles
10/11/02 – 0.5 p/c from 15
01/31/08 – 0.5 s 466
7. Mumps:
08/16/02 – 0.5 s 0840
01/31/08 – 0.5 s 404
8. Rubella:
08/16/02 – 0.5 s 251
09/26/06 – 0.5 s 404
9. Flu:
01.11.06 – 0.5 s 0806
11/12/07 – 0.5 s 0907
PAST ILLNESSES:
07/17/01 – physiological jaundice, erythema of newborns
9.10.01 – pyramidal insufficiency syndrome
11/14/01 – acute rhinitis
03/26/02 – reaction to teething
05/15/02 – acute respiratory infections, acute nasopharyngitis
06/23/03 – ORZ
07/24/03 – ARVI, nasopharyngitis
08/12/03 – nasopharyngitis
09/08/03 – ARVI, nasopharyngitis
04/14/04 - acute nasopharyngitis
05/06/04 – acute nasopharyngitis
06/23/04 – acute tracheobronchitis
06.23.04 – acute nasopharyngotracheitis, IDA – degree I
08/20/04 – acute pharyngitis
08/27/04 – nasopharyngitis
10/14/04 – bronchopneumonia
11/29/04 – acute nasopharyngitis
08/17/05 – ARVI
07/20/06 – acute pharyngitis
07/25/06 – acute nasopharyngitis
12/13/06 – acute rhinopharyngotracheitis
12/17/08 – acute nasopharyngobronchitis
09/16/10 – acute obstructive bronchitis, respiratory failure of the 1st degree
02.12.10 – acute bronchitis
01/25/11 – acute rhinopharyngotracheitis
05/04/12 – acute nasopharyngitis, acute bronchitis
05/14/12 – moderate acute obstructive bronchitis
FAMILY HISTORY:
Father– Prudnikov Vladislav Vyacheslavovich, born in 1978
Nationality Russian.
Occupation: assistant driver.
Mother– Prudnikova Irina Nikolaevna, born in 1978.
Russian nationality
Occupation: URMM – accountant.
The presence of occupational hazards and bad habits is denied. Parents and immediate family are healthy.
Family tree diagram:
There is no information about the patient's pedigree.
Conclusion:
1. There are no chromosomal diseases.
2. there is no significant burden of genealogical history. Allergy history: food – history of chicken. Medicinal, epidermal, household, pollen - none. There is no information about the presence of allergies in parents and relatives.
A new cat has recently been living in the house.
Material and living conditions :
The family lives in a two-room comfortable apartment. There is no information about monthly family income. The child is raised by his parents. Attends school, 5th grade, actively communicates with peers.
Daily regime:
07:00 - Wake up, morning toilet
07:15 – Breakfast
07:30 – 07:50 - Road to school
8:00 - School activities
12:00 – Lunch
14:00 – End of classes
14:10 – 14:30 – The way home
15:00 – Afternoon snack
15:30 – 17:00 – Free time
17:00 - Dinner
18:00 – Doing homework
21:00 - Watching TV shows, playing games
22:00 - Evening toilet, sleep
COMPREHENSIVE HEALTH ASSESSMENT:
‣‣‣ Genealogical ana mnez - there are no chromosomal diseases, there is no significant genetic history.
‣‣‣ Biological history- the antenatal period is burdened by maternal illness. The presence of one risk factor determines an insignificant burden of biological history - a low-risk group.
‣‣‣ Social history- father's age is 23 years, mother's age is 23 years. Parents' education: mother - secondary vocational (salesperson), information about father's education is missing. Parents' activities: father is an assistant driver, mother is on maternity leave. The family is complete. The psychological microclimate in the family is favorable. There is no information about the family's financial support. The sanitary and hygienic conditions for raising a child meet the requirements. Social history is not burdened.
PHYSICAL DEVELOPMENT ASSESSMENT (12 YEARS):
Height 139 cm (II corridor) - area of “low values”
Body mass 24.5 kg (I corridor) - area “area of very low values”
Chest circumference 57 cm (I corridor) - area “area of very low values”
Head circumference 49.3 cm (I corridor) - area of “very low values”
Somatotype: II+I+I=IV – microsomatotype.
Harmony: II-I=I - harmonious.
Conclusion: the main anthropometric parameters are in the area of “low” and “very low” values. FR - low, microsomatotype, harmonious development - (by height).
