Consequences, signs and methods of treatment of subarachnoid cerebral hemorrhage. Subarachnoid cerebral hemorrhage: symptoms, choice of treatment tactics and consequences What is subarachnoid cerebral hemorrhage
Subarachnoid hemorrhage is a diagnosis that plunges into shock both the patient suffering from such an illness and his friends and relatives. Like any pathological process in the brain, the disease has an etiology that is dangerous to human health and can threaten not only loss of capacity, but also death.
In this article we will talk about the features of the disease, its root causes and symptoms, knowledge of which will help you seek medical help in time, and also consider the specifics of diagnosis, treatment and rehabilitation of the disease, and effective ways to prevent it.
Features of the disease
To understand what subarachnoid cerebral hemorrhage is, a short excursion into physiology, namely into the structure of the hemispheres, will help. Physiologically, the meninges consist of three balls:
- external, solid configuration;
- medium, spider type;
- internal, which is the vascular cover.
There is space between all the balls: the area between the first two balls is called subdural, and the area between the choroid and tunica media is called subarachnoid.
In a normal state, all membranes have an integral structure, which ensures protection of the hemispheres and normal brain activity. A case in which, due to difficulties in blood circulation, vascular spasms or traumatic events, an outpouring of blood occurs in the subarachnoid zone is identified as subarachnoid. Subarachnoid hemorrhage, abbreviated as SAH, may also be referred to as intracranial hemorrhage or stroke.
Hemorrhage of the subarachnoid type is often characterized by spontaneity, occurs against the background of a segmental or large-scale rupture of cerebral blood lines, and is accompanied by sharp and intense headaches, bouts of vomiting, and loss of consciousness. This is a very dangerous condition, often causing sudden death for the patient, and the chances of saving a person directly depend on the promptness of first aid and the intensity of blood filling in the subarachnoid zone.

Causes of effusion
Help for the progression of pathology is a violation of the tightness of the walls of the vascular highways of the hemispheres. The causes of subarachnoid hemorrhage can have different etiologies, mainly the following:
- Complex head injuries, which are accompanied by traumatic brain injuries, brain contusions or direct rupture of arteries in the hemispheres.
- An unexpected rupture of the artery wall, which can be caused by infectious diseases, a rapid increase in pressure, or may also occur due to the use of alcoholic beverages or drugs.
- Vascular malformation deformity.
Symptoms of pathology
Often, the progression of the pathology begins to make itself felt to a person with unpleasant symptoms, with its etiology of a neuralgic nature, several days before the onset of a massive outpouring. During this period, a characteristic feature is the thinning of the vessel wall, through which blood begins to leak in small volumes. This condition is accompanied by nausea and dizziness, visual impairment. In the absence of timely diagnosis and adequate treatment, the disease progresses, one or more vessels rupture, and blood begins to intensively fill the subarachnoid segments of the brain. Similar symptoms may be accompanied by traumatic subarachnoid hemorrhage if the head injury is not particularly intense.
Symptoms of extensive bleeding are pronounced, accompanied by sharp, explosive, diffuse pain in the head, followed by irradiation to the shoulders, neck and occipital region. Subarachnoid hemorrhage in the brain of a progressive type is often accompanied by nausea with bouts of vomiting, photophobia, disturbances of consciousness, often with fainting precedents and coma. The period from the onset of massive effusion to coma can range from several minutes to half a day.
In newborns, subarachnoid hemorrhage is predominantly a consequence of trauma during childbirth and is characterized by the formation of hematomas in the hemispheres. Cerebral hemorrhage in newborns is accompanied by the following symptoms:
- shrill, intense crying of a child against the background of increased physical activity;
- convulsive attacks;
- lack of sleep;
- involuntary eye movement, visual strabismus;
- extreme severity of innate reflexes;
- increased muscle tone;
- convexity of the fontanel with intense pulsation;
- jaundiced body color.

Symptoms of the pathology in a newborn can appear either immediately after birth or within several days, depending on the scale of the effusion in the hemispheres. If the problem is identified in a timely manner, modern medicine allows the child to be resuscitated, in most cases without negative consequences for his future life.
Prevalence of the disease and stages of its progression
Precedents associated with SAH of the brain are a fairly common phenomenon. According to statistics, the most common cases are considered to be cases of subarachnoid effusion due to trauma, accounting for about sixty percent of all cases.
Less common are precedents for the development of pathology due to changes in blood circulation in the cerebral vessels, diagnosed in seven percent of patients with this pathology. Most often these are patients of advanced and retirement age, as well as people with alcohol or drug addiction. The rarest cases are cases of spontaneous progression of the disease, their prevalence is less than one percent.
As for the etiology of the disease, the most common situations in medical practice are the occurrence of SAH due to rupture of arteries located in the circle of Visilli. Such precedents account for about eighty-five percent of all registered cases, half of them end in death, while fifteen percent of patients do not even have time to get to a medical facility.
Cerebral hemorrhage is a disease that most often affects the adult population, however, the pediatric category is no exception. In children, this pathology often occurs due to trauma. Subarachnoid hemorrhage in newborns can be the result of a prolonged or too rapid natural labor, when there is a mismatch between the mother’s birth canal and the baby’s head, as well as a consequence of the baby being without oxygen for a long time. The progression of pathology in a child can be provoked by infectious diseases of the mother, pathologies of brain activity in a child of the congenital category, and fetal hypoxia.

Medicine classifies SAH of traumatic origin into three stages of development:
- Progression of intracranial hypertension against the background of mixing of gushing blood with cerebrospinal fluid, increasing the latter in volume.
- An increase in hemispheric hypertension to extreme maximums, due to the formation of blood clots in the cerebrospinal fluid channels, their blocking and disturbances in the circulation of cerebrospinal fluid.
- Dissolution of blood clots, followed by intensification of inflammatory processes in the hemispheres.
Classification of disease severity
To assess the severity of a patient’s condition, medical specialists use three methodologies for ranking the course of pathology.
Most often in practice, the Hunt-Hess scale is used to categorize the patient’s condition, which has five degrees of damage to the human brain:
- The first degree of the disease is considered the least life-threatening if therapy is started in a timely manner, and is characterized by a high percentage of patient survival. At this stage, the disease is asymptomatic with minor headaches and the onset of stiffness of the neck muscles.
- The second degree of the disease is characterized by a distinct loss of mobility of the occipital muscles, intense headaches, and paresis of the nerves of the hemispheres. The prospects for a favorable outcome do not exceed sixty percent.
- The third degree of the disease manifests itself in a person as a moderate deficiency of the neuralgic category, stunning. The patient's chance of survival does not exceed fifty percent.
- The fourth level of pathology is characterized by the patient’s frozen state, and a first-degree coma may occur. Typical for this stage are failures of the autonomic system and severe hemiparesis. Chances of life are about twenty percent.
- Last degree of progression: second or third level coma. The prognosis for the patient is disappointing, survival rate is no more than ten percent.
The second, no less popular in medical practice for assessing a patient’s condition, is the Fisher gradation, which is based on the results of computed tomography:
- If a CT examination does not visually detect bleeding, the disease is assigned the first degree of severity.
- The second stage is assigned to pathology if the scale of the effusion does not exceed one millimeter in thickness.
- If the lesion is more than one millimeter in size, the third level of pathology progression is diagnosed.
- When blood spreads inside the ventricles and in the parenchyma, the fourth degree of progression of SAH is diagnosed.

The SAH severity scale according to the World Federation of Neurosurgeons ranks the disease as follows:
- The first stage is fifteen points on the GCS, no neurological deficit.
- The second level is from thirteen to fourteen points, with the absence of neurological impairment.
- Third level – scores are similar to the previous version, with signs of disorders in the nervous and peripheral systems.
- The fourth stage of progression is assigned from seven to twelve points on the Glasgow Coma Scale.
- The last stage of the disease: less than seven points were diagnosed according to the GCS.
Diagnosis of pathology
Subarachnoid hemorrhage belongs to the category of the most complex and life-threatening cases. Its diagnosis involves conducting a complex of hardware examinations of the patient in order to confirm the diagnosis, as well as determine the stage of development, localization of hemorrhage, and the degree of disorders in the vascular system and hemispheres.
The main examination procedures include:
- Initial examination of the patient, analysis of his complaints.
- Visual assessment of a person’s condition, monitoring of his consciousness and the presence of neurological abnormalities.
- A laboratory blood test that can be used to determine the criteria for blood clotting.
- Cerebrospinal fluid puncture. If about twelve hours have passed since the onset of hemorrhage, its results, namely the presence of blood in the cerebrospinal fluid, can confirm the progression of SAH.
- or computed tomography allows you to identify the presence and location of the effusion, as well as assess the general condition of the brain. CT is more informative in the situation with SAH, which is why this type of examination is often prescribed to patients.
- If there is a suspicion of brain displacement as a result of injury, echoencephalography is prescribed to confirm or refute this fact.
- Transcranial Doppler ultrasound is performed to monitor the quality of blood flow in the cerebral arteries and its deterioration as a result of narrowing of the blood vessels.
- Magnetic resonance angiography of the arteries helps to assess their integrity and patency.

Based on the results of the study, the patient will be diagnosed in accordance with the International Classification of Diseases, Tenth Revision. SAH is classified in the section “Diseases of the circulatory system,” a subgroup of cerebrovascular diseases, and may have an ICD-10 code from I160.0 to I160.9, depending on the location of the source of the effusion.
Treatment methods
The methodology for treating pathology involves both drug treatment and surgical intervention, depending on the stage of the disease and its complexity. The feasibility of therapy and its direction can only be determined by a qualified specialist solely on the basis of diagnostic results. Primary measures should be focused on stopping bleeding, stabilizing, preventing or reducing the volume of brain swelling.
First aid
First aid for subarachnoid hemorrhage does not provide for any specific procedures; it consists of immediately calling an ambulance. It is strictly forbidden to give the patient any medications to eliminate symptoms, as this can cause unpredictable consequences.
If a sick person has an epileptic seizure, you must try to create comfortable conditions for him by placing soft things under his head and other parts of the body. After the seizure ends, you need to lay the sick person on his side, try to fix his limbs and wait for the ambulance to arrive.
When a person is unconscious as a result of cardiac arrest, it is necessary to perform cardiopulmonary resuscitation, with the proportion of chest compressions to breaths being thirty to two.
When there is an outpouring into the hemispheres, the only rational help for the patient is his hospitalization as soon as possible. All restorative and therapeutic procedures are subsequently carried out exclusively under the guidance of specialists, based on the results of diagnosing the patient’s condition.
Drug treatment
Conservative therapy can be used in situations where there are no indicators for surgical intervention, as well as to normalize the patient’s condition in the preoperative and postoperative period.
The main objectives of drug treatment of subarachnoid hemorrhage are:
- achieving stability of the patient's condition;
- prevention of relapses;
- stabilization of homeostasis;
- eliminating the original source of the outpouring;
- carrying out treatment and preventive measures aimed at prevention.
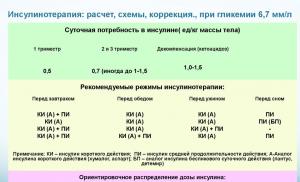
Depending on the complexity of the disease and its manifestations, the patient may be prescribed the following medications:

The appropriateness, dosage and duration of taking medications are determined exclusively by the attending physician and are based on medical indicators. During the treatment process, the doctor monitors the dynamics and can change the quantitative and qualitative composition of the drugs if there are no positive results.
Surgery
Surgical intervention is often prescribed by medicine for existing intracranial hematomas of significant size or when SAH occurs as a result of a serious head injury. In a situation where the patient experiences massive bleeding, emergency surgical procedures are performed. In other cases, the timing of the operation may vary and depend on the condition and age of the patient, the volume of effusion and the complexity of the symptoms.
Medicine provides the following types of surgical intervention for subarachnoid effusion:
- Removal of hemorrhagic contents by inserting a syringe or a specific needle.
- Elimination of hematoma with opening of the skull.
- Laser coagulation of blood vessels, if the effusion cannot be stopped with medications, sometimes with the application of specific clips to the damaged areas of the artery.
After surgery, the patient will have to undergo a mandatory course of drug therapy.
Rehabilitation procedures
Measures to restore the patient after subarachnoid hemorrhage are a mandatory continuation of therapy in the postoperative period. Depending on the complexity of the illness suffered, rehabilitation can last from six months to several years and has a complex structure.
After the incident, it is important for the patient to completely abandon bad habits, try to avoid stressful situations and maintain a healthy lifestyle. In addition, during the rehabilitation period, medicine provides for the use of medications, the action of which is aimed at preventing relapses.
Rehabilitation of the patient, depending on the severity of the illness experienced, may include the following areas:
- specific massages and hardware procedures to restore the patient’s muscle and motor activity;
- health treatments in special centers;
- therapeutic exercises to restore walking and coordination skills;
- classes with a psychologist to restore the patient’s psycho-emotional state.

During the recovery process at home, the patient will need proper care, as well as the support of loved ones.
Prognosis and possible complications
Subarachnoid cerebral hemorrhage is an insidious disease that very rarely goes away without a trace for a person. The most harmless complications are in the form of frequent migraines and disturbances in hormonal regulation of the body. Additionally, after experiencing an illness, the patient may experience a deterioration in brain activity, manifested in the form of psycho-emotional disorders, deterioration of attention and memory. However, such manifestations of the body after SAH are not considered particularly dangerous. Dangerous consequences include:
- vasospasm, which often provokes ischemic processes in the hemispheres;
- delayed ischemia, which affects more than a third of all patients, entails irreversible brain starvation with all the ensuing consequences;
- recurrent exacerbation of pathology;
- hydrocephalus;
- Rare complications include pulmonary edema and heart attacks.
The chances of a patient’s recovery after SAH depend on many factors, such as the person’s general physical health, his age, the stage of the disease and the extent of the effusion, and the promptness of first aid.
Often, it is a belated visit to a medical institution against the backdrop of a heavy outpouring that causes death for the patient or serious complications that do not allow the person to return his life to normal.
Preventive measures
Prevention of SAH, like many other diseases of the cardiovascular system, is not particularly difficult. The main rule, the observance of which helps to prevent cerebral hemorrhage, in addition to precedents with injuries, is a healthy lifestyle. A balanced diet, giving up bad habits, regular walks in the fresh air and moderate physical activity to keep the body in excellent condition, timely treatment of problems with blood vessels and heart under the supervision of doctors are the primary and effective preventive measures against the development of SAH and other complex ailments.
If a person has prerequisites for the development of SAH caused by cardiac problems, it is worth undergoing regular examinations, taking preventive medications prescribed by doctors as necessary to normalize blood pressure and heart rate, and monitor the state of one’s health.
In this case, careful attention to your body and a correct lifestyle are the most important preventive measures that help to avoid a complex and life-threatening incident.
Let's sum it up
Subarachnoid hemorrhage belongs to the category of the most dangerous diseases, which very often cause death. Of course, it is better to prevent such situations, however, if such a precedent occurs, it is worthwhile to immediately deliver the patient to a medical facility: a person’s life depends on the speed of diagnosis and provision of correct assistance.
Lead a full, healthy and correct lifestyle - this will help you avoid many health problems, is the key to the proper functioning of the body, and reduces the risk of developing not only SAH, but also other diseases.
19446 0
Subarachnoid hemorrhages include the accumulation of blood and/or blood clots in the subarachnoid space resulting from trauma, causing disturbances in the circulation and resorption of cerebrospinal fluid, vasospasm, irritation of the soft meninges and cerebral cortex.
EPIDEMIOLOGY
Traumatic subarachnoid hemorrhage (TSAH) is the most common type of intracranial hemorrhage. Previously, this was evidenced by data from large series of autopsies. Currently, the prevalence of (TSAC) is confirmed by brain neuroimaging methods. N.M. Eisenberg et al. Based on the analysis of primary CT data in 753 patients with severe TBI, the presence of TSAC was revealed in 39% of victims. A. Kakarieka. et al. Based on materials from a European multicenter study (819 patients), CT signs of TSAC were found in more than 32% of patients with severe TBI. TSAC turned out to be the most common pathology on CT according to J.S. Jeret et al. in a series of 712 observations of patients with moderate TBI. N. Fukuda et al., in a group of 123 patients with severe diffuse brain injury, TSAC was diagnosed in the first 24 hours by CT scan in 99 patients. The frequency of observations of TSAC according to CT data varies widely from 8% to 59%.
Age factors in TSAH are not decisive, but there is a tendency for the frequency of hemorrhages to increase with the age of the victims.
Alcohol intoxication increases the risk of TSAC.
MECHANISMS OF EDUCATION
TSAC is considered as a result of direct damage to vessels located in the subarachnoid space (arterial or venous branches, smallest pial arteries), covering the entire surface of the brain. The blood poured into the subarachnoid space spreads through the cerebrospinal fluid channels, subarachnoid cells, and cisterns. In this case, a significant amount of shed blood is removed with cerebrospinal fluid flowing from the subarachnoid space.
In some cases, TSAC is caused by arterial bleeding in areas of massive brain contusions.
Another trigger for TSA may be a complex of severe vasomotor disturbances accompanying the course of TBI.
PATHOGENESIS AND PATHOMORPHOLOGY
Hemorrhage developing in the subarachnoid space affects, first of all, the arachnoid and pia (vascular) membranes, the structures of the subarachnoid space, and advetitia of the arteries. Features of the localization and course of TSAC are primarily associated with the development of pathology of the cerebrospinal fluid circulation system. Pathomorphological changes associated with the presence of blood in the subarachnoid space depend not only on the time since the injury, but also on the massiveness of the TSAC. There are morphological types of TSAC with disruption and preservation of the pia mater. Disturbances of the leptomeninges in TSAH can have a tearing and erosive appearance. Rupture injuries of the soft meninges occur only at the site of fractures of the skull bones, accompanied by ruptures of the dura mater. Erosive injuries are more often observed with acceleration trauma and compression of the head. When the membrane is intact, spotty and limitedly diffuse TSACs are observed. They are usually located at the site of impact or on the opposite side, usually of small size. Diffuse TSAC can spread over the entire surface of both hemispheres, the surface of the cerebellum and fill the cisterns of the base of the brain with blood.
Reactive changes in the meninges in response to shed blood develop within 1-4 hours - a concentration of polymorphic leukocytes around the blood vessels is noted, followed by their infiltration of the pia mater within 4-16 hours. In the next 16-32 hours, the number of leukocytes and lymphocytes increases, and phagocytosis phenomena are observed. The polymorphocellular reaction reaches its greatest development on the third day with a predominance of leukocytes and increasing phagocytosis. The passage of erythrocytes through the arachnoid membrane is accompanied by the expansion of intercellular spaces with the destruction of demosomes and the reaction of arachnoid cells. The varied shape and plasticity of erythrocytes facilitates their penetration through the cellular layers of the arachnoid membrane, promoting its loosening and deformation.
Ultrastructural changes in the pia mater reveal disturbances in the outer endothelial layer facing the subarachnoid space, loosening of the collagen-fibrous base of the shell, loosening of microfibrils of the osmiophilic component of the basement membrane at the border with the brain. Disturbances in the morphological substrate of the pia mater lead to disruptions in the cerebrospinal fluid barrier. Thus, the removal of blood components from the subarachnoid space is accompanied by disturbances in the ultrastructure of the morphological substrates of the barriers between the cerebrospinal fluid and the environments and tissues bordering them.
By 8-10 days, signs of the organization of TSAC with signs of fibrosis of the soft meninges are detected. Fixation of blood elements in the protective-trophic system of the subarachnoid space contributes to the loading of the pia mater with the products of their decay. Their accumulation is a kind of irritant that causes the development of chronic aseptic leptomeningitis, an adhesive process in the subarachnoid space with subsequent disturbances in the circulation of the cerebrospinal fluid, which, in turn, leads to the development of hydrocephalus.
The course of TSAC reflects three sequential stages:
1) blood poured into the subarachnoid space spreads from the site of hemorrhage along the systems of liquor-carrying canals, reaching the excretory canals at the apexes of the convolutions, while simultaneously penetrating through the holes in the walls of the canals into the subarachnoid cells. The appearance of blood in the subarachnoid space leads to an increase in the volume of cerebrospinal fluid with subsequent acute cerebrospinal fluid hypertension. An increase in cerebrospinal fluid pressure increases the outflow of cerebrospinal fluid from the subarachnoid space. From the moment of injury, in the first hours and days, there is an intensive removal of erythrocytes and other blood components from the cerebrospinal fluid outside the subarachnoid space, which contributes to partial sanitation of the cerebrospinal fluid;
2) blood coagulation in the cerebrospinal fluid with the formation of clots. It has been established that blood coagulates into liquor at a dilution of 1:100 or more. Under these conditions, blood clots form in the subarachnoid space, leading to partial or complete blockade of individual or several cisterns and cerebrospinal fluid channels. These disturbances entail further disturbances of the liquor circulation, with increasing liquor hypertension. At the same time, there are disturbances in the outflow of cerebrospinal fluid outside the subarachnoid space in the excretory canals of the leptomeninges. This, in turn, leads to disruption of the process of removing blood components from the subarachnoid space. The forming bundles are located mainly in the systems of cisterns and liquor-carrying channels, in places of interweaving of paravasal structures. During the process of blood clotting, some platelets disintegrate with the release of serotonin, which has a pronounced vasoconstrictor effect. In the system of subarachnoid cells, blood cells are also retained and fixed. Starting from 2-3 days, phagocytosis of blood clot components by arachnoid cells and macrophages begins, which contributes to the sanitization of the cerebrospinal fluid and the normalization of its composition;
3) lysis of blood clots due to the fibrinolytic activity of arachnoid cells everywhere lining the subarachnoid space. Lysis of clots leads to a gradual complete or partial restoration of cerebrospinal fluid circulation and resorption of cerebrospinal fluid. The degree of these disorders depends to a certain extent on the massiveness of the TSAC.
Thus, ideas about sanitation of cerebrospinal fluid during TSAH suggest the following mechanisms of cerebrospinal fluid purification: 1. Removal of spilled blood with flowing cerebrospinal fluid outside the subarachnoid space; 2. Fixation of blood elements in the protective-trophic system of the pia mater.
Blood spilled into the subarachnoid space, according to angiography, in 5%-41% of cases is accompanied by the development of vascular spasm. Transcranial Dopplerography, which determines vasospasm, with a linear cerebral blood flow velocity exceeding >120 cm/sec, is observed in 27-50% of victims with TBI. Vasospasm is based on a whole complex of reasons: mechanical factors, the effects of hemolysis and fibrinolysis products of blood cells and blood clots, imbalance of calcium, prostaglandins, their derivatives and other biochemical disorders. Vasospasm is one of the main causes of the development of secondary ischemic neurological disorders in patients with ASCA and is a prognostically unfavorable factor in the course of the acute period of TBI.
CLINIC
The clinical picture of TSAC is characterized by a combination of cerebral, meningeal and focal neurological symptoms. Victims with TSAC experience intense headaches. They are often of a shell nature, predominantly localized in the forehead, brow ridges and back of the head. According to G.E. Pedachenko, 47% of patients with TSAC are diagnosed with cerebellar tentorium syndrome. Headaches are aggravated by head movement, tension and percussion of the skull. Dizziness, nausea, vomiting, and autonomic disorders are often combined with headaches. The latter are manifested by sweating, coldness of the extremities, paleness of the skin, a decrease in previously elevated temperature, and fluctuations in blood pressure.
General cerebral symptoms are often accompanied by psychopathological symptoms in the form of psychomotor agitation, disorientation and
confusion. Depression of consciousness manifests itself in the form of moderate and/or deep stupor, stupor lasting up to 3-7 days. Restoration of consciousness usually occurs against the background of asthenovegetative syndrome and memory impairments observed for a long time after TBI, often in the form of retro and anterograde amnesia, Korsakoff syndrome, etc. The severity of memory changes depends on the severity of TBI.
The characteristic clinical manifestations of TSAC include meningeal symptoms. Its development is associated with irritation of the meninges by shed blood and its decay products. Monsingal symptoms (photophobia, painful restriction of movements of the eyeballs, stiff neck, Kernig's, Brudzinski's symptoms, etc.) are detected in most patients. The severity of clinical signs of meningeal irritation often reflects the massiveness of TSAC. Meningeal symptoms usually increase during the first few days after TBI. Regression of meningeal symptoms occurs at a later date compared to the sanitation of the cerebrospinal fluid, on days 14-21 with a favorable course of TBI.
Symptoms of focal brain damage in TSAC are varied and can be caused by irritation of the cortical parts of the brain, accumulation of blood outside the areas of injury, and brain damage. Thus, with localized TSAC, focal symptoms can manifest as mild insufficiency of the VII and XII cranial nerves of the central type, anisoreflexia, and mild pyramidal insufficiency. With massive TSCA, focal neurological symptoms can be clear and persistent, and their severity depends on the extent and localization of brain damage.
One of the features of the course of TSAC is disturbances in thermoregulation. Significant fluctuations in body temperature within 1-2 weeks are often observed.
DIAGNOSTICS
Direct visualization of TSC is available using CT (Fig. 14-1; see also Fig. 27-9). A sign of TSAC is an increase in density in the area of the basal cisterns, lateral fissure and subarachnoid spaces. An admixture of blood in cerebrospinal fluid is detected on CT if its concentration is high enough to increase the coefficient of cerebrospinal fluid adsorption. The most clear CT verification
Rice. 14-1. CT. 1 day after moderate TBI: A - subarachnoid hemorrhage localized in the basal cisterns (interpeduncular, surrounding cisterns); B - subarachnoid hemorrhage localized in the left lateral and interhemispheric fissures
TSAC is possible only in the early period. According to A. Kakarieka, signs of TSAC on primary CT scans (average time 4 hours after TBI) are detected in 33% of victims. At the same time, TSACs are most often visualized in the area of the convexital surface of the brain (in 70%), subarachnoid sheli (in 53%), and less often in the area of the basal cisterns (in 33%). CT assessment of the massiveness of TSAC is also possible, determined by a scoring system reflecting the distribution of blood in the liquor-containing spaces. The severity of TSAC decreases by 50% when repeat CT is performed within the first two days after TBI and on the third day is only one third of its assessment in the first hours. Visualization of the dynamics of TSAC emphasizes the need for early CT after TBI for the purpose of its verification. The limitations of CT in determining TSAC are most often due to the low resolution of the equipment and the time parameters of the study.
The effectiveness of MTP in the diagnosis of acute TSAC is controversial. The admixture of blood in the cerebrospinal fluid very slightly increases the signal on tomograms in T1 mode and minimally decreases it in T2 mode. MRI is much more accurate than CT in detecting TSAC in the subacute and chronic stages, when blood or even traces of it, due to the presence of methemoglobin, play the role of natural contrast and provide a high signal on T1 and T2 tomograms (superficial siderosis).
Routine diagnosis of TSAC is based on the results of a lumbar puncture, which reveals the presence of bloody coloration of the cerebrospinal fluid. This sign confirms the fact of TSAC, of course, with the exception of situations associated with travel blood. An additional sign of TSAH is also xanthochromia of the cerebrospinal fluid, caused by hemolysis, and observed in 10% of cases already on the first day after TBI. It reaches its greatest intensity on days 3-5 and is observed within 1-3 weeks after TBI. CSF pleocytosis, as a reaction to escaping blood, usually with a predominance of neutrophils, constantly accompanies the course of TSAC. The severity of its manifestations is varied and is associated with the individual reactivity of the membranes of the brain. A characteristic cerebrospinal fluid test for TSAH is a change in the protein composition of the cerebrospinal fluid, caused not only by the intake of blood, but also by dysgemic disorders.
The severity of TSA often reflects the severity of TBI. Thus, with mild brain contusions, the number of red blood cells in 1 mm3 of cerebrospinal fluid can range from several hundred to 8-10 thousand; for moderate brain contusions from several tens of thousands to 100-200 thousand higher; with severe bruises from several hundred to 1 million or more red blood cells per 1 mm3.
Diagnostic assessment of the number of red blood cells in the cerebrospinal fluid requires mandatory consideration of the clinical picture of TBI.
TREATMENT
Therapeutic measures for TSAH are aimed at stopping bleeding, normalizing intracranial pressure, removing spilled blood and its breakdown products and preventing complications.
Conservative therapy includes the prescription of hemostatic agents (dicinone, aminocalronic acid, calcium gluconate, etc.), dehydration therapy under the control of water-electrolyte balance (osmotic diuretics, saluretics), anti-inflammatory therapy according to indications (open penetrating head injury - broad-spectrum antibiotics covering gram-positive and gram-negative microflora ); vascular therapy and nootropics. Anticonvulsant therapy is carried out prophylactically. The use of calcium antagonists (nimodipine) in the treatment of TSCA, according to international cooperative studies (HIT I-IV trials), is not accompanied by reliable results, however, there is an improvement in the outcomes of TSCA in the group of patients who received the drug for a long time (21 days). Complex treatment is supplemented as necessary with symptomatic medications (analgesics, sedatives, vitamins, etc.). Victims must strictly adhere to bed rest.
Periodic lumbar punctures are used to sanitize the cerebrospinal fluid spaces with the removal of spilled blood and its breakdown products. In this case, clearing of the cerebrospinal fluid is observed within 7-14 days. Along with routine methods of cleansing liquor spaces, intensive methods of sanitation have been developed. They are indicated for massive TSCA in victims without signs of intracranial traumatic space-occupying formations, cerebral edema and dislocation manifestations. They are based on constant drainage of cerebrospinal fluid spaces with controlled removal of cerebrospinal fluid or its partial replacement (drainage of the subarachnoid space with the installation of lumbar drainage; drainage of cerebrospinal fluid spaces at different levels with washing with liquor-replacing solutions).
Previously widely used methods of endolumbar administration of air, oxygen, ozone, lidase and other drugs have now been abandoned due to the lack of reliable information about the positive effect of these methods on the outcomes of ASCA, and often the possibility of severe complications.
PROGNOSIS AND OUTCOMES
TSAC is one of the unfavorable factors in TBI. The course and outcomes of brain damage are influenced by the massiveness of TSACs and their localization, detected on primary CT studies. The age of the victims and alcohol intoxication during TSCA also affect the outcomes of TBI.
Against the background of mild TBI, good recovery is observed in the majority of victims with TSAC.
In moderate trauma, TSAC significantly increases the number of adverse outcomes. In particular, post-traumatic epilepsy develops in victims after TSCA twice as often as without it.
Poor outcomes, including death, vegetative state, and severe disability, are twice as likely to be observed in victims with severe TBI accompanied by ASCVD than in those without it.
HELL. Kravchuk, G.F. Dobrovolsky
Subarachnoid hemorrhage (SAH) is a pathology associated with penetration of blood into the subarachnoid cerebral space. Such hemorrhage can be spontaneous (non-traumatic) or traumatic in nature (traumatic hemorrhage). Most often, the pathology is diagnosed in elderly people, although it can also occur in a newborn child. The main cause of subarachnoid hemorrhage is a violation of the integrity of the aneurysm. In approximately 40% of cases, it occurs as a result of a traumatic brain injury.
Subarachnoid cerebral hemorrhage is a type where blood flows into the subarachnoid space. As a result, the level of cerebrospinal fluid increases, which causes.
Due to rapid ischemic disorders and vascular disorders, it occurs. This is what is associated with the high percentage of deaths. About 15% of victims die before the ambulance arrives, 25% do not survive the first day, 40% of patients die within the first week and about 20% within 6 months after suffering a subarachnoid cerebral hemorrhage.

Most often, doctors diagnose non-traumatic subarachnoid hemorrhage, which occurs spontaneously and is associated with vascular pathologies. This condition has an acute development and mostly occurs without obvious reasons. The patient requires immediate hospitalization.
Traumatic subarachnoid hemorrhage can occur due to a blow to the head, which results in vascular damage and bleeding.
There are 3 degrees of development of pathology:
- Blood enters the subarachnoid space and spreads through the liquor channels. Because of this, the victim’s intracranial pressure increases.
- Once in the cerebrospinal fluid, the blood clots. The resulting blood clots block the movement of cerebrospinal fluid.
- When blood clots dissolve, meningeal syndrome and aseptic inflammation occur.
Classification
If the artery is damaged, blood can flow not only into the subarachnoid space, but also into neighboring areas. Based on this, the following types of pathology are distinguished:
- Isolated hemorrhage - appears to be limited to the meninges.
- Subarachnoid parenchymal hemorrhage is characterized by blood leaking into the brain tissue.
- Subarachnoid ventricular (intraventricular hemorrhage) is distinguished by its localization in one of the ventricles of the brain.
- Subarachnoid parenchymal ventricular leads to damage to both the ventricles and other brain tissues.
Hosts of the program “Live Healthy!” Elena Malysheva and interventional cardiologist Gandelman German Shaevich will talk about the reasons for the rupture of a cerebral aneurysm:
There are the following types of SAC:
- Spontaneous subarachnoid hemorrhage. It has no connection with a traumatic factor and occurs as a result of spontaneous bleeding.
- Hemorrhage from the basilar artery. Bleeding occurs in the basilar region with subsequent penetration into the subarachnoid space.
- SAH from the communicating artery.
- Basal subarachnoid hemorrhage occurs when blood accumulates in the basal cisterns.
- Subdural hemorrhage occurs due to damage to large veins.
- Diffuse subarachnoid hemorrhage is associated with trauma, which resulted in numerous small hematomas.
Causes
In most cases, the cause of subarachnoid bleeding is a ruptured aneurysm. This is due to weakness in the walls of the blood vessels passing through the brain. Most often, their damage occurs at the point where small vessels depart from the main trunk.
Doctors cannot say for sure why a person develops an aneurysm. However, there are certain risk factors that can cause such a pathology:
- Arterial hypertension.
- Hereditary predisposition.
- Rare diseases of the body.
- Bad habits (smoking, alcohol and drug addiction).

One of the causes of the disease is arterial hypertension
In addition to rupture of aneurysms, other reasons can lead to a condition such as SAH:
- Injuries that may result in hemorrhage with blood entering the subarachnoid space.
- The development of a tumor in the brain, which leads to damage to nearby vessels. In this case, the nature of the neoplasm can be both malignant and benign.
- Arteriovenous malformations are a congenital pathology, as a result of which veins and arteries become intertwined.
- Vasculitis is an inflammatory lesion of blood vessels caused by an infectious or autoimmune process.
- Infectious lesion of the brain (complication of purulent meningitis, encephalitis, etc.).
- Fibromuscular dysplasia.
- Moyamoya disease.
Symptoms
Symptoms of subarachnoid hemorrhage usually occur suddenly. In this case, the patient experiences:
- Headache that can get worse with any movement.
- Photophobia.
- Cramps.

The photo shows one of the symptoms of the disease - nausea and vomiting.
- Psycho-emotional disorders (affective disorder), manifested in the form of increased excitability, drowsiness, etc.
- Impaired consciousness.
- Increased body temperature.
Signs of pathology can be observed for several days. If there is a disruption in the functioning of nerve endings and the cerebral cortex, the victim experiences:
- Speech problems.
- Loss of skin sensitivity.
- Strabismus.
A few hours after SAH, a person experiences the following symptoms:
- Stiff neck.
- Kernig's sign (the victim is unable to straighten the leg, bent at the hip and knee).
If massive subarachnoid hemorrhage is the result of trauma, then the symptoms will depend on the location where the blow was struck. When the frontal lobe is damaged, the following occurs:
- Speech impairment.
- Unsteadiness of gait.
- Cramps of the fingers of the upper limb.
- Behavioral changes.

Kernig's sign is one of the primary signs confirming the presence of irritation of the lining of the brain
In case of a temple injury, a person’s hearing and memory are impaired. Damage to the parietal zone entails a violation of tactile sensations, the inability to read and navigate in space. When hemorrhage occurs in the occipital region, vision is impaired and hallucinations occur.
With the development of a relapse, all manifestations of SAH intensify and new ones may arise. Sometimes your blood pressure may rise, your heart rhythm may become abnormal, your lungs will swell, or your heart may even stop.
The following symptoms indicate pathology in newborns:
- Excited state of the baby.
- Divergence of the skull bones and bulging of the fontanelle.
- Brain scream.
- Muscle hypertonicity.
- Strengthening innate reflexes.
- Cramps.
- Increased physical activity.
- Hyperesthesia.
- Sleep inversion.
Diagnostics
Subarachnoid hematoma or hemorrhage into the subarachnoid space can be detected using computed tomography. Doctor in the picture:
- Check for cerebral edema.
- Determine the location where the hemorrhage occurred.
- Assess the condition of the liquor system.
Why is a lumbar puncture done? Allergist-immunologist Ermakov Georgy Aleksandrovich will answer the question:
To determine the source of SAH, a test is required. If the CT result is negative, this indicates minor hemorrhage or examination at a later date. In this case, the condition of the cerebrospinal fluid is carried out and studied. The presence of pathology is indicated by an increased level of red blood cells.
If the cause of the disease is an aneurysm, it is necessary to do vascular angiography. To obtain detailed images of the brain, it is carried out.
Treatment
If a patient is suspected of having SAH, the doctor will immediately hospitalize him to confirm the diagnosis and begin treatment. In this case, the main task of doctors becomes:
- Stabilization of the victim's condition.
- Prevention of recurrent hemorrhage.
- Preventing damage to brain structures.
Drug therapy
Treatment of subarachnoid hemorrhage with drugs is aimed at:
- Reduced headache intensity.
- Normalization of blood pressure and restoration of cerebral circulation.
- Prevention of seizures, which are often a consequence of brain damage.

Codeine – analgesic, antitussive, antidiarrheal agent
In most cases, the patient is prescribed Nimodipine, a drug that helps normalize cerebral circulation and prevents the risk of relapse. Side effects of this medication include:
- Rash on the skin.
- Nausea.
- Headache.
- Tides.
- Tachycardia.
To reduce pain in the head, the patient is prescribed Codeine and Morphine. Additionally, for the treatment of pathology the following is used:
- Drugs with anticonvulsant effect (Phenytoin).
- Antiemetic drugs (“Promethazine”).
Surgical intervention
To restore the vessels damaged by the aneurysm and prevent recurrent hemorrhage, the doctor may prescribe surgery. There are 3 methods for doing this:
- Neurosurgical clipping. The operation is performed under general anesthesia. To gain access to the affected area, the surgeon will make a small incision and remove part of the skull bone. Next, a clip is applied to the neck of the aneurysm. Gradually, it will be overgrown with choroid and will be able to protect the aneurysm from enlargement and re-damage.
- Endovascular occlusion. Basically, the operation is performed under general anesthesia. During the intervention, the surgeon inserts a catheter through the inguinal artery, which is guided to the location of the aneurysm. Using such a catheter, a platinum spiral is inserted inside. The purpose of such a spiral is to prevent the growth of protrusion and reduce the likelihood of re-rupture of the vessel walls.
- Shunt surgery with removal of blood from the ventricles.

The photo shows endovascular occlusion
The method of performing the operation depends on the shape, size and location of the aneurysm. Endovascular occlusion is considered more gentle. After it is carried out, the patient’s recovery occurs much faster.
Contraindications to surgical intervention are:
- Coma state.
- Depression of consciousness.
- A sharp deterioration in the patient's condition.
- Neurological focal symptoms.
- Expressed.
Complications
Extensive subrarachnoid hemorrhage can lead to the development of a number of complications, including:
- Repeated bleeding can occur as a result of a new rupture of the walls of the aneurysm. The risk of such a complication is especially high during the first days after the first SAH. In case of repeated hemorrhage, the likelihood of disability or death increases significantly. Related to this is that treatment of an aneurysm should begin immediately after its diagnosis.
- Secondary ischemia is a complication that can occur due to spasm of the walls of blood vessels. In this case, blood circulation in the brain deteriorates significantly, which leads to damage to neurocytes. Secondary ischemia may occur during the first days after SAH. Its symptoms include: drowsiness, which can lead to a coma or weakness in the body (usually in one of the halves).
- Hydrocephalus is a pathology associated with excessive accumulation of cerebrospinal fluid in the brain. As a result, the patient experiences intracranial hypertension and damage to nerve cells. These include severe headaches, blurred vision, gait disturbance, and nausea. To treat this condition, a lumbar puncture or shunt is used to drain excess fluid from the brain.
Neurosurgeon Fayyad Akhmedovich Farhat talks about the symptoms and treatment of hydrocephalus:
In the case of subarachnoid hemorrhage, long-term consequences develop:
- Epilepsy. The disease is associated with impaired functioning of the brain, which is manifested by frequent seizures. This condition develops in approximately 5% of patients diagnosed with SAH. In this case, convulsions can have a different nature and duration of manifestation. Anticonvulsants (Carbamazepine) are prescribed to treat epilepsy.
- Cognitive impairment. The patient's memory suffers, it becomes difficult for him to perform ordinary actions, and concentration is impaired. Over time, many cognitive impairments may improve, but memory problems remain.
- Emotional disturbances. The patient suffers from prolonged depression and has anxiety disorders (panic, fear). To eliminate such symptoms, the use of antidepressants or psychotropic drugs is indicated.
Rehabilitation
The period required for the patient’s rehabilitation is directly related to the severity of the pathology. A course of exercise therapy, physiotherapy, and the help of speech therapists and rehabilitation specialists help speed up the process.
Table 1. Methods of rehabilitation after SAH
| Violation | Rehabilitation methods |
|---|---|
| Excessive fatigue | At first, people who have suffered a subarchnoid hemorrhage experience chronic fatigue. Even simple daily activities become difficult for them. Doctors recommend that they spend more time outdoors and relax. |
| Sleep disturbance | To cope with insomnia, patients need to follow a daily routine. It is important to set aside time for yourself to relax while working. |
| Headache | To relieve pain, you can take Paracetamol. It is important to drink more clean water without carbon and completely eliminate coffee, strong tea and alcoholic drinks. |
| Impaired mobility and sensitivity | If sensitivity is impaired in the extremities, a course of exercise therapy is indicated. |
| Visual impairment | Often after SAH, a person experiences a feeling of double vision or blurry vision. Treatment for this condition should be prescribed by an ophthalmologist. Usually this disorder goes away within a few months. |
Prognosis and prevention
According to statistics, only 1 in 4 people manage to fully restore their health after a subarachnoid hemorrhage. About 30% of patients suffer from severe neurological defects. The mortality rate from SAH is also very high.
To reduce the negative consequences of the disease and prevent its recurrence, patients are advised to:
- More time to walk in the fresh air.
- Eat well. At the same time, the diet should contain a sufficient amount of vitamins and microelements.

- Monitor blood pressure and blood glucose levels.
- Loads must be introduced gradually.
- Give up any bad habits.
Subarachnoid hemorrhage is a very dangerous pathology, often ending in death. In order for a person to not only survive, but also recover from an illness, it is important that if any symptoms appear, immediately consult a doctor and begin treatment.
Subarachnoid hemorrhage is a widespread pathological condition, which ranks third in frequency among all types of cerebral strokes. Most often it develops in people aged 30 to 55 years.
What is subarachnoid hemorrhage
The human brain is covered by three membranes:
- external (solid);
- middle (arachnoid);
- internal (vascular).
The space that is located between the dura mater and the arachnoid membrane is called the subdural, and between the arachnoid and vascular membranes is called the subarachnoidal space.
The outpouring of blood into the subarachnoid space or the accumulation of its coagulations, caused by impaired microcirculation, vasospasm and damage to the cerebral cortex, is called subarachnoid.
This pathological condition may also be called intracranial hemorrhage, hemorrhagic stroke or SAH.
Patients at risk for developing cerebral hemorrhage include:
- hypertension;
- autoimmune and degenerative diseases of the cerebral vessels;
- who take anticoagulant drugs, i.e. drugs that reduce the ability of blood to clot;
- with tumors of the brain and its membranes;
- with aneurysmal formations of cerebral vessels;
- with infectious and fungal lesions of the arteries and veins of the head;
- with cocaine addiction.
Classification of hemorrhages in the subarachnoid space: non-traumatic, traumatic, primary, isolated and others
If a vessel is damaged, blood can escape not only under the subarachnoid membrane, but also into neighboring anatomical structures. Therefore, the following types are distinguished:
- isolated - SAH is limited to the meninges;
- subarachnoid-parenchymal hemorrhage - occurs in brain tissue;
- subarachnoid-ventricular - hemorrhage into one of the ventricles (anatomical formation of the brain);
- subarachnoid-parenchymal-ventricular hemorrhage - affects not only the substance, but also the ventricles of the brain.
According to the reasons for the occurrence of SAH, they are distinguished:
- traumatic - the mechanical energy from a blow to the head is so strong that it can cause rupture of an artery or vein of the membrane or brain parenchyma. The consequences of such an impact are unpredictable and depend on its strength, the caliber of the vessel and the location of the hemorrhage;
- non-traumatic - develops due to an anomaly in the development of a vessel, infectious processes, pathology of the blood coagulation system, or an immediate increase in blood pressure.
Primary, or spontaneous, SAH occurs only with malformations of the cerebral vasculature. Secondary is caused by a variety of external factors that provoke rupture of a vein or artery.
Causes and factors for the development of SAH
Factors that can lead to subarachnoid hemorrhage are conventionally divided into several groups:
- Structural or anatomical - pathology of the development of the vascular wall or a violation of its integrity.
- Hemodynamic disturbances caused by high blood pressure.
- Dysfunction of the blood coagulation system.
The most common cause of subarachnoid hemorrhage is the rupture of a sac-like aneurysm, the size of which can range from 2 mm to several centimeters.
SAH is less commonly provoked by pathologies of the venous outflow from the brain, tumor destruction of blood vessels, and atherosclerotic damage to the arteries, which lead to their dissection.
Toxic substances and some medications affect the condition of the vascular wall, which leads to its rupture in weak spots. For example, Mannitol, which is used for intracranial hypertension, tends to cause “recoil” syndrome due to complex biochemical processes. A sharp repeated increase in pressure readings spasms the arteries of the brain and can provoke their rupture.
Subarachnoid hemorrhage often occurs after traumatic brain injury.
A very rare cause of SAH can be considered acute pancreatitis, which in advanced forms leads to the release of pancreatic enzymes into the blood, which damages the choroid of the brain. A similar phenomenon occurs during surgical interventions on the gland.
Elena Malysheva about subarachnoid hemorrhage - video
Symptoms and signs of subarachnoid hemorrhage
Clinical manifestations of SAH are divided into three periods, each of which has its own symptoms. It depends on the pathogenetic processes occurring after the rupture of the vessel.
- Pre-hemorrhagic, or the period before the onset of bleeding into the subarachnoid space, is manifested by periodic one-sided headaches, causeless dizziness, and loss of vision. If a vessel aneurysm is located in the brain parenchyma, then the patient may experience epileptic seizures, double vision, loss of part of the visual fields, and spasms of the facial muscles. Diagnosis of this period is very difficult, since in half of the patients the aneurysmal formation does not manifest itself.
- Hemorrhagic period - blood that flows from an aneurysm or a traumatically damaged vessel begins to gradually fill not only the subarachnoid space, but also other formations of the brain (ventricles, system of cisterns and cerebrospinal fluid channels), thereby causing increased pressure in them and an increase in the volume of cerebrospinal fluid ( fluid that bathes the brain and spinal cord). Clinically, this is manifested by an acute headache, heat throughout the body, and a sensation of hot liquid spreading throughout the head. Dizziness intensifies and after some time loss of consciousness occurs, up to a coma. After two weeks, memory loss, oral and written speech disorders, deterioration of mental health, as well as the development of paresis and paralysis are also observed. If hemorrhage occurs in the brain stem, where the centers of respiratory and cardiac activity are located, then death is inevitable.
- Posthemorrhagic period - occurs after the bleeding has been eliminated, and its manifestations depend on the degree of damage to brain structures and the speed of specialized medical care. Massive hemorrhage can lead to cerebral edema and hydrocephalus (an increase in the size of the skull), which further aggravates the course of the disease. Often, after emerging from a coma, the patient remains with symptoms of amnesia, mental retardation, absence or decreased sensitivity in the limbs.
Features of SAH of the brain in children and newborns
Birth trauma and prolonged stay without oxygen can cause circulatory disorders and subarachnoid hemorrhage in newborns. Low oxygen levels in the blood and a combination of other brain damage during childbirth can have very unpleasant and sometimes fatal consequences.
In newborns with SAH, the following is noted:
Older children diagnosed with SAH in infancy are delayed in physical and mental development, they continue to have signs of high blood pressure and an enlarged skull. Periodically, such patients suffer from epileptic seizures.
Diagnosis and differential diagnosis of the disease
Upon examination, the neurologist may suspect subarachnoid hemorrhage in the patient. But the symptoms are very nonspecific, and sometimes the patient is in a coma, which further confuses the diagnosis and determination of the obvious cause of brain disorders. Therefore, the main methods are instrumental:

Differential diagnosis is carried out with ischemic stroke, which is characterized by:
- the appearance of frequent, repeated symptoms that indicate a violation of cerebral circulation, but disappear within 12 hours;
- the presence of heart pathology, myocardial infarction, cardiac arrhythmia;
- ischemic disease of the lower extremities;
- manifestation of symptoms during sleep, after taking a hot bath, physical fatigue;
- gradual development of symptoms, with periodic extinction and increase in manifestations with renewed vigor;
- age over 55 years.
Therapeutic tactics for SAH
Treatment of subarachnoid hemorrhage is primarily aimed at providing adequate emergency care, stopping blood loss, reducing intracranial pressure and reducing cerebral edema.
Urgent measures
- During an epileptic attack, do not interfere with muscle contraction, do not try to stick out your tongue. At this moment, it is important to prevent additional trauma to the patient, try to place soft objects under parts of the body, and after the end of the convulsions, lay him on his side with the lower extremities secured.
- If you lose consciousness and stop breathing, call an ambulance, tilt the patient’s head back, push out the lower jaw and begin performing cardiopulmonary resuscitation with a ratio of sternum compressions to inhalations of 30:2.
When providing first aid, do not try to insert medications into the victim’s mouth.
Drug treatment
- To stop bleeding, use Aminocaproic acid, sodium etamsylate, Dicinone, Tranexam.
- To reduce intracranial pressure and cerebral edema under the control of the level of electrolyte blood parameters, Mannitol, Veroshpiron, Furosemide are used;
- To prevent ischemia of brain tissue and reflex vascular spasm - Nimotop.
- To eliminate the inflammatory process, in particular after a traumatic brain injury, antibiotics (Flemoclav, Sulbactomax, Cedoxime), as well as non-steroidal anti-inflammatory drugs (Ibuprofen, Diclofenac) are used.
- For indomitable vomiting - Cerucal, Metoclopramide.
- For repeated convulsions - Finlepsin.
- With a rapid increase in the volume of cerebrospinal fluid, shunting is performed, i.e. placing a catheter into the spinal canal or ventricles of the brain to drain the accumulated fluid.
Drugs for the treatment of SAH - photo gallery
 Aminocaproic acid is used to stop bleeding
Aminocaproic acid is used to stop bleeding  Cerucal is used to eliminate indomitable vomiting
Cerucal is used to eliminate indomitable vomiting  Diclofenac - eliminates inflammatory processes of the vascular wall
Diclofenac - eliminates inflammatory processes of the vascular wall  Sulbactomax - antibacterial drug
Sulbactomax - antibacterial drug  Mannitol - reduces cerebral edema
Mannitol - reduces cerebral edema  Tranexam - a drug to stop bleeding
Tranexam - a drug to stop bleeding  Nimotop - eliminates cerebral ischemia
Nimotop - eliminates cerebral ischemia  Finlepsin - prevents recurrent seizures
Finlepsin - prevents recurrent seizures
Surgical procedures: progress of the operation
Surgical intervention is indicated in case of rapid deterioration of the patient’s condition and the formation of a hematoma of significant size. Surgical treatment includes:
- preparing the patient and administering anesthesia;
- elimination of hematoma (blood accumulation) using a special aspiration needle and syringe or through trephination (opening) of the skull;
- coagulation of the vessel using a laser if the bleeding has not stopped. It is also possible to apply special clips or ligatures to the damaged artery.
For traumatic brain injury, surgical treatment is the main method, since, in addition to eliminating the source of hemorrhage, a comparison of the displaced skull bones is performed.
Rehabilitation
Restoring the body after this type of injury is a very complex and lengthy process. Not only proper home care is important, but also treatment in specialized centers. Rehabilitation activities include:

The use of traditional medicine in the development of subarachnoid hemorrhage is not only not advisable, but also absurd.
Prognosis, complications and consequences after SAH
The prognosis for the success of treatment for subarachnoid hemorrhage largely depends not only on the age category of the patient, the size of the damaged area, but also on the psychological support of loved ones, mood, motivation and, of course, the presence of consciousness.
After a patient has suffered SAH:
- phenomena of speech, memory, walking and coordination impairment may remain;
- prolonged vasospasm may be complicated by delayed cerebral infarction;
- massive hemorrhage, which affects large areas of nervous tissue, is fatal.
Preventive measures
In order to prevent the development of SAH it is necessary:
- adhere to proper nutrition and perform moderate physical activity;
- promptly eliminate surgically diagnosed aneurysmal formations of cerebral vessels;
- prevent increases or fluctuations in blood pressure;
- correct heart rhythm disturbances;
- Infectious or fungal diseases of blood vessels should be treated in a hospital setting.
Timely diagnosis of predisposing factors for subarachnoid hemorrhage will help not only to avoid death, but also to prevent a high level of severe disability in patients with this pathology. It is important to determine as soon as possible the possibilities of surgical treatment for a particular disorder of the blood supply to the brain in order to avoid serious complications.
Subarachnoid hemorrhage is a sudden bleeding that is quite often associated with a ruptured aneurysm or occurs. This is a very dangerous condition that quite often ends in death. Therefore, it is so important to call an ambulance in time.
Brain hemorrhages
Intracerebral or, as it is also called, parenchymal hemorrhage is considered a cerebral circulatory disorder of the hemorrhagic type. With this pathology, blood usually does not enter the cerebrospinal fluid.
Subarachnoid hemorrhage (SAH) is an acute cerebral circulatory disorder in which bleeding occurs between the arachnoid and pia mater.
Parenchymal-subarachnoid hemorrhage combines the signs of the above pathologies. In this case, hormetonia very often occurs, which is attacks of tonic muscle tension that alternate with hypotension. Loss of reactions to light stimuli and unilateral muscle paralysis are also characteristic.
With intraventricular hemorrhage, small vessels are damaged and blood enters the ventricles. Usually the vessels heal over time and the bleeding stops. This pathology is typical for premature babies.
Non-traumatic subdural and epidural hemorrhages are spontaneous and are usually associated with rupture of a small glial artery. Often these pathologies are associated with blood diseases.
Classification according to ICD-10
According to the International Classification of Diseases, 10th revision, the following types of subarachnoid hemorrhage can be distinguished:
- Spontaneous subarachnoid hemorrhage. This term refers to spontaneous bleeding into the subarachnoid space. The hemorrhage is not associated with head injuries.
- Subarachnoid hemorrhage from the basilar artery. In this case, bleeding begins in the basin of the basilar artery and enters under the arachnoid membrane of the brain.
- Subarachnoid hemorrhage from the middle cerebral artery. Bleeding occurs in the middle cerebral artery basin.
- Basal subarachnoid hemorrhage. The cause of the development of this pathology is often the rupture of an aneurysm. In this case, blood accumulates in the basal cisterns of the subarachnoid space.
- Subarachnoid hemorrhage from an aneurysm. Occurs in approximately 85% of cases. An aneurysm is an expansion of the lumen of an artery, which is associated with a change in its wall.
ICD-10 also distinguishes subarachnoid hemorrhage from the carotid sinus and bifurcation, from the anterior or posterior communicating artery, from the vertebral and other intracranial arteries.
A very large percentage of brain hemorrhages come from an aneurysm. But it is possible to do it in advance.
This pathology is mainly associated with loss of integrity of the walls of intracranial arteries. There are certain pathological conditions that increase the risk of developing this condition:
- Traumatic injury. TBI in this case is associated with brain contusion and loss of arterial integrity.
- Sudden rupture of an artery. Changes in the arterial wall can be influenced by the following:
- taking drugs;
- increased blood pressure;
- infections.
- Aneurysm rupture. Often occurs as a consequence of injury or infectious disease.
- Rupture of arteriovenous malformation.
Symptoms
As a rule, the main symptom of this pathology is a sharp headache, which is diffuse and pulsating in nature. This state usually lasts literally a few seconds. It is accompanied by dizziness, loss of vision, or a feeling of double vision.
Other symptoms include the following:
- Vomit.
- Delirium, confusion.
- Speech disorders.
- Convulsions, which occur in only 7% of all cases.
- Depressive state.
- Difficulty raising the eyelids.
- Bleeding in the eye.
- A sharp increase in pressure.
Subarachnoid hemorrhage in children and newborns
In children, this pathology appears as a result of brain contusion, skull fracture or hematoma inside the brain. Subarachnoid hemorrhage in children is often accompanied by conditions such as:
- motor excitement;
- disturbance of consciousness;
- meningeal symptoms;
- temperature fluctuations.
In newborns, this condition is usually a consequence of damage to the skull during childbirth.
This is due to a discrepancy between the size of the mother's birth canal and the baby's head. Typically, this pathology occurs during rapid or protracted labor. This condition is often associated with post-term pregnancy or premature birth. In addition, it may be the result of:
- hypoxia;
- somatic diseases in the mother;
- intrauterine infections;
- disorders of brain development in a child.
Diagnostics
To make a diagnosis, it is necessary to conduct a whole range of studies:
- Analysis of the patient's history and complaints. At this stage, the doctor collects the following information:
- how long ago the symptoms of the pathology began;
- whether there have been injuries or pressure surges;
- does the patient have bad habits?
- Examination of the patient. During this procedure, the doctor must look for symptoms of neurological disorders and assess the person’s level of consciousness.
- Blood analysis. Using this study, it is possible to determine blood clotting.
- Lumbar puncture. Using a special needle, you need to make a puncture in the lumbar region and take a couple of milliliters of cerebrospinal fluid. If there is hemorrhage in the subarachnoid space, then blood can be detected in the cerebrospinal fluid.
- Computer and With the help of these studies it is possible to study the structure of the brain and detect hemorrhage.
- Echoencephalography. Intracranial hemorrhage can cause the brain to become misaligned, and this procedure can detect this.
- Transcranial Dopplerography. With its help, it is possible to evaluate blood flow in the arteries of the brain. The fact is that with such hemorrhage, vasoconstriction occurs, and this fact can be established.
- Magnetic resonance angiography. Using this technique, the integrity of the cerebral arteries and their patency are assessed.
Everyone strives to get from point A to point B as quickly as possible, by traveling by plane. But sometimes the height difference can become...
Disease of the blood vessels of the brain - vascular dementia - can lead to memory impairment.
Treatment
If the patient has signs of subarachnoid hemorrhage, he is immediately hospitalized in a neurological hospital.
When identifying vascular pathologies that require surgical intervention, the decision on the timing of the operation is made on an individual basis. This is influenced by the patient’s age, the amount of hemorrhage, the severity of symptoms, and general health.
If there are no indications for surgery, conservative treatment is carried out. The main objectives of such therapy include:
- stabilization of the patient's condition;
- relapse prevention;
- maintaining homeostasis;
- treatment of the disease that led to the hemorrhage.
Using medications should stop bleeding and reduce the risk of complications.
- To relieve spasm and reduce ischemia, calcium antagonists are prescribed.
- To prevent the development of convulsive activity, the administration of phenytoin is indicated.
- Nitroprusside is prescribed to treat hypertension. Using this remedy, it is possible to prevent the threat of recurrent bleeding.
- Endothelial antagonists and magnesium sulfate are used as symptomatic agents.
Carefully! The video shows open brain surgery to remove a subarachnoid hemorrhage (click to open)
[collapse]
Typical clinic
This condition has an acute onset, which is characterized by a sudden headache. The patient may faint for a short time, and impaired consciousness is also often observed.
The person is in a state of anxiety and does not allow doctors to examine him/herself. As the meningeal syndrome decreases, these disorders begin to gradually decrease.
Vomiting, hiccups, and stiff neck are often observed. The medical history may include Kerning's sign and bradycardia. On the second day, low-grade fever often occurs.
If you do a lumbar puncture in the first days, you can see the cerebrospinal fluid, evenly stained with blood. After a few days it acquires a yellowish color, and after three weeks it becomes colorless, although it contains a lot of protein and leukocytes.
30% of patients with this pathology die. After an autopsy, a collection of blood clots can be detected at the base and convex part of the cerebral cortex.
Carefully! The photo shows the brain after subarachnoid hemorrhage (click to open)
[collapse]
Recovery
Rehabilitation after treatment of subarachnoid hemorrhage takes approximately six months. During this period, a person is forced to regularly take medications and undergo examination by a neurologist. Relatives must monitor his health.
As for indications for restoration, there are not too many of them. A person must give up bad habits and lead a calm lifestyle. It should be taken into account that this pathology belongs to the category of recurrent diseases.
Consequences of the disease
It is difficult to make a prognosis for subarachnoid hemorrhage. This pathology can have quite dangerous consequences for health:
- Neurological disorders. Muscle tone may increase, weakness in the limbs may appear, and speech disorders are often observed. A person may lose the ability to move independently, which threatens him with disability.
- Development of a heart attack. This is due to narrowing of the arteries or death of brain tissue.
- Threat of death. This risk is usually present with large volumes of hemorrhage. Death can also occur as a result of prolonged spasm of the cerebral arteries.
Subarachnoid hemorrhage in the brain is classified as a life-threatening pathology.
In addition, this condition can pose a serious threat to human health. To minimize the risk of complications, it is very important to consult a doctor in a timely manner - this will help you maintain your health and life.
Video illustrates current scientific knowledge on subarchonoid hemorrhage: