Ligaments of the abdominal cavity. Mesenteric sinuses (sinuses) and channels of the abdominal cavity
The abdominal cavity is the part of the abdominal cavity covered by the parietal peritoneum. In men, it is closed, and in women it communicates with the uterine cavity through the openings of the fallopian tubes.
The visceral peritoneum covers the organs located in the abdominal cavity. Organs can be covered by the peritoneum on all sides (intraperitoneally), on three sides (mesoperitoneally) and extraperitoneally (on one side or lying extraperitoneally). The organs covered by the peritoneum intraperitoneally have significant mobility, which is increased by the mesentery or ligaments. The displacement of meso-peritoneal organs is insignificant (Fig. 123).
A feature of the peritoneum is that the mesothelium (the first layer of the peritoneum) forms a smooth surface that ensures the sliding of the organs during their peristalsis and changes in volume. In the peritoneal cavity, under normal conditions, there is a minimal amount of transparent serous fluid, which moisturizes the surface of the peritoneum and fills the gaps between organs and walls. The movements of organs in relation to each other and to the abdominal wall are made easily and without friction due to the fact that all contact surfaces are smooth and moist. Between the anterior wall of the abdomen and the internal organs there is a gasket-omentum. "
In the region of the diaphragm, the peritoneum becomes thinner at the site of the “suction hatches”. The lumen of the hatches changes during the respiratory movements of the diaphragm, which ensures their pumping action. "Suction hatches" are also present in the peritoneum of the rectovesical cavity in men and the recto-uterine cavity in women.
There are transuding, absorbing and indifferent to the abdominal fluid areas of the peritoneum. Transuding areas are the small intestine and broad ligaments of the uterus. The suction parts of the parietal peritoneum are the diaphragm and the iliac fossae.
The abdominal cavity of the mesentery of the transverse colon is divided into two floors: upper and lower, which communicate with each other in front through the preomental fissure and from the sides - through the right and left lateral canals. In addition, the peritoneal floor of the small pelvis is isolated
The upper floor of the abdominal cavity is located between the diaphragm and the mesentery of the transverse colon. It contains intraperitoneally covered stomach, spleen and mesoperitoneally - liver, gallbladder and upper part of duodenum. The pancreas belongs to the upper floor of the abdominal cavity, although it lies retroperitoneally, and part of the head is located below the root of the mesentery of the transverse colon. The listed organs, their ligaments and the mesentery of the transverse colon limit isolated spaces, cracks and bags in the upper floor of the abdominal cavity.
Top floor bags. The space between the diaphragm and the liver is divided by the falciform ligament into two sections: left and right.
The right liver bag, or bursa hepatica dextra, is the gap between the right lobe of the liver and the diaphragm. It is bounded above by the diaphragm, below by the right lobe of the liver, behind by the right part of the coronary ligament, and to the left by the falciform ligament of the liver. It distinguishes the right subdiaphragmatic space and subhepatic.
The right subphrenic space is located most deeply between the posterior surface of the right lobe of the liver, the diaphragm, and the coronary ligament. It is in the subdiaphragmatic space, as in the deepest place of the hepatic sac, that the fluid that has poured into the abdominal cavity can be retained. The subphrenic space in most cases directly passes into the right lateral canal of the lower floor of the abdominal cavity. Therefore, inflammatory exudate from the right iliac fossa can freely move towards the subphrenic space and lead to the formation of an encysted abscess, called a subphrenic abscess. It most often develops as a complication of perforated gastric and duodenal ulcers, destructive appendicitis, cholecystitis.
The subhepatic space is the lower section of the i fava of the hepatic sac and is located between the lower surface of the right lobe of the liver, the transverse colon and its mesentery, to the right of the gate of the liver and the hepatoduodenal ligament. In the subhepatic space, the anterior and posterior sections are distinguished. Almost the entire peritoneal surface of the gallbladder, the upper outer surface of the duodenum, faces the anterior part of this space. The posterior section, located at the posterior edge of the liver, is the least accessible part of the subhepatic space - a recess called the renal-hepatic pocket. Abscesses resulting from perforation of a duodenal ulcer or purulent cholecystitis are more often located in the anterior section, while the distribution of the periappendicular abscess occurs mainly in the posterior section of the subhepatic space.
The left subdiaphragmatic space consists of widely communicating bags: the left hepatic and pregastric.
The left hepatic bursa is a gap between the left lobe of the liver and the diaphragm, bounded on the right by the falciform ligament of the liver, behind the left part of the coronary ligament and the left triangular ligament of the liver. This bursa is much smaller in width and depth than the right hepatic bursa and is not usually identified as a distinct part of the subdiaphragmatic space.
The pregastric sac is bounded behind by the lesser omentum and stomach, the upper left lobe of the liver, the diaphragm, in front by the anterior abdominal wall, on the right by the falciform and round ligaments of the liver, on the left, the pregastric sac has no pronounced border. In the outer-posterior section of the left subdiaphragmatic space, the spleen is located with ligaments: gastrosplenic and diaphragmatic-splenic. () t of the left lateral canal, it is separated by the left phrenic-colic ligament. This ligament is often wide, it covers the lower pole of the spleen and is called the suspensory ligament of the spleen. Thus, the bed of the spleen is well demarcated from the left lateral canal, this is a blind pocket (saccus caecus lienalis). The left subdiaphragmatic space plays a much smaller role than the right one as a site of abscess formation. Purulent processes rarely developing in this space tend to spread between the left lobe of the liver and stomach down to the transverse colon or to the left to the blind sac of the spleen. Communication between the right hepatic and pregastric bags is carried out through a narrow gap between the liver and the pyloric part of the stomach, in front of the lesser omentum.
Stuffing bag (bursa omentalis) is a large closed slit-like space of the abdominal cavity, the most isolated and deep.
The anterior wall of the omental sac is formed by the lesser omentum, the posterior wall of the stomach, and the gastrocolic ligament (the initial part of the greater omentum). The lesser omentum is three ligaments that pass one into the other: hepatic-duodenal, hepatic-gastric and diaphragmatic-gastric. The lower wall of the omental sac is formed by the transverse colon and its mesentery. From above, the omental bag is bounded by the caudate lobe of the liver and the diaphragm, the posterior wall is formed by the parietal peritoneum, which covers the front of the pancreas, aorta, inferior vena cava, the upper pole of the left kidney with the adrenal gland, on the left it is limited by the spleen with the gastrosplenic ligament, and the right wall is not expressed.
In the omental bag, depressions or inversions are distinguished: the upper one is located behind the caudate lobe of the liver and reaches the diaphragm, the lower one is in the region of the mesentery of the transverse colon and the spleen.
Entry into the omental bag is possible only through the omental opening, bounded in front by the hepatoduodenal ligament, behind by the hepatorenal ligament, in the thickness of which lies the inferior vena cava, above by the caudate lobe of the liver, below by the renal-duodenal ligament.
The stuffing hole passes one or two fingers, but in case of adhesion formation it can be closed and then the stuffing bag is a completely isolated space. In the omental bag, the contents of the stomach can accumulate when the ulcer is perforated;
nigsya purulent processes as a result of inflammatory diseases of the pancreas.
There are three operational accesses to the stuffing bag for examination, revision of organs and operations on them (Fig. 124):
1. Through the gastrocolic ligament, which is most preferable, since it can be dissected widely. It is used to examine the posterior wall of the stomach and pancreas in case of inflammation and trauma.
2. Through the hole in the mesentery of the transverse colon in an avascular place, you can examine the cavity of the omental bag, apply a gastrointestinal anastomosis.
3. Access through the hepatogastric ligament is more convenient when the stomach is prolapsed. Used in operations on the celiac artery.
Channels and sinuses of the lower floor. The lower floor of the abdominal cavity occupies the space between the mesentery of the transverse colon and the small pelvis. The ascending and descending colons, the root of the mesentery of the small intestine divide the lower floor of the abdominal cavity into four sections: the right and left side canals and the right and left (mesenteric sinuses (Fig. 125).
The right lateral canal is located between the ascending colon and the right lateral wall of the abdomen. At the top, the canal passes into the subscapular space, at the bottom - into the right iliac fossa, and then into the small pelvis.
The left lateral canal is limited by the descending colon and the left lateral wall of the abdomen and passes into
left iliac region. The deepest in the horizontal position are the upper sections of the canals.
The right mesenteric sinus is limited to the right by the ascending colon, from above by the mesentery of the transverse colon, to the left and below by the mesentery of the small intestine. This sinus is largely delimited from other parts of the abdominal cavity. In the horizontal position, the upper right angle of the sinus is the deepest.
The left mesenteric sinus is larger than the right one. From above it is bounded by the mesentery of the transverse colon, on the left by the descending colon and the sigmoid mesentery, on the right by the mesentery of the small intestine. From below, the sinus is not limited and directly communicates with the pelvic cavity. In the horizontal position, the superior angle of the sinus is the deepest. Both mesenteric sinuses communicate with each other through a gap between the mesentery of the transverse colon and the initial part of the jejunum. Inflammatory exudate from the mesenteric sinuses may spread into the lateral channels of the abdominal cavity. The left mesenteric sinus is larger than the right one, and due to the absence of anatomical restrictions in its lower sections, suppurative processes that develop in the sinus tend to descend into the pelvic cavity much more often than from the right mesenteric sinus.
Along with the tendency for inflammatory exudates to spread through all the crevices of the abdominal cavity, there are anatomical prerequisites for the formation of encysted peritonitis both in the lateral canals and in the mesenteric sinuses, especially in the right one, as it is more closed. During operations on the abdominal organs, especially with peritonitis, it is important to divert the loops of the small intestine first to the left, then to the right and remove pus and blood from the mesenteric sinuses to prevent the formation of encysted abscesses.
Abdominal pockets. The peritoneum, passing from organ to organ, forms ligaments, next to which there are recesses, called pockets (recessus).
Recessus duodenojejunalis is formed at the junction of the duodenum into the jejunum, recessus iliocaecalis superior is formed at the confluence of the ileum into the caecum in the region of the upper ilio-caecal angle, recessus iliocaecalis inferior is formed in the region of the lower ileo-caecal angle, recessus retrocaecalis is located behind the caecum, recessus intersigmoideus is a funnel-shaped recess e between the mesentery of the sigmoid colon and the parietal peritoneum, its beginning is turned into the left lateral canal.
Peritoneal pockets can become the site of internal hernia formation. Peritoneal pockets with internal hernias can reach very large sizes. Internal hernias can become strangulated and cause intestinal obstruction.
Topographic anatomy of the stomach. The stomach is the main organ of the digestive system and is a mystical sac-like extension of the digestive tract located between the esophagus and the duodenum.
Holotopia. The stomach is projected onto the anterior abdominal wall in the left hypochondrium and its own epigastric region.
Departments. The inlet of the stomach is called cardiac, and the outlet is called pyloric. The perpendicular, descending from the esophagus to the greater curvature, divides the stomach into a cardial section, consisting of the fundus and body, and a pyloric section, consisting of the vestibule and pyloric canal. In the stomach, there is a greater and lesser curvature, anterior and posterior surfaces.
Syntopy. The concept of "syntopic fields of the stomach" is distinguished. These are the places where the stomach comes into contact with neighboring organs. Syntopic fields of the stomach must be taken into account in case of combined wounds, penetration of ulcers and germination of stomach tumors. Three syntopic fields are distinguished on the anterior wall of the stomach: hepatic, diaphragmatic and free, which is in contact with the anterior wall of the abdomen. This field is also called the gastric triangle. This site is commonly used for gastrotomies and gastrostomies. The size of the gastric triangle depends on the filling of the stomach. Five syntopic fields are distinguished on the posterior wall of the stomach: splenic, renal, adrenal, pancreatic, and gastrointestinal.
Position. In the abdominal cavity, the stomach occupies a central position in the upper floor. Most of the stomach is located in the left subphrenic space, limiting the pancreatic sac in the back and the omental sac in front. The position of the stomach corresponds to the degree of inclination of the longitudinal axis of the stomach. Shevkunenko, in accordance with the location of the axis of the stomach, identified three types of positions: vertical (hook shape), horizontal (horn shape), oblique. It is believed that the position of the stomach is directly dependent on the type of physique.
relation to the peritoneum. The stomach occupies an intraperitoneal position. In places of transition of the sheets of the peritoneum on the lesser and greater curvature, ligaments of the stomach are formed. Ligaments of the stomach are divided into superficial and deep. Surface bonds:
1) gastrocolic (part of the greater omentum);
2) gastro-splenic, short gastric vessels pass through it, splenic vessels are located behind the ligament;
3) gastro-diaphragmatic;
4) diaphragmatic-esophageal, in it passes the esophageal branch from the left gastric artery;
5) hepatogastric, in it along the lesser curvature is the left gastric artery and vein;
6) hepato-pyloric - continuation of the hepatic / laryngeal ligament. It has the form of a narrow strip stretched between the gates of the liver and the pylorus, is an intermediate part between the hepatic-gastric and hepato-duodenal in dogs and serves as the right border when dissecting the ligaments of the stomach.
Deep Ligaments:
1) gastro-pancreas (during the transition of the peritoneum from the upper-I icro edge of the pancreas to the posterior surface of the stomach);
2) with pyloric-pancreas (between the pyloric otic um of the stomach and the right side of the body of the pancreas);
3) lateral diaphragmatic-piciform.
Blood supply of the stomach. The stomach is surrounded by a ring
wide anastomosing vessels giving off intramural branches and forming a dense network in the submucosa (Fig. 126). The source of blood supply is the celiac trunk, from which the left gastric artery departs, which goes directly to the lesser curvature of the stomach. The right gastric artery departs from the common hepatic artery, which anastomoses with the left on the lesser curvature of the stomach, forming an arterial arc of the lesser curvature. The left and right gastroepiploic arteries form an arc of greater curvature, and there are also short gastric arteries.
Innervation of the stomach. The stomach has a complex nervous apparatus. The main sources of innervation are the vagus nerves, the celiac plexus and its derivatives: gastric, hepatic, splenic, superior mesenteric plexus. The vagus nerves, branching on the esophagus, form the esophageal plexus, I de branches of both nerves are mixed and repeatedly connected. Passing from the esophagus to the stomach, the branches of the esophageal plexus are concentrated into several trunks: the left one passes to the anterior surface of the stomach, and the right one to the posterior surface of the stomach, giving branches to the liver, solar plexus, kidney and other organs. A long branch of Latarjet departs from the left vagus nerve to the pyloric section of the stomach. vagus nerves are a complex conduction system that connects nerve fibers of various functional purposes to the stomach and other organs. Between the left and right nerves there are a large number of connections in the chest and abdominal cavities, here there is an exchange of fibers. Therefore, it is impossible to talk about the exclusive innervation of the anterior wall of the stomach by the left vagus nerve, and the posterior wall by the right one. The right vagus nerve goes more often in the form of a single trunk, and the left one forms from one to four branches, more often there are two.
Lymph nodes of the stomach. Regional lymph nodes of the stomach are located along the lesser and greater curvature, as well as along the left gastric, common hepatic, splenic and celiac arteries. According to A. V. Melnikov (1960), lymph outflow from the stomach occurs through four main collectors (pools), each of which includes 4 stages.
Collector I of the lymphatic outflow collects lymph from the pyloric-angral part of the stomach, adjacent to the greater curvature. The first stage is the lymph nodes located in the thickness of the gastrocolic ligament along the greater curvature, near the pylorus, the second stage is the lymph nodes along the edge of the pancreatic head under and behind the pylorus, the third> tap is the lymph nodes located in the thickness of the mesentery of the small intestine, and the fourth is the retroperitoneal para-aortic lymph nodes.
In the 7/ collector of the lymphatic outflow, lymph flows from the part of the pyloric-antral section adjacent to the lesser curvature, and partly from the body of the stomach. The first stage is the retropyloric lymph nodes, the second is the lymph nodes in the lesser omentum in the dietary part of the lesser curvature, in the region of the pylorus and duodenum, immediately behind the pylorus, the third stage is the lymph nodes located in the thickness of the hepatic o-gastric ligament. The fourth stage A. V. Melnikov considered the lymph nodes in the gates of the liver.
Collector III collects lymph from the body of the stomach and lesser curvature, adjacent sections of the anterior and posterior walls, paintings, the medial part of the fornix and the abdominal esophagus. The first stage is the lymph nodes located in the form of a chain along the lesser curvature in the fiber of the lesser omentum. The upper nodes of this chain are called paracardial; in cancer of the cardia, they are affected by metastases in the first place. Lymph nodes along the left gastric vessels, in the thickness of the gastro-pancreatic ligament, are the second stage. I third stage - lymph nodes along the upper edge of the pancreas and in the region of its tail. The fourth stage is the lymph nodes in the paraesophageal tissue above and below the diaphragm.
In the IV collector, lymph flows from the vertical part of the greater curvature of the stomach, the adjacent anterior and posterior walls, and a significant part of the fornix of the stomach. Lymph nodes located in the upper left gastrocolic ligament are the first stage. The second stage is the lymph nodes along the short arteries of the stomach, the third stage is the lymph nodes in the hilum of the spleen. A. V. Melnikov considered the defeat of the spleen to be the fourth stage.
Knowledge of the anatomy of the regional lymph nodes of all collectors is extremely important for the correct operation of the stomach in compliance with oncological principles.
Topographic anatomy of the duodenum. The duodenum (duodenum) is the initial section of the small intestine. In front, it is covered by the right lobe of the liver and the mesentery of the transverse colon, it itself covers the head of the pancreas, so the duodenum lies deep and does not directly adjoin the anterior abdominal wall anywhere. The duodenum is divided into four parts. It consists of upper horizontal, descending, lower horizontal and ascending parts. Knowing the syntopy of the duodenum helps to explain the direction of penetration of the ulcer, the germination of the tumor and the spread of phlegmon during retroperitoneal rupture of the organ.
The upper part of the duodenum, 4-5 cm long, is located between the pylorus and the upper flexure of the duodenum and goes to the right and back along the right surface of the spine, passing into the descending part. This is the most mobile section of the intestine, covered on all sides by the peritoneum. All other sections of the intestine are covered with peritoneum only in front. In the initial section of the duodenum, an extension is determined, which is called the duodenal bulb. The upper part of the duodenum from above; in contact with the square lobe of the liver, in front - with the gallbladder, behind - with the portal vein, gastroduodenal artery, common bile duct. From below and from the inside, the head of the pancreas is adjacent to the intestine.
The descending part of the duodenum, 10-2 cm long, is located between the flexura duodeni superior and flexura duodeni inferior. This part of the duodenum is inactive and is covered by the peritoneum only in front. The descending part of the duodenum in front borders on the right lobe of the liver, the mesentery of the transverse colon, behind - with the gate of the right kidney, renal pedicle, inferior vena cava. Outside, the ascending part and the hepatic flexure of the colon are adjacent, from the inside, the head of the pancreas. The common bile duct and the pancreatic duct open into the descending part of the duodenum. They perforate the postero-meshal wall of the descending part of the duodenum in its middle section and open on the major (vater) papilla of the duodenum. Above it, there may be a non-permanent small duodenal papilla, on which the accessory pancreatic duct opens.
From the lower bend of the duodenum begins - 1 "and its horizontal part 2 to 6 cm long, covered in front by the peritoneum. The horizontal (lower) part lies at the level of the III and IV lumbar vertebrae, below the mesentery of the transverse colon, partly behind the root of the mesentery of the small intestine. The following organs adjoin these sections of the duodenum: from above - the head and body of the pancreatic gland, in front - the transverse colon, loops of the race intestines, the root of the mesentery of the small intestines and the upper mesenteric vessels. a, left renal vein.
Tie the duodenum. The hepatoduodenal ligament is located between the hilum of the liver and the initial Hi (fracture of the upper part of the duodenum. It fixes the I initial section of the intestine and limits the omental opening< переди. В связке располагаются: общий желчный проток справа, | обственная печеночная артерия слева, а между ними и сзади - поротная вена. Двенадцатиперстно-почечная связка в виде склад- Mi брюшины натянута между наружным краем нисходящей части шенадцатиперстной кишки и правой почкой, где она переходит в париетальную брюшину, расположенную кпереди от почки. Она 01 раничивает сальниковое отверстие снизу. Большую роль в фик- i.iiшп двенадцатиперстно-тощекишечного изгиба играет связка I рейтца (lig. duodenojejunalis).
In the upper part of the duodenum is covered with peritoneum from ■ h ex sides. The descending and horizontal parts are located retroperitoneally, the ascending part occupies an intraperitoneal position.
The blood supply of the duodenum (see Fig. 126) I a "strikes from the system of the celiac trunk and the superior mesenteric irgern. The upper and lower pancreatic-duodenal arteries have anterior and posterior branches. As a result of the anastomosis, anterior and posterior arterial arches are formed between them, which run between the concave semicircle of the duodenum and the head of the pancreas, which makes it impossible to separate them during surgery and forces them to be removed as a single block - pancreatoduodenal resection, performed, for example, in cancer of the Vater nipple or tumor of the head of the pancreas.
Large glands of the digestive tract
Topographic anatomy of the liver. The liver is one of the large glands in the digestive tract. The liver is distinguished by four morphofunctional features: 1) is the largest organ; 2) has three circulatory systems: arterial, venous and portal; 3) all substances that enter the gastrointestinal tract pass through it; 4) serves as a huge blood depot; 5) participates in all types of metabolism, synthesizes albumins, globulins, factors of the blood coagulation system, plays an important role in carbohydrate and fat metabolism and detoxification of the body, plays an important role in lymph production and lymph circulation.
Gayutopia. The liver of an adult is located in the right hypochondrium, the epigastric region proper, and partially in the left hypochondrium. The projection of the liver on the anterior abdominal wall looks like a triangle and can be built on three points: the upper point is on the right at the level of the 5th costal cartilage along the midclavicular line, the lower point is the 10th intercostal space along the midaxillary line, on the left - at the level of the 6th costal cartilage along the parasternal line. The lower border of the liver coincides with the costal arch. Behind the liver is projected onto the chest wall, to the right of the 10-11th thoracic vertebrae.
The position of the liver. The liver in relation to the frontal plane can be located: 1) in the dorsopetal position, the diaphragmatic surface of the liver is thrown back and its front edge can be located above the costal arch; 2) in the ventropetal position, the diaphragmatic surface faces forward, and the visceral surface faces backwards. In the ventropetal position, surgical access to the lower surface of the liver is difficult, and in the dorsopetal position, to the upper one.
The liver can occupy a right-sided position, then its right lobe is highly developed, and the size of the left lobe is reduced. () the organ occupies an almost vertical position, sometimes located only in the right half of the abdominal cavity. The left-sided position of the liver is characterized by the location of the organ in the horizontal plane and with a well-developed left lobe, which in some cases can go beyond the spleen.
Syntopy of the liver. The diaphragmatic surface of the right juli of the liver borders on the pleural cavity, the left lobe - on the pericardium, from which it is separated by the diaphragm. The visceral surface of the liver comes into contact with various organs, from which depressions form on the surface of the liver. The left lobe of the liver borders the lower end of the esophagus and the stomach. The pyloric part of the stomach is adjacent to the square lobe. The right lobe of the liver in the region of the neck of the gallbladder adjoins the upper horizontal part of the duodenum. 11 to the right is in contact with the transverse colon and the hepatic curvature of the colon. Posterior to this impression, the surface of the right lobe of the liver borders the right kidney and adrenal gland. Syntopy of the liver must be taken into account when assessing possible options for combined injuries of the abdominal and thoracic cavities.
The gate of the liver is an anatomical formation, which is made up of the transverse and left longitudinal grooves of the visceral surface of the liver. Here, vessels and nerves enter the liver and bile ducts and lymphatic vessels exit. In the gates of the liver, the vessels and ducts are accessible for surgical treatment, since they are located superficially, outside the parenchyma of the organ. Of practical importance is the shape of the gate: open, closed and intermediate. With an open form of the gate of the liver, the transverse sulcus communicates with the left sagittal and accessory sulci, thereby creating favorable conditions for access to the lobar and segmental ducts. With a closed form of the gate of the liver, there is no communication with the left sagittal sulcus, there are no additional grooves, the size of the gate is reduced, therefore, it is impossible to isolate segmental vessels and ducts in the gate of the liver without dissecting its perenchyma.
The gates of the liver can be located in the middle between the edges of the liver or shifted to its posterior or anterior edge. In the case of posterior displacement of the gate, more difficult conditions are created for prompt access to the vessels and ducts of the portal system during liver resections and operations on the biliary tract.
The relation to the peritoneum is mesoperitoneal, that is, the liver is covered with peritoneum on three sides. The posterior surface of the liver is not covered by the peritoneum, it is called the extraperitoneal field of the liver or pars m.ida.
The ligamentous apparatus of the liver is usually divided into true ligaments and peritoneal ligaments. True ligaments: 1) coronary, firmly fixing the posterior surface of the liver to the diaphragm, turning into triangular ligaments at the edges; 2) sickle-shaped, located in the sagittal plane at the border of the right and left lobes and turning into a steep ligament, which goes to the navel and contains a partially obliterated umbilical vein. From the visceral surface of the liver, the peritoneal ligaments are sent down to the organs: hepatogastric and hepatoduodenal. The hepatoduodenal ligament (ligament of life) is considered the most important, since the common bile duct (on the right), the common hepatic artery (on the left) and the portal vein pass through it, lies between them and posteriorly. Clamping of the hepatoduodenal ligament with fingers or a special instrument is used to temporarily stop bleeding from the liver.
Fixing apparatus of the liver. The liver is kept in the correct anatomical position: 1) extraperitoneal field (part of the posterior surface of the liver, not covered by the peritoneum); 2) the inferior vena cava, lying on the posterior surface of the liver and receiving the hepatic veins. Above the liver, the vein is fixed in the opening of the diaphragm, below it is firmly connected with the spine; 3) intra-abdominal pressure, muscle tone of the anterior abdominal wall and suction action of the diaphragm; 4) ligaments of the liver.
Blood supply to the liver. Two vessels bring blood to the liver: the hepatic artery and the portal vein, respectively 25 and 75%. The arterial supply of the liver comes from the common hepatic artery, which, after departing from it by the gastroduodenal artery, is called the proper hepatic artery and is divided into the right and left hepatic arteries.
Portal vein, v. porta, is formed behind the head of the pancreas. This is the first section of the vein, which is called the pars pancreatica. The second section of the portal vein is located behind the upper horizontal part of the duodenum and winds pars retroduodenalis. The third section of the vein is located in the head of the hepatoduodenal ligament above the upper horizontal part of the duodenum and is called pars supraduodenaiis. The portal vein collects blood from unpaired organs of the abdominal cavity: intestines, spleen, stomach, and is formed from three large trunks: the splenic vein, superior mesenteric and inferior mesenteric veins.
At the hilum of the liver, the hepatic artery, portal vein, and bile duct form the portal triad, Glisson's triad.
Liver jen, vv. hepatic i, are collected from the central lobular veins and, ultimately, form three large trunks, the right, left and middle hepatic veins, which emerge from the liver tissue on the posterior surface at the upper edge (caval portal of the liver) and flow into the inferior vena cava at the level of its transition through the diaphragm.
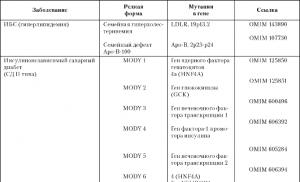
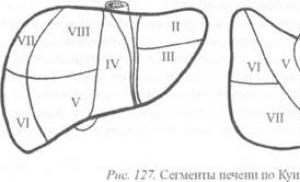
The structure of the liver, segmental division. The division of the liver into the right, left, caudate and square lobes, accepted in classical anatomy, is unacceptable for surgery, since the outer boundaries of the lobes do not correspond to the internal architectonics of the vascular and biliary systems. The modern division of the liver into segments is based on the principle of coincidence of the course of the first-order branches of the three liver systems: portal, arterial and bile, as well as the location of the main venous trunks of the liver. The portal vein, hepatic artery, and bile ducts are called the portal system (portal triad, Glisson triad). The course of all elements of the portal system inside the liver is relatively the same. The hepatic veins are called the caval system. The course of the vessels and bile ducts of the portal system of the liver does not coincide with the direction of the vessels of the caval system. Therefore, division of the liver according to the portal sign is now more common. The division of the liver along the portal system is of greater importance for the surgeon, since it is with the isolation and ligation of the vascular-secretory elements in the gates of the liver that the resection of this organ begins. However, when performing a resection based on liver division along the portal system, it is necessary to take into account the course of the hepatic veins (caval system) so as not to disturb the venous outflow. In clinical practice, the scheme of segmental division of the liver according to Quino, 1957 (Fig. 127) has become widespread. According to this scheme, the liver is divided into two lobes, five sectors and eight segments. The segments are arranged in radii around the gate. Lobe, sector and segment is called a section of the liver, which has separate blood supply, bile outflow, innervation and lymph circulation. The lobes, sectors and segments of the liver are separated from each other by four main gaps.
 |
Mesenteric sinuses (sinuses) and channels of the abdominal cavity. Ways
Distribution of streaks in the abdominal cavity. Topographic
Anatomical rationale for the occurrence of internal hernias
Abdominal cavity.
Right mesenteric sinus, sinus mesentericus dexter, limited from above
mesentery of the transverse colon, on the right - ascending ob-
daughter intestine, on the left and below - the mesentery of the small intestine and termi-
the nasal part of the ileum. Separated from the pelvis
terminal section of the small intestine and its mesentery; with the left mesenteric
the eternary sinus has a message over the duodenal-skinny from-
fold of the small intestine. Left mesenteric sinus
sinister, is located to the left and downward from the root of the mesentery of the small intestine.
From above it is limited by the mesentery of the transverse colon, on the left
Descending colon and mesentery of the sigmoid colon
on the right - the mesentery of the small intestine. Left mesenteric sinus wide
communicates with the pelvic cavity. Upper left sinus
in front is usually covered by a large omentum, transverse colon
intestine and its mesentery. Right lateral canal, canalis lateralis dexter,
located between the lateral wall of the abdomen and the right (ascending)
part of the colon lying mesoperitoneally. Top channel
passes into the posterior part of the right subdiaphragmatic space,
below - in the right iliac fossa. Left lateral canal, canalis
lateralis sinister, limited by the left side wall of the abdominal cavity,
covered by the parietal peritoneum, and the left (descending) section
colon, also located mesoperitoneally. Aperture-
small colic ligament, lig. phrenicocolicum, delimits at the top
lateral canal from the bed of the spleen and the left subphrenic passage
wanderings. At the bottom, the left side channel freely passes into the left
iliac fossa and then into the small pelvis. Duodenal transition
the intestines in the lean looks like a bend and is called flexura duodenojejunalis.
It is usually located on the left side of the body of the II-III lumbar vertebrae.
under the root mesocolon transversum. Behind the bend there is usually
pocket (deepening), recessus duodenojejunalis. It is limited in front
plica duodenojejunalis, the fold of the peritoneum between the fold and the root
mesentery of the transverse colon, behind - parietal li-
drainage of the peritoneum of the posterior abdominal wall, from above - mesocolon
transversum, from below - by the upper edge of the duodenum-jejunum bend.
In some cases recessus duodenojejunalis can be large
sizes, turn into a pocket, extending into the retroperitoneal tissue,
forming a hernial sac. This bag can be penetrated by loops of thin
intestines, thus forming a true internal hernia in the area
flexura duodenojejunalis, called duodenojejunalis hernia
kink, or Treitz hernia.
The cavity of the peritoneum. Division into floors. Subdiaphragmatic spaces. Pregastric and omental bags. Operative accesses to the cavity of the omental bag.
The peritoneal cavity is the part of the abdominal cavity that is bounded by
parietal peritoneum. The peritoneum is a serous
shell that covers the inner surface of the walls
abdomen and organs located in it, forming a closed cavity. IN
connection with this distinguish parietal, or parietal, peritoneum,
peritoneum parietale, and visceral, or visceral, peritoneum,
peritoneum viscerale. Intraperitoneally, or intraperitoneally, located
the underlying organs are covered with visceral peritoneum on all sides,
mesoperitoneally - on three sides and extraperitoneally - on one side
sides. The space between the peritoneal surfaces of individual
organs and the parietal sheet - the abdominal cavity. Normally, she has
the nature of the gap filled with serous fluid. men have a cavity
the peritoneum is closed, in women through the fallopian tubes it communicates with
uterine cavity. It is conditionally divided into two floors - upper and lower.
The border between them is the transverse colon with its
mesentery, mesocolon transversum. In the upper abdomen
located liver with gallbladder, stomach, spleen, upper
half of the duodenum, pancreas and four
practically important spaces: the right and left subdivisions
aphragmatic, pregastric, subhepatic, as well as omental
bag. Lower half of the duodenum, small and large
intestine occupy the lower floor of the abdominal cavity. In addition, in it you
divide two lateral peritoneal canals (right and left) and two mesenteric
echny - mesenteric sinuses (right and left). Right subdiaph-
ragmal space , or right liver bag, bursa hepatica
dextra, limited above and in front by the diaphragm, below by the upper back
surface of the right lobe of the liver, behind - the right coronary and right
triangular ligament of the liver, on the left - falciform ligament of the liver.
Inflammatory exudate rises here most often on the right
lateral canal from the right iliac fossa or from the subhepatic
spaces along the outer edge of the liver. Left subphrenic
space consists of two widely communicating with each other
departments: pregastric bag, bursa pregastrica, and left hepatic
bags, bursa hepatica sinistra. Space between the left lobe of the liver
below and diaphragm above and in front, bursa hepatica sinistra, on the right
limited to the falciform ligament, behind - the left part of the coronary
ligament and the left triangular ligament of the liver. Pregastric bag ,
bursa pregastrica, bounded behind by the lesser omentum and stomach,
front and top - the diaphragm, the left lobe of the liver and the anterior abdomen
wall, on the right - crescent and round ligaments of the liver. late-
the oral section of bursa pregastrica, located outward from the large
curvature of the stomach and enclosing the spleen, limited to the left and
behind lig. phrenicolienale, from above - lig. gastrolienale and diaphragm, below
Lig. phrenicocolicum. The left subdiaphragmatic space is separated
but from the left lateral canal of the well-defined left diaphragmatic
but-colic ligament, lig. phrenicocolicum sinistrum, and free
has no communication with him. Occurs in the left subphrenic
space abscesses as a result of complications of perforated gastric ulcers
ka, purulent liver diseases, etc. can spread to the left in
blind sac of the spleen, and in front to fall between the anterior wall
stomach and the upper surface of the left lobe of the liver to the transverse
colon and below. Subhepatic __________ space, bursa subhepatica,
located between the inferior surface of the right lobe of the liver and
mesocolon with the transverse colon, to the right of the hilum of the liver and
gland hole. Divided into anterior and posterior sections. IN
the anterior part of this space faces almost the entire peritoneal
the surface of the gallbladder and the upper outer surface of the twelfth
duodenal ulcer. The posterior section, located at the posterior edge of the liver
nor, to the right of the spine, the hepato-renal pouch. Abscesses
resulting from perforated duodenal ulcers
or purulent cholecystitis, are located more often in the anterior section;
periappendicular abscess extends predominantly into
posterior subhepatic space. Stuffing bag, bursa
omentalis, is located behind the stomach, looks like a gap and is
the most isolated space of the upper floor of the abdominal
cavities. It is limited in front of the hepatoduodenal
ligament, lig. hepatoduodenale, behind - parietal peritoneum, covered with
waving v. cava inferior, and hepatic-renal ligament, lig, hepatorenale;
above - the caudate lobe of the liver and below - the renal
duodenal, ligament, lig. duodenorenale, and pars superior duodeni.
In you can select the anterior, posterior, upper, lower and left
walls, and on the right - the vestibule of the omental bag. vestibule of the sebaceous
bag, vestibulum bursae omentalis, its rightmost part, located
lies behind the hepatoduodenal ligament and is limited
from above the caudate lobe of the liver and the peritoneum covering it, from below -
duodenum, behind - parietal peritoneum, covered
enclosing the inferior vena cava. The front wall of the stuffing bag
are the lesser omentum (lig. hepatogastricum and lig. hepatoduodenale),
back wall of the stomach and lig. gastrocolicum; posterior - parietal
sheet of peritoneum covering here the pancreas, aorta,
inferior vena cava and nerve plexuses of the superior abdominal
cavities; upper - caudate lobe of the liver and partly the diaphragm;
lower - mesentery of the transverse colon; left - spleen
and its ligaments - lig. gastrolienale et phrenicolienale.
Operative accesses to the omental bag are more often carried out
by dissection lig. gastrocolicum closer to the left flexure of the colon
intestines, through mesocolon transversum.
Pancreas located retroperitoneally, behind the stomach, in
upper half of the abdomen. Functionally and anatomically, it is associated with
duodenum, liver and stomach. pancreas
gland is projected onto the anterior abdominal wall along a horizontal
line connecting the ends of the VII-VIII ribs, or along a horizontal
line passing through the middle of the distance between the xiphoid
process and navel, which corresponds to the level of the body of the I lumbar
vertebra. The shape can be elongated, arched, youthful
shaped and angular. The pancreas is conditionally divided
into three sections: head, body and tail, neck of the gland. The head of the
the gland is thickened and approaches in shape to an irregular
quadrilateral; occupying the inner flexure of the duodenum
intestines, it is firmly fixed together with the common bile and pancreas
daughter ducts to its descending part. In the anterior-posterior direction
the head is flattened. It distinguishes between anterior and posterior
top, as well as the top and bottom edges. Body of the pancreas
represents the middle, largest part of the body. Right side front
its surface protrudes somewhat forward, forming an omental
tubercle, tuber omentale pancreatis. On the back surface is
longitudinal recess for the splenic vein passing here. Tail
pancreas is flattened and has no facets. It distinguishes
front and back surfaces, as well as the top and bottom edges.
Its shape is usually cone-shaped or pear-shaped. output system
pancreas contains small lobular ducts
flow into the main and accessory pancreatic ducts. Duct
pancreas, ductus pancreaticus, is formed by the fusion
lobular ducts of most of the organ and can be traced for
the entire gland, located at an equal distance from the upper and
its lower edges. In the region of the major duodenal papilla, it
unites with the common bile duct or opens on its own.
At the junction, the pancreatic duct has its own
smooth muscle sphincter. accessory pancreatic duct
PS, ductus pancreaticus accessorius, located in the upper anterior
parts of the head of the gland. It connects with the main duct in the head,
empties independently on the minor duodenal papilla
duodenal ulcer. Allocate gastro-pancreas, pyloric
in the pancreas and pancreas-splenic ligaments. Blood supply
compression of the head of the pancreas is carried out mainly
from the anterior and posterior arterial arches formed by the two upper
(from a. gastroduodenalis) and two lower ones (from the initial section of a. mesenterica
superior) pancreatoduodenal arteries. body and tail
pancreas are supplied with blood from rr. pancreatici from spleen-
nocturnal artery. The outflow of venous blood occurs directly in
portal vein and its main tributaries - vv. lienalis and mesenterica
superior. Regional lymph nodes of the first stage for
pancreas are pyloric, pancreatoduodenal-
nye, upper and lower pancreas, as well as splenic nodes.
Lymph nodes of the second stage are pre-aortic,
lateral caval, postcaval, located at the level of the gate
both kidneys. The sources of innervation of the gland are the celiac,
hepatic, superior mesenteric, splenic and left renal plexus
niya. The nerve plexuses of the pancreas are
powerful reflexogenic zone, the irritation of which can cause
shock state.
After opening the abdominal cavity, the gland can be approached
in three ways. 1. Through the gastrocolic ligament, for which it
cut in the avascular area, closer to the greater curvature
stomach. Penetrating into the stuffing bag, they move the stomach back to the
xy, and the transverse colon with its mesentery - from top to bottom. 2.Through
mesentery of the transverse colon. 3. By separating a large
omentum from the transverse colon. In addition, it applies
access through the lesser omentum by dissection of the hepato-
gastric __________ ligament between the lower edge of the liver and the lesser curvature
formations, except for:
1) liver bag
2) subhepatic space
3) pelvic cavity
4) cavities of the stuffing bag
5) right mesenteric sinus
8.025. The left lateral abdominal canal communicates with:
1) liver bag
2) subhepatic space
3) pelvic cavity
4) Cavity stuffing bag
5) left mesenteric sinus
8.026. The small omentum consists of the following three ligaments:
1) diaphragmatic-gastric
2) gastro-splenic
3) gastrointestinal
4) hepatoduodenal
5) hepatic-gastric
8.027. In relation to the spinal column, the gallbladder is located at the level of the vertebra:
1) X chest
2) XI chest
3) XII chest
4) I lumbar
5) II lumbar
8.028. All structures are adjacent to the gallbladder, except:
2) pylorus of the stomach
3) hepatic flexure of the transverse colon
4) head of the pancreas
5) ascending duodenum
8.029. Knowledge of the constituent sides of the Calot triangle is necessary when performing:
1) cholecystostomy
2) cholecystojejunoanastomosis
3) cholecystoduodenoanastomosis
4) cholecystectomy
5) liver resection
8.030. Set the appropriate anatomical formations that form the walls of the omental sac:
1) upper A) mesentery of the transverse colon
2) lower B) stomach
3) anterior B) gastrocolic ligament
4) back D) small gland
D) posterior parietal peritoneum
E) transverse colon
G) caudate lobe of the liver
8.031. All formations are adjacent to the back wall of the stomach, except:
1) left lobe of the liver
2) posterior leaf of the parietal peritoneum
3) pancreas
4) spleen
5) abdominal aorta
8.032. All formations are adjacent to the stomach in front, except:
1) left lobe of the liver
2) transverse colon
3) right lobe of the liver
4) anterior abdominal wall
5) small intestine
8.033. Set the appropriate anatomical formations that form the boundaries of the omental opening:
1) upper A) hepatoduodenal ligament
2) inferior B) hepato-renal ligament and inferior vena cava
3) anterior B) renal-duodenal ligament and
duodenum
D) caudate lobe of the liver
8.034. In a patient with a perforated ulcer of the posterior wall of the stomach, the gastric contents appeared in the right iliac fossa near the caecum, where it caused symptoms simulating an attack of appendicitis. Specify 4 formations that make up the sequential path of gastric contents entry into this area:
1) subhepatic fissure
2) right side channel
3) right mesenteric sinus
4) pregastric bag
5) stuffing bag
6) gland hole
7) gap in front of the transverse colon
8.035. Of the four peritoneal formations of the lower floor of the abdominal cavity, it freely communicates with the peritoneal bags of the upper floor:
1) left mesenteric sinus
2) left side channel
3) right mesenteric sinus
4) right side channel
8.036. Messages from the right and left mesenteric sinuses:
1) between the loops of the small intestine and the anterior abdominal wall
2) through a hole in the root of the mesentery of the small intestine
3) through holes in the mesentery of the transverse colon
4) between the beginning of the root of the mesentery of the small intestine and the mesentery of the transverse colon
5) not reported
8.037. Of the four peritoneal formations of the lower floor of the abdominal cavity, one does not communicate with the peritoneal floor of the small pelvis:
1) left mesenteric sinus
2) left side channel
3) right mesenteric sinus
4) right side channel
8.038. The most likely route for the spread of purulent peritonitis from the right mesenteric sinus is:
2) left mesenteric sinus
3) left side channel
4) right side channel
5) peritoneal floor of the small pelvis
8.039. The most likely ways of spreading purulent peritonitis from the left mesenteric sinus are two:
1) the upper floor of the abdominal cavity
2) left side channel
3) right mesenteric sinus
4) right side channel
5) peritoneal floor of the small pelvis
8.040. The lateral border of the right mesenteric sinus is:
1) the root of the mesentery of the sigmoid colon
2) the root of the mesentery of the small intestine
3) medial edge of the ascending colon
4) right side wall of the abdomen
5) lateral edge of the ascending colon
8.041. The most likely ways of spreading purulent peritonitis from the right lateral canal are two:
1) liver bag
2) left mesenteric sinus
3) left side channel
4) right mesenteric sinus
5) peritoneal floor of the small pelvis
8.042. The most likely route for the spread of purulent peritonitis from the left lateral canal is:
1) the upper floor of the abdominal cavity
2) left mesenteric sinus
3) right mesenteric sinus
4) right side channel
5) peritoneal floor of the small pelvis
Intra-abdominal hernias can occur in the following three
In places of the lower floor of the abdominal cavity, in accordance with the
position of the abdominal pockets:
1) behind the duodenal lean bend
2) in the region of the ileocecal angle
3) in the area of the hepatic flexure of the colon
4) in the area of the splenic flexure of the colon
5) behind the mesentery of the sigmoid colon
6) in front of the mesentery of the sigmoid colon
In a patient, purulent appendicitis was complicated by the formation
Peritoneum, peritoneum, is called a thin serous membrane that lines the inner surface of the walls of the abdominal cavity and the internal organs that are in it. Its total area is on average 2 m2.
If we trace the further course of the peritoneum on the anterior and upper abdominal walls, it turns out that it passes to the diaphragmatic surface, forming a crescent-shaped ligament, lig.falciforme hepatis, in the free edge of which there is a round ligament of the liver, lig. teres hepatis. From the lower surface of the diaphragm behind the falciform ligament, the peritoneum wraps onto the diaphragmatic surface of the liver, forming the coronary ligament of the liver, lig. coronarium hepatis, which has the shape of triangular plates, or triangular ligaments, lig. triangulare dextrum et sinistrum.
From the diaphragmatic surface of the liver, the peritoneum through its lower edge passes to the visceral surface, from where it gives a number of ligaments to the internal organs: to the kidney - lig. hepatorenal, lesser curvature of the stomach - lig. hepatogastricum, into the duodenum - lig. hepatoduodenal. Lig. hepatoduodenale, lig. hepatogastricum and lig. phrenicogastricum together form the lesser omentum, omentum minus. Hepatoduodenal ligament, lig. hepatoduodenale, connecting the gate of the liver with the initial section of the duodenum. In this bundle they pass from right to left - ductus choledochus, v. portae, a. hepatica propria (according to the anatomical code (TWO) - ductus, vena, arteria), as well as lymphatic vessels and nerves. This is important to consider when performing surgical interventions on the extrahepatic bile ducts.
On the lesser curvature of the stomach, the leaves of the lesser omentum diverge and cover the anterior and posterior surfaces of the stomach. On the greater curvature of the stomach, these sheets converge and descend in front of the transverse colon and small intestine, forming the anterior plate of the greater omentum, omentum majus. The leaves of the greater omentum go down, after which they wrap up, forming its back plate. Thus, the greater omentum is formed by four sheets of peritoneum. The posterior plate of the greater omentum, reaching the transverse colon and its mesentery, fuses with them, and then together they go dorsally to the pancreas, where the sheets diverge. One leaf covers and goes up to the diaphragm, and the second one covers the lower surface of the gland and passes into the mesentery, colon transversum.
The organs that lie in the abdominal cavity have a different relationship to the peritoneum.
If the organ is covered with peritoneum from all sides, then its relation to the peritoneum is called intraperitoneal; if the organ is covered with peritoneum on three sides, this relationship is called mesoperitoneal; if the organ is covered by the peritoneum on one side, then this relationship is called extraperitoneal.
When the visceral peritoneum passes from one organ to another or in the parietal or vice versa, the peritoneum forms ligaments, folds, a cap, as well as grooves, depressions, pits, sinuses, bags. Abdomen, cavum abdominis, - is conditionally divided into three levels: upper, middle and lower.
1. Top level bounded above by the diaphragm, below by the transverse colon and its mesentery. It contains the stomach, liver and spleen.
2. Average level occupies the area from the mesentery of the transverse colon, mesocolon transversum to the entrance to the small pelvis. It contains the empty and ileum, ascending, descending and caecum with appendix.
3. Lower level extends from the entrance to the small pelvis to the pelvic diaphragm, deepening its cavity. It contains the rectum, bladder, ureters, prostate, seminal vesicles in men, and in women, the uterus and ovaries.
1. For the organs of the upper level, the peritoneum forms three bags, bursae (D. N. Zernov): hepatic, bursa hepatica; preventricular, bursa pregastrica; and omental, bursa omentalis.
Liver bag, bursa hepatica, - located under the diaphragm and separated from the perventricular sac by the falciform ligament, behind it is limited by the coronary ligament, lig. coronarium hepatis. The liver bag contains the right lobe of the liver, and in the depth of the bag under the liver, the upper pole of the right kidney and adrenal glands is palpated.
preventricular sac, bursa pregastrica, - located in front of the liver and spleen under the diaphragm. It contains the left lobe of the liver, the spleen and the anterior surface of the stomach, it has a deep space around the spleen.
Stuffing bag, bursa omentalis, - located behind the stomach and lesser omentum, omentum minus, formed by three ligaments of the peritoneum: hepatogastric, lig. hepatogastricum, which goes from the gate of the liver to the lesser curvature of the stomach and hepatoduodenal, lig. hepatoduodenale, connecting the gates of the liver with the pars superior duodeni. The stuffing bag is limited by the anterior wall, which is formed by the lesser omentum, the posterior wall of the stomach and the gastrocolic ligament, lig. gastrocolicum.
The posterior wall is formed by the parietal sheet of the peritoneum; upper - the lower surface of the caudal lobe of the liver and the diaphragm; lower - mesocolon transversum et colon transversum. The left wall of the stuffing bag is formed by ligaments of the spleen: lig. gastrolienal et colon transverrsum and lig. phrenicosplenicum.
The stuffing bag communicates with the peritoneal cavity through the stuffing hole, foramen omentale (Winslowi), which is limited: in front - lig. hepatoduodenal; behind - lig. hepatorenale; below - lig. duodenorenale and from above - the caudate lobe of the liver. In the omental bag, a parietal, upper and lower splenic recesses are distinguished. During surgical interventions, the surgeon can enter the stuffing box through the stuffing hole in order to revise it.
Big omentum, omentum majus, - in the form of an apron covers the loops of the small intestine in front. It is formed by four sheets of peritoneum, which have grown together in the form of plates. The anterior plate is formed by two sheets of peritoneum that go down from the greater curvature of the stomach and, passing in front of the transverse colon, grow together with it, forming the gastrocolic ligament, lig. gastrocolicum. The anterior plate descends to the level of the pubic bones and then wraps around to form the posterior plate of the greater omentum. Between the sheets of the anterior and posterior plates of the omentum there is a slit-like cavity, which communicates with the cavity of the omental bag, however, in adults, the omentum cavity is partially obliterated.
2. The middle level of the peritoneal cavity can be seen by lifting the greater omentum and transverse colon upward. Four departments are distinguished at the middle level: the right and left lateral canals, canalis lateralis dexter et sinister, which pass between the lateral walls of the abdomen and the ascending and descending intestines, as well as two mesenteric sinuses, sinus mesentericus dexter et sinister, formed as a result of the division of the middle floor of the mesentery of the small intestine, which runs obliquely from top to bottom, from left to right. The left and right sinuses are separated from each other by the root of the mesentery of the small intestine and are combined with the small pelvis.
Mesentery, mesenterium, is a fold formed by two sheets of the peritoneum, through which the small intestine is attached to the posterior wall of the abdominal cavity. The posterior edge of the mesentery is its root, radix mesenterii, which originates on the left side of the II lumbar vertebra and runs in an oblique direction to the right iliac fossa. The root of the mesentery, when moving, crosses the end section of the duodenum, the aorta, the inferior vena cava, the right ureter, and the psoas major muscle.
Between the serous sheets of the mesentery contains adipose tissue, lymph nodes, blood and lymphatic vessels and nerves pass. On the posterior parietal sheet of the peritoneum there are a number of pits that are of practical importance, since internal abdominal hernias of the retroperitoneal type can sometimes form in them. At the place where the duodenum passes into the empty one, small depressions are formed, recessus duodenalis superior et inferior. In the area of the transition of the small intestine into the thick above and below the ileocecal fold, plica ileoceacalis, there are two depressions: recessus ileoceacalis superior et inferior. At the location of the caecum, the parietal sheet of the peritoneum forms a recess - the fossa of the caecum, or the caecal recess, recessus retrocaeacalis. In the fossa behind the caecum there is sometimes an opening leading to the caecal cavity.
3. The peritoneum of the lower level covers its walls and organs that are located in it, depending on the sex. and the initial section of the rectum are covered with peritoneum from all sides (intraperitoneally) and have their own mesentery. The middle section, the rectum, is covered with the peritoneum in front and on the sides, the posterior surface remains not covered with the peritoneum, and even lower, at a distance of 7.5-8 cm from the anus, the peritoneum, passing from the anterior surface of the rectum to the posterior surface of the bladder, forms a rectovesical depression, excavatio rectovesical. A feature of the peritoneum in men is that part of the serous sac is isolated in the scrotum, covering each testicle separately. In the process of development, a finger-shaped sac protrudes through the inguinal canal into the scrotum - the vaginal process, processus vaginalis, which in 99% of cases overgrows, except for the distal section. Thus, two serous sacs remain in the scrotum, in which serous fluid accumulates during inflammation of the testicle (orchitis).
In women, the uterus is located between the bladder and rectum. It is covered with peritoneum on all sides, so there are two recesses in the pelvic cavity of women: recto-uterine, excavatio recto-uterina (between the rectum and uterus), and vesico-uterine, excavatio vesicouterina (between the uterus and bladder). Excavatio rectouterina, or Douglas' deepening (Douglasi) is of practical importance: blood, pus or serous fluid accumulates in it during inflammatory conditions and bleeding in the abdominal cavity, therefore, in clinical (gynecological) practice, this deepening is punctured for diagnostic purposes. On the sides of the uterus, the peritoneum passes to the walls of the small pelvis, forming a wide uterine ligament, lig. latum uteri, located transversely in the pelvic cavity and divides it into anterior and posterior sections.
In both sexes, in the umbilical region, regio pubica, there is a prostatic cellular space, spatium prevesicale (cavum Retzii), bounded in front by the transverse fascia, fascia transversalis, and behind by the bladder and peritoneum. The space is filled with fatty tissue, venous plexus of the bladder and prostate, and arteries supplying the bladder. Through the prostate space, access to the bladder is carried out during the operation of suprapubic high opening of the bladder. The prostate is a place where blood accumulates (in case of fractures of the pubic bones) and urine (in case of injury to the bladder). All this is of great importance in clinical (urological) practice. Therefore, when the bladder is full, the peritoneum rises, and the bladder is adjacent to the anterior abdominal wall, which allows in clinical (surgical) practice to puncture the bladder (with a Beer needle or trocar) above the symphysis.
Within the lower level of the abdominal cavity, the peritoneum forms pits and folds. On the posterior surface of the anterior abdominal wall, five umbilical folds stretch from the navel to the bladder: median, plicae umbilicalis mediana, two medial, plicae umbilicales mediates, two lateral, plicae umbilicales laterals. In the median umbilical fold is the dewy urinary duct, urachus; in the medial - umbilical arteries, and in the lateral - aa. epigastricae inferiores (branches of a. iliaca externa). On the sides of the median umbilical fold are supra-cystic fossae, fossae supravesicales. Between the medial and lateral folds on each side are the medial inguinal fossae, fossae inguinales mediates, and outside of the lateral folds are the lateral fossae, fossae inguinales laterales. the lateral inguinal fossa coincides with the deep inguinal ring, and the medial one with the superficial one; inguinal hernias can exit through these pits, which is important in clinical (surgical) practice.
blood supply The peritoneum is carried out by branches (arteries) of the abdominal aorta: the inferior diaphragmatic, superior and inferior mesenteric, anterior and posterior caecal, adrenal, renal and lumbar arteries. Venous blood flows into the system of the superior and inferior vena cava and into the portal vein.
Lymph drainage from the peritoneum it passes through the lymphatic capillaries with a superficial and deep lymphatic network (L. V. Chernyshenko, A. M. Sinitskaya, 1982), after which the lymph penetrates through the hatches into the lymphatic vessels of the peritoneum.
innervation The peritoneum is carried out by the superficial nerve plexus, which is located in the peritoneum above the elastic meshes, and the deep nerve plexus, which is located in the deep cribriform collagen-elastic layer.
Peritoneum, peritoneum, represents a closed serous sac, which only in women communicates with the outside world through a very small abdominal opening of the fallopian tubes. Like any serous sac, the peritoneum consists of two sheets: parietal, parietal, peritoneum parietale, and visceral, peritoneum viscerale. The first lines the abdominal walls, the second covers the insides, forming their serous cover over a greater or lesser extent. Both sheets are in close contact with each other, between them, with an unopened abdominal cavity, there is only a narrow gap called the peritoneal cavity, cavitas peritonei, which contains a small amount of serous fluid, moisturizing the surface of the organs and thus facilitating their movement around each other. When air enters during an operation, or an autopsy, or when pathological fluids accumulate, both sheets diverge and then the peritoneal cavity takes the form of a real, more or less voluminous cavity.
Parietal peritoneum lines the anterior and lateral walls of the abdomen with a continuous layer from the inside and then continues to the diaphragm and the posterior abdominal wall. Here it meets the viscera and, wrapping itself on the latter, directly passes into the visceral peritoneum covering them. Between the peritoneum and the walls of the abdomen there is a connective tissue layer, usually with a greater or lesser content of adipose tissue, tela subserosa, - subperitoneal fiber, which is not equally pronounced everywhere. In the region of the diaphragm, for example, it is absent; on the back wall of the abdomen, it is most developed, covering the kidneys, ureters, adrenal glands, abdominal aorta and inferior vena cava with their branches.

Along the anterior abdominal wall, for a large extent, the subperitoneal tissue is weakly expressed, but below, in the regio pubica, the amount of fat in it increases, the peritoneum here connects to the abdominal wall more loosely, due to which the bladder, when stretched, pushes the peritoneum away from the anterior abdominal wall and its anterior surface at a distance of about 5 cm above the pubis comes into contact with the abdominal wall without the mediation of the peritoneum. The peritoneum in the lower part of the anterior abdominal wall forms five folds converging to the navel, umbilicus; one median unpaired, plica umbilicalis mediana, and two paired, plicae umbilicales mediales and plicae umbilicales laterales. These folds delimit on each side above the inguinal ligament two fossae inguinales related to the inguinal canal. Immediately below the medial part of the inguinal ligament is the fossa femoralis, which corresponds to the position of the inner ring of the femoral canal.
Up from the navel, the peritoneum passes from the anterior abdominal wall and diaphragm to the diaphragmatic surface of the liver in the form of a falciform ligament, lig. falciforme hepatis, between the two leaves of which in its free edge is laid a round ligament of the liver, lig. teres hepatis (overgrown umbilical vein). The peritoneum behind the falciform ligament from the lower surface of the diaphragm wraps onto the diaphragmatic surface of the liver, forming the coronary ligament of the liver, lig. coronarium hepatis, which at the edges looks like triangular plates, called triangular ligaments, lig. triangulare dextrum et sinistrum.
From the diaphragmatic surface of the liver, the peritoneum through the lower sharp edge of the liver bends to the visceral surface; from here it departs from the right lobe to the upper end of the right kidney, forming lig. hepatorenale, and from the gate - to the lesser curvature of the stomach in the form of a thin lig. hepatogastricum and on the part of the duodeni closest to the stomach in the form of lig. hepatoduodenale. Both of these ligaments are duplications of the peritoneum, since two layers of the peritoneum meet in the region of the gate of the liver: one - going to the gate from the front of the visceral surface of the liver, and the second - from its back. Lig. hepatoduodenale and lig. hepatogastricum, being a continuation of one another, together make up the lesser omentum, omentum minus. On the lesser curvature of the stomach, both sheets of the lesser omentum diverge: one sheet covers the anterior surface of the stomach, the other - the back. On the greater curvature, both sheets converge again and descend down in front of the transverse colon and loops of the small intestine, forming the anterior plate of the greater omentum, omentum majus. Going down, the leaves of the greater or lesser height are wrapped back up, forming its back plate (the greater omentum, thus, consists of four leaves). Having reached the transverse colon, the two sheets that make up the posterior plate of the greater omentum fuse with the colon transversum and with its mesentery and, together with the latter, then go back to the margo anterior of the pancreas; from here the leaves diverge; one is up, the other is down. One, covering the anterior surface of the pancreas, goes up to the diaphragm, and the other, covering the lower surface of the gland, passes into the mesentery of the colon transversum. In an adult, with complete fusion of the anterior and posterior plates of the greater omentum with the colon transversum on the tenia mesocolica, 5 sheets of the peritoneum are thus fused: four sheets of the omentum and the visceral peritoneum of the intestine. Let us now trace the course of the peritoneum from the same sheet of the anterior abdominal wall, but not in the upward direction to the diaphragm, but in the transverse direction.

From the anterior abdominal wall, the peritoneum, lining the lateral walls of the abdominal cavity and passing to the posterior wall on the right, surrounds the caecum with its appendix on all sides; the latter receives the mesentery - mesoappendix. The peritoneum covers the colon ascendens in front and from the sides, then the lower part of the anterior surface of the right kidney, passes in the medial direction through m. psoas and ureter and at the root of the mesentery of the small intestine, radix mesenterii, folds into the right leaf of this mesentery. Having supplied the small intestine with a complete serous cover, the peritoneum passes into the left leaf of the mesentery; at the root of the mesentery, the left sheet of the latter passes into the parietal sheet of the posterior abdominal wall, the peritoneum further covers the lower part of the left kidney to the left and approaches the colon descendens, which belongs to the peritoneum, as well as the colon ascendens; further, the peritoneum on the lateral wall of the abdomen is again wrapped on the anterior abdominal wall. The entire peritoneal cavity, in order to facilitate the assimilation of complex relationships, can be divided into three areas, or floors:
- the upper floor is bounded from above by the diaphragm, from below by the mesentery of the transverse colon, mesocolon transversum;
- the middle floor extends from the mesocolon transversum down to the entrance to the small pelvis;
- the lower floor starts from the line of entry into the small pelvis and corresponds to the cavity of the small pelvis, which ends downward with the abdominal cavity.
Upper floor of the peritoneal cavity breaks up into three bags: bursa hepatica, bursa pregastrica and bursa omentalis. Bursa hepatica covers the right lobe of the liver and is separated from bursa pregastrica by means of lig. falciforme hepatis; behind it is limited lig. coronarium hepatis.

In the depths of the bursa hepatica, iodine by the liver, the upper end of the right kidney with the adrenal gland is palpated. Bursa pregastrica covers the left lobe of the liver, the anterior surface of the stomach and spleen; the left part of the coronary ligament passes along the posterior edge of the left lobe of the liver; the spleen is covered on all sides by the peritoneum, and only in the region of the gate does its peritoneum pass from the spleen to the stomach, forming lig. gastrolienale, and on the diaphragm - lig. phrenicolienale.

Bursa omentalis, stuffing bag, is a part of the common cavity of the peritoneum, lying behind the stomach and lesser omentum. The composition of the lesser omentum, omentum minus, includes, as indicated, two ligaments of the peritoneum: lig. hepatogastricum, running from the visceral surface and the gate of the liver to the lesser curvature of the stomach, and lig. hepatoduodenale, connecting the gates of the liver with the pars superior duodeni. Between leaves lig. hepatoduodenale pass the common bile duct (right), common hepatic artery (left) and portal vein (posteriorly and between these formations), as well as lymphatic vessels, nodes and nerves. The cavity of the omental bag communicates with the common cavity of the peritoneum only through a relatively narrow foramen epiploicum. Foramen epiploicum is bounded above by the caudate lobe of the liver, in front by the free edge of lig. hepatoduodenale, from below - by the upper part of the duodenum, from behind - by a sheet of peritoneum covering the inferior vena cava passing here, and more outwards - by a ligament passing from the posterior edge of the liver to the right kidney, lig. hepatorenale. Part of the stuffing bag, directly adjacent to the stuffing hole and located behind lig. hepatoduodenale, is called the vestibule - vestibulum bursae omentalis; it is bounded above by the caudate lobe of the liver, and below by the duodenum and head of the pancreas. The lower surface of the caudate lobe of the liver serves as the upper wall of the stuffing bag, and the processus papillaris hangs in the bag itself.

The parietal sheet of the peritoneum, which forms the posterior wall of the omental sac, covers the aorta, inferior vena cava, pancreas, left kidney and adrenal gland located here. Along the anterior edge of the pancreas