Neuropsychic development appropriate for age.
Functional status normal - indicators correspond to the age norm, behavior without deviations.
Adaptive capabilities of the child- the degree of adaptation is easy, there are no somatovegetative deviations.
There are no congenital defects.
Based on research and assessment of all health criteria, the child is classified as IV health group- children with chronic diseases in the subcompensation stage.
ANAMNESIS VITAE - concept and types. Classification and features of the category "ANAMNESIS VITAE" 2017, 2018.
Disease history
Clinical diagnosis:
Basic:
Related:
Curator: IV year student
Faculty of Pediatrics
Papandin A.A.
Start of supervision: 2.09.2013
End of supervision: 4.09.2013
Yaroslavl, 2013.
General information.
3. Gender: male.
5. Place of work: pensioner.
6. Position held: no.
Complaints at the time of supervision does not present.
Conclusion:
Conclusion
Life history of the patient (Anamnesis vitae).
Dolgopolov Vladimir Mikhailovich was born on September 15, 1940 in Kotlas in a family of workers. Considers material and living conditions during childhood and school years to be satisfactory. I went to school at the age of 6, studied satisfactorily, and completed 8 grades. After that, he served in the army in motorized rifle troops, but did not take part in hostilities. He began his working career at the age of 20. At this time, he considers material and living conditions to be satisfactory; he and his wife live in a comfortable two-room apartment in a brick building on the fourth floor.
Eats at home, regularly. He is on a diet, giving up sugar, fatty and salty foods.
He is not involved in sports or physical education. He does not smoke, drinks alcoholic beverages (vodka) about 100-200 ml once every 2-3 weeks. Doesn't take drugs. Denies childhood illnesses. People rarely get sick from ARVI. Surgeries performed: left testicular cyst, inguinal hernia. There were no blood transfusions. Denies sexually transmitted diseases, tuberculosis.
Heredity is not burdened. There is no allergic history.
Conclusion: 4 risk factors: age 73 years, alcohol abuse, male gender, diabetes.
Status praesens.
General inspection
At the time of supervision 09/02/2013.
The general condition is of moderate severity, active position, clear consciousness, calm facial expression, correct physique, normosthenic constitution.
Weight 77 kg. Height 165 cm. Body mass index 28.3 – tendency to obesity of the first degree.
Body temperature 36.5ºС.
Skin is pale
In the area of the inguinal fold there is a postoperative scar of a pale pink color, 5 mm wide, dense, mobile on palpation.
There are no visible tumors, scratches, abrasions, or hemorrhages.
Skin moisture is moderate, elasticity is reduced, tissue turgor is reduced.
Nails are of regular shape, not brittle, no striations. Graying of hair.
The mucous membranes of the lips, mouth, nose, and eyes are pink, clean, and moist.
Subcutaneous fat is pronounced, the thickness of the subcutaneous fat fold below the angle of the scapula is 2 cm. The greatest deposition of fat is observed on the abdomen. There is no pain on palpation, crepitus is not detected.
Lymph nodes: The submandibular lymph nodes are palpable, 0.5 cm in size, round in shape, elastic in consistency, mobile, not fused with surrounding tissues, painless. The skin over them is not changed. The remaining groups of lymph nodes (occipital, parotid, mental, cervical, supraclavicular, subclavian, axillary, ulnar, inguinal, popliteal) are not palpable.
The muscles are developed evenly, the muscle tone is reduced, the strength is sufficient. On palpation, the muscles are painless, there are no seals.
The shape of the bones of the skull, spine, and limbs is correct, there is no curvature of the spine. The symptom of “drum sticks” is not detected. There is no pain when tapping the sternum, ribs, tubular bones, or vertebrae. Thickening and unevenness of the periosteum, softening of the bones are not detected during palpation.
When examined, the joints have the correct configuration and there is no swelling. The skin over the joints is not changed. On palpation, the local temperature is not increased, there is no pain, and on tapping they are painless. Active and passive movements in the joints are free and in full range. There is no crunch.
Respiratory system.
Condition of the upper respiratory tract: Nasal breathing is free. The voice has not been changed. On palpation and percussion, the paranasal sinuses are painless. There is no feeling of dryness, no nosebleeds or discharge from the nose. There are no pathological changes in the larynx. The voice is preserved, there is no hoarseness.
Examination of the chest: The shape of the chest is normal, asymmetry, protrusion or recession of the supra and subclavian fossae is not determined. The width of the intercostal spaces is 1 cm, the direction of the ribs is moderately oblique. The shoulder blades fit tightly to the chest cage. The type of breathing is mixed, the movement of the chest is uniform. When breathing, the intercostal spaces do not change location and direction. NPV – 16 per minute. Breathing is of medium depth, rhythmic. No periodic breathing is noted. There is no shortness of breath.
Palpation of the chest: The chest is resistant, painless. Voice tremors are carried out moderately, equally on both sides. The pleural friction noise is not detected.
Percussion of the lungs: A clear pulmonary sound is noted over the entire percussed surface of the lungs, identical on both sides. No focal changes in percussion sound are detected.
Topographic percussion:
Height of the apex of the lungs in front and behind:
Lower border of the lungs:
Mobility of the lower pulmonary edges, cm
Auscultation of the lungs: When auscultating over the area of the larynx, trachea and behind to the level of the third thoracic vertebra, bronchial breathing is heard, over the entire remaining surface of the lungs vesicular breathing is determined, the same on both sides. Adverse respiratory sounds (wheezing, crepitus, pleural friction noise) are not heard. Brochnophony over symmetrical areas is not changed; slurred, unintelligible speech is heard equally on both sides.
Endocrine system.
On examination: the thyroid gland is not visualized. On palpation, the thyroid gland: not enlarged, normal consistency, painless and moderately mobile. Secondary sexual characteristics are expressed according to the male type, according to age and gender.
Preliminary diagnosis
Based on the patient's complaints: paroxysmal, intense pain of a compressive nature, occurring behind the sternum during normal walking on level ground at a distance of 1000 meters and when climbing to the 4th floor, radiating to the lower jaw, accompanied by pain, weakness, dizziness, darkening in the eyes (“floaters” before eyes) and passes on its own after 3-5 minutes.
History of the disease: Conclusion: symptoms characteristic of angina pectoris have been identified. Chronic course, because the first symptoms appeared 4 years ago. The patient considers himself sick for the last 4 years. Increased frequency of attacks.
Patient's life story
Conclusion: risk factors: Conclusion: risk factors: age 73 years, alcohol abuse, male gender, diabetes.
Objective research: Conclusion: blood pressure 150/90, accent of 1 tone at the apex, shift of the left border of relative cardiac dullness to the left (in the 5th intercostal space along the left midclavicular line)
I make a preliminary diagnosis:
Basic: IHD: stable angina pectoris, FC II
Hypertension stage III, degree 3, risk 4
Related: Type II diabetes in the stage of subcompensation.
Additional examination plan:
- clinical blood test every 7-10 days
- general urine test every 7-10 days
- stool test for helminth eggs and occult blood
- Wasserman reaction
- daily recording of blood pressure, heart rate, respiration
- fibrogastroduodenoscopy
- electrocardiography
- determination of blood group, Rh factor
- determination of lipoproteins, cholesterol, lecithin, cholesterol/lecithin ratio in blood serum upon admission and before discharge
- total protein and protein fractions of blood serum
- prothrombin index, blood clotting time, coagulogram, thromboelastogram on admission, repeated according to clinical indications
- dosed physical activity with examination of external respiration parameters, ECG
- rheography of peripheral vessels
- precordial rheography
- phase analysis of the cardiac cycle
- echocardiography
- blood leukocytes and ESR dynamics every 3-4 days after a painful attack
- biochemical blood test: determination of the activity of serum enzymes - aminotransferases - in the period from 12 to 48 hours after a painful attack, creatine phosphokinase - in the period 6-12 hours after an attack of pain, lactate dehydrogenase - from 2 to 5-7 days, lactate dehydrogenase isoenzymes (lactate dehydrogenase 1, lactate dehydrogenase 5) from 2 to 5 days
- ECG monitoring
- kinetocardiography
Differential diagnosis.
| Sign | Angina pectoris | THEM | Dissecting aortic aneurysm | TELA | Acute pericarditis | Left-sided pleurisy | Cervicothoracic radiculitis |
| Localization | Behind the sternum | Anterior surface of the chest | In the chest | In the chest | In the chest | In the chest | In the chest |
| Nature of pain | Compressive pressing | Dagger, sharp | paroxysmal | sharp | Constant, aching | Constant, compressive | shooting through |
| Pain intensity | strong | To the point of painful shock | To the point of painful shock | To the point of painful shock | strong | strong | strong |
| Duration of pain | Up to 15 min | More than 20 min | From a few minutes to a day | Several days | Several days | Several days | |
| Irradiation | left-handed | In all directions | Belly, neck, head | No irradiation | No irradiation | No irradiation | Belly, lower back |
| Pain relief | nitroglycerine | Morphine IV bolus | Resistance to narcotic analgesics | Morphine IV bolus | Analgesics, antibacterial therapy | NSAIDs | |
| Provocation | Breath | Cough | |||||
| Patient's appearance | Freezes, scared | Anxiety, pained look | Excited | Anxiety | Suffering look | anxiety | anxiety |
| Skin color | pale | Severe pallor, acrocyanosis | Cold, pale, cyanotic hands | cyanosis | ordinary | ordinary | ordinary |
| urinary system | polyuria | Polyuria and anuria | Oligoanuria | Oligoanuria | norm | norm | norm |
| Body temperature | norm | 37-38 ºС | 37-38 ºС | 37-38 ºС | norm | Very high numbers | norm |
| UAC | norm | Leukocytosis, increased ESR | Leukocytosis, increased ESR | Leukocytosis, increased ESR | Leukocytosis, increased ESR | Leukocytosis, increased ESR | inflammation |
| Cardio enzymes | norm | elevated | elevated | elevated | norm | norm | norm |
| C-reactive protein | norm | elevated | Doesn't change | Doesn't change | Doesn't change | Norm | norm |
| Lipid spectrum | Slightly elevated | elevated | norm | norm | Doesn't change | norm | norm |
| Coagulogram | Norm | Sharply increased | No changes | Sharply increased | Without changes | Norm | norm |
| ECG | Without pathology | Pat. Q, R T missing, ST below isoline | Decrease in ST and changes in T | C I Q II | ST segment elevation | norm | norm |
| Ultrasound of the heart | norm | hypokinesia | Aortic dissection | dilatation and asynergia of the right ventricle | widening of the precordial fissure behind the posterior wall of the left ventricle | norm | norm |
| Coronary angiography | Atherosclerotic plaques | Complete obliteration of the vessel | regurgitation of contrast material from the aorta into the left ventricle | Protrusion of the myocardial infarction towards the left ventricle | norm | norm | norm |
| R-gr | norm | norm | Expansion of the aortic shadow | High position of the dome of the diaphragm on the affected side, wedge-shaped shadow of the lungs | revealed an increase in the pulmonary pattern in the hilar regions on both sides | Fluid level in the pleura | signs of osteochondrosis |
Clinical diagnosis:
Based on complaints: paroxysmal, intense pain of a compressive nature, occurring behind the sternum during normal walking on level ground for a distance of 1000 meters and when climbing to the 4th floor, radiating to the lower jaw, accompanied by pain, weakness, dizziness, darkening in the eyes (flickering “spots” before the eyes) and goes away on its own after 3-5 minutes.
Based on the medical history: Symptoms characteristic of angina pectoris were identified, a chronic course, since the first symptoms appeared 4 years ago, and an increase in the frequency of attacks. The patient considers himself sick for the last 4 years.
Based on life history: Conclusion: 5 risk factors: age 73 years, alcohol abuse, male gender, diabetes.
Based on objective examination data: Blood pressure is 150/90, the first tone at the apex is weakened, a slight shift of the left border of relative cardiac dullness to the left (in the fifth intercostal space along the left midclavicular line).
Based on data from additional research methods :
BAC – hypercholesteremia,
ECG – sinus rhythm. Slowing of AV conduction. Shift of the heart axis to the left, cicatricial changes in the myocardium. Blockade of the left bundle branch. Echocardiography shows moderate dilatation of the cavity of the left atrium and right atrium. Compaction and expansion of the root Ao. Compaction of the valve leaflets with moderate degree of valve insufficiency. Mitral valve prolapse. Eccentric LV hypertrophy, increased LVMM. Violation of local contractility of the posterior, lower basal and middle segments. Global LV contractility is reduced. Moderate MCC hypertension.
as well as the differential diagnosis carried out with diseases such as myocardial infarction, pulmonary embolism, dissecting aortic aneurysm, acute pericarditis, left-sided dry pleurisy, left-sided cervicothoracic radiculitis, I make a clinical diagnosis:
basic IHD: stable angina pectoris, FC II, Post-infarction cardiosclerosis, Left bundle branch block, Incomplete AV block I degree
Hypertension stage III, degree 3, risk 4
accompanying: Type II diabetes
Etiology and pathogenesis.
In the development of coronary heart disease, an important role is played by risk factors, which are divided into modifiable (arterial hypertension, diabetes mellitus, dyslipidemia, obesity, smoking, predominance of animal fats and easily digestible carbohydrates in the diet, physical inactivity, psycho-emotional stress, long-term use of hormonal contraceptives in women) and non-modifiable (age, gender, family history).
The etiological basis of coronary heart disease are atherosclerosis and coronary spasm.
The pathogenesis is based on a discrepancy between the myocardial oxygen needs and the capabilities of its delivery. Myocardial oxygen demand increases with increasing heart rate, which may be associated with stress, physical exertion, and anemia. Delivery possibilities are determined by the patency of the vascular bed. In the early stages, spasm of the coronary arteries takes first place in the pathogenesis, which is caused by an increase in the activity of the sympatho-adrenal system, which is facilitated by neurohumoral disorders, increased production of catecholamines that excite α-adrenergic receptors, resulting in vascular spasm. At this stage, the process is reversible (dynamic obstruction).
In 95% of cases, coronary artery disease is based on atherosclerosis of the coronary vessels - this is a multi-stage, steadily progressing process.
The body secretes anti-atherogenic and pro-atherogenic factors.
Antiatherogenic include high-density lipoproteins (HDL), which have a strong connection between the lipid and the protein part; they are involved in the transfer of lipids from tissues to the liver.
Pro-atherogenic include low-density lipoproteins (LDL), which have a weak hydrogen bond between the protein and lipid parts; they are involved in the transfer of lipids from the liver to tissues.
In the case of hyperlipoproteinemia, there is an increase in the concentration of cholesterol in the membranes of endothelial cells, which leads to an increase in the permeability of the membrane to LDL.
When oxidized, LDL causes damage to the endothelium, which causes a powerful release of biologically active substances by endothelial cells. This further increases the permeability of the endothelium, which facilitates the penetration of oxidized LDL into the subendothelium, where they are captured by macrophages, which, overflowing with them, become foam cells, which gradually collapse into fatty stripes. Subsequently, the fatty strip is covered with a connective tissue covering, which then turns into a fibrous plaque. Further development follows the path of compaction of the tire; collagen fibers and smooth muscle tissue appear, and a true atherosclerotic plaque (atheroma) is formed.
Plaques can be smooth or loose.
The growth of a smooth plaque is slow, symptoms of angina pectoris appear when 2/3 of the lumen of the vessel is blocked. In the core of the plaque, proteolytic enzymes can be released that destroy the fibrous membrane, which leads to the appearance of a loose atherosclerotic plaque. Damage to the endothelium above it provokes the development of parietal thrombosis, which leads to a sharp narrowing of the lumen of the vessel and an exacerbation of symptoms. Thus, loose plaques are the substrate of unstable angina.
Calcium antagonists.
Does not improve prognosis except for verapamil with good left ventricular function.
Rp.: Verapamili 0.12
Da tales doses numero 30 in tabuletti.
Signa. 1 tablet 3 times a day.
Supervision diary.
| date | The patient's condition | Appointments |
| 02.09.13 | He makes no complaints. The general condition is satisfactory, consciousness is clear, position is active, facial expression is pained, body temperature is 36.5ºC. The skin of the face is pale, the lower extremities are pasty. Nasal breathing is free, breathing rate is 18 per minute, percussion sound is clear pulmonary over the entire area of the lungs, during auscultation vesicular breathing is heard over the entire area of the lungs, during auscultation of the heart - muffling of the first tone, the rhythm of tones is correct, pulse - 50 per minute, blood pressure – 140/90mmHg. On superficial palpation the abdomen is soft and painless. | |
| 03.09.13 | He makes no complaints. The general condition is satisfactory, consciousness is clear, position is active, facial expression is pained, body temperature is 36.7ºC. The skin of the face is pale, the lower extremities are pasty. Nasal breathing is free, breathing rate is 20 per minute, percussion sound is clear pulmonary over the entire area of the lungs, during auscultation vesicular breathing is heard over the entire area of the lungs, during auscultation of the heart - muffling of the first tone, the rhythm of tones is correct, pulse - 55 per minute, blood pressure – 145/90mmHg. On superficial palpation the abdomen is soft and painless. | General mode. Table No. 10. Rp: Tab Concor 2.5 N 10 Da.Signa: 1 tab in the morning Rp: Tab Atoris 0.2 N 10 Da.Signa: 1 tab in the evening, after meals Rp: Tab Cardiomagny l 75 N 10 Da.Signa : 1 tablet in the evening, after meals |
| 04.09.13 | He has no complaints. The general condition is satisfactory, consciousness is clear, position is active, facial expression is pained, body temperature is 36.5ºC. The skin of the face is pale, the lower extremities are pasty. Nasal breathing is free, breathing rate is 19 per minute, percussion sound is clear pulmonary over the entire area of the lungs, during auscultation vesicular breathing is heard over the entire area of the lungs, during auscultation of the heart - muffled sound of the first tone, the rhythm of tones is correct, pulse - 52 per minute, blood pressure – 140/90mmHg. On superficial palpation the abdomen is soft and painless. | General mode. Table No. 10. Rp: Tab Concor 2.5 N 10 Da.Signa: 1 tab in the morning Rp: Tab Atoris 0.2 N 10 Da.Signa: 1 tab in the evening, after meals Rp: Tab Cardiomagny l 75 N 10 Da.Signa : 1 tablet in the evening, after meals |
Epicrisis.
The patient Vladimir Mikhailovich Dolgopolov was admitted to the hospital on August 29, 2013 as planned. In the clinic, based on complaints, medical history, life history, objective examination data and additional examination methods, a clinical diagnosis was made:
basic: IHD: stable angina pectoris, FC II, Post-infarction cardiosclerosis, Left bundle branch block, Incomplete AV block I degree
Hypertension stage III, degree 3, risk 4
accompanying: Type II diabetes
The patient was treated: Concor 2.5 mg in the morning, Atoris 20 mg in the evening, after meals,
Cardiomagnyl 75 mg in the evening after meals.
By the time supervision ends, the patient continues treatment in the hospital.
Forecast.
Regarding life:
the nearest one is very doubtful;
distant – unfavorable, because there are complications - MI
Regarding the disease, it is unfavorable, since the disease is chronic and tends to steadily progress.
Regarding ability to work, it cannot be decided, since the patient is of retirement age.
Curator's signature
List of used literature.
- I.K. Novikova. A.I.Rudnichenko. Acute coronary syndromes.
Diagnosis and treatment at the prehospital and hospital stages.
Yaroslavl 2000, pp. 9-14.
- A.L. Syrkin. Myocardial infarction. Moscow. 1991, pp. 174-186.
- S.I. Ryabova. Internal illnesses. St. Petersburg. 2004, pp. 36-51, 254-259, 264-267.
- A.N.Inkova. Emergency cardiology. Rostov-on-Don. 2001, pp. 171, 263-268.
- M.D. Mashkovsky. Medicines. Moscow. 2002, volume 1 p. 147-154, 164-166, 377-384, 411-413, 421-422, volume 2 p. 149.
6. Materials of lectures on therapy.
Disease history
Dolgopolov Vladimir Mikhailovich, 73 years old.
Clinical diagnosis:
Basic: IHD: stable angina pectoris, FC II, Post-infarction cardiosclerosis, Left bundle branch block, Incomplete AV block I degree
Hypertension stage III, degree 3, risk 4
Related: Type II diabetes in the stage of subcompensation.
Curator: IV year student
Faculty of Pediatrics
Papandin A.A.
Start of supervision: 2.09.2013
End of supervision: 4.09.2013
Yaroslavl, 2013.
General information.
1. Full name: Dolgopolov Vladimir Mikhailovich.
2. Age: 09/15/1940, 73 years old.
3. Gender: male.
4. Education: secondary specialized.
5. Place of work: pensioner.
6. Position held: no.
7. Home address: Arkhangelsk region, Kotlas,
st. Severomorskaya, 5a, apt. 35.
8. Date of admission to the clinic: 09/29/2013
Patient complaints upon admission to the clinic:
Upon admission to the clinic, the patient complained of: paroxysmal, intense pain of a compressive nature, occurring behind the sternum during normal walking on level ground for a distance of 1000 meters and when climbing to the 4th floor, radiating to the lower jaw, accompanied by pain, weakness, dizziness , darkening in the eyes (flickering “flies” before the eyes) and passing on its own after 3-5 minutes.
Complaints at the time of supervision does not present.
Conclusion: These complaints indicate angina syndrome.
History of the present disease (Anamnesis morbi).
Considers himself sick since the age of 68, when attacks first appeared 3-4 years ago, associated with physical activity. I didn’t take any medications. The pain was relieved with rest. After 3 years, attacks appeared more often - once a month, after which he went to a paid clinic in Kotlas to see a cardiologist, who diagnosed him with ischemic heart disease: angina pectoris and prescribed him drugs such as simvastatin and amlodipine. There were fewer attacks. On August 27, I went independently to see a cardiologist at a local clinic with complaints such as paroxysmal, intense pain of a compressive nature, occurring behind the sternum during normal walking on level ground for a distance of 1000 meters and when climbing to the 4th floor, radiating to the lower jaw, from where he was sent to the Russian Railways hospital in Yaroslavl. During hospital treatment, the pain intensity decreased.
Conclusion: symptoms characteristic of angina pectoris have been identified. Chronic course, because the first symptoms appeared 4 years ago. The patient considers himself sick for the last 4 years. Increased frequency of attacks.
COMPLAINTS
At the time of supervision, the patient complained of pain in the area of the postoperative suture, weakness, and normal urination.
HISTORY OF THE PRESENT DISEASE
Anamnesis morbi/.
He considers himself sick since September, when the patient noticed an admixture of blood in his urine, then periodic pain began to appear in the right side, affecting the lower back and right half of the abdomen, and pain when urinating. The patient went to the clinic at her place of residence, where she was diagnosed with bladder cancer, after which the patient was sent to City Clinical Hospital No. 11 to clarify the diagnosis and further treatment. After further examination (carried out from November 7, 2006 to October 10, 2006), the clinical diagnosis did not change.
Anno naraptoy with a blurred vision in the left eye, weakness in the right hand, dizziness LIFE HISTORY OF THE PATIENT
Anamnesis vitae/.
Modest Pavlovich Saburov was born in Ryazan to healthy parents, his mother was 25 years old, his father was 31 years old, the second child in the family. Breastfed with mother's milk until one year of age. He developed along with his peers. I studied at school from the age of seven, graduated from 7 classes. Studying was easy.
Living conditions
Lives in his own house (50 m2), three people. Housing conditions are satisfactory. The room is dry, bright, clean.
Nutrition
He eats regularly, three times a day (morning, lunch, evening). Food is eaten hot. He takes most of his food in the evening and eats slowly. The diet contains fresh vegetables and fruits.
Family status
Married. Has a daughter.
Bad habits
Currently does not smoke. Doesn't drink alcohol regularly. Denies drug use and substance abuse.
Past illnesses
In childhood I suffered from acute respiratory infections, influenza, sore throat, rubella measles without complications. There is a history of diabetes mellitus, stage II. Over the past month, I have had no contact with infectious patients.
Allergy history
He denies hypersensitivity to medications and manifestations of allergic reactions to medications, food products, drinks, cosmetics, and contact with animals. My younger sister is allergic to pollen. Denies any previous allergic diseases.
bl., Chuchkovsky district, village. and I
puppy.ena.
voznik chronic gastritis. ruffle wall. PRESENT CONDITION OF THE PATIENT
/Status praesens/
At the time of the examination, the general condition is satisfactory, the patient’s position is active, consciousness is clear, adequate, oriented in space and time. The face is calm. The chest is normosthenic, the physique is proportional. Height 165 cm, weight 83 cm. At the time of supervision, body temperature is normal (36.6ºC).
The skin is of normal color. The fingers are warm. The elasticity and moisture of the skin are normal. There are no rashes, ulcers, spider veins, hemorrhages, spots, erythema, blisters, erosions, or nodules. There are no visible tumors. Skin turgor is normal. Hair growth is uniform according to the male type. The nails are round, unbreakable, pink in color, and there is no tremor of the fingers.
Visible mucous membranes are moist, pink, without rashes, blisters, or erosions.
Subcutaneous tissue is developed moderately and evenly. There is no pain on palpation. There is no peripheral edema.
The occipital, parotid, chin, cervical, supraclavicular, subclavian, ulnar, femoral, and popliteal lymph nodes are not palpable. The submandibular (oval-shaped, the size of a lentil, elastic consistency, mobile, painless, the skin over them is in normal condition), axillary and inguinal lymph nodes the size of a pea, painless, mobile, not fused to each other or to the surrounding tissues are palpated. The color of the skin over the lymph nodes is normal.
The general development of the muscular system is satisfactory, the muscles are evenly developed. Muscle strength in the arms and legs is normal. The cuts are coordinated. On palpation, no pain, tightness in the muscles, or local hypertrophy are observed.
The shape of the bones of the skull, spine and limbs is correct. No pain was detected on palpation of the sternum, ribs, tubular bones, vertebrae, or pelvic bones.
The color of the skin and its temperature in the joint area are normal. The joint configuration is correct; active and passive movements are free, painless, and fully preserved. The volume of symmetrical joints is the same. The symptom of “floating ice” when pressing on the patella is negative.
This section describes in detail, in chronological order, the occurrence, course and development of the present disease. from its first manifestations to the moment of examination by the curator.
Suggested question scheme:
How long has he considered himself sick?
Where and under what circumstances did you first get sick?
Factors that contributed to the onset of the disease?
What signs did the disease begin with?
The first visit to the doctor, the results of studies carried out that have diagnostic significance, the diagnosis of the disease, medical and medical care during that period, its effectiveness.
Subsequent course of the disease:
a) the dynamics of initial symptoms, the appearance of new symptoms and the further development of all signs of the disease;
b) frequency of exacerbations, duration of remissions, complications of the disease;
c) the therapeutic and diagnostic measures used (inpatient or outpatient examination and treatment, medications, physiotherapy, spa treatment and other methods), the effectiveness of the therapy;
d) ability to work during the period of illness.
A detailed description of the current exacerbation of the disease that forced the patient to see a doctor.
Study the documents available to the patient that characterize the course of the disease before admission to the clinic (outpatient card, certificates, extracts, etc.) and record their data in the medical history.
Life history (anamnesis vitae).
Brief biographical information: year and place of birth, what family he was born into, what kind of child he was, how he grew up and developed. Education.
Period of childhood and adolescence: how he grew and developed, health.
Work, profession: at what age did you start working? Was there a change in work due to any illness, indicate length of service, working conditions (find out the presence of harmful aspects in work: forced, abnormal body position, dust and noise in the workshop, high temperature, industrial intoxications).
Military service: length of stay in the army, participation in combat operations, discharged on time or due to illness.
Housing: hostel, apartment, occupies a corner, sanitary and hygienic conditions.
Cloth: how to dress, warm or light, clothes in winter, shoes, hypothermia.
Nutrition: meals in the canteen or at home. Does he follow a diet? Body hygiene: does he wash his hands before eating, does he brush his teeth, how often does he wash in the bathhouse.
Family status: married, single. Lives with a family or alone.
Family history: the health status of the parents, paying attention to tuberculosis, sexually transmitted diseases, neoplasms, metabolic diseases, mental illness, alcoholism and others. If relatives died, at what age, cause of death
Past illnesses: all diseases, operations, wounds, injuries, concussions are stated in chronological order, indicating the date, duration and severity of these diseases, injuries and their complications and the treatment provided. Particularly mention past infectious diseases, sexually transmitted diseases, tuberculosis, jaundice. Note whether blood or blood substitutes have been transfused before and whether there have been any reactions to the transfusion. Indicate whether parenteral medications have been administered within the last 6 months. A gynecological history is collected from women: presence, regularity of menstruation, number of pregnancies, births, children.
Habitual intoxications: alcohol abuse: how often does he drink (daily, periodically, casually, at lunch, in company), what quantity, since when. Smokes - how many cigarettes or cigarettes does he smoke per day, does he use drugs, how often.
Allergic history: intolerance to foods, various medications, vaccines and serums. The presence of allergic reactions: causes, seasonality, how they manifest themselves.
Disability(from what age, reason, disability group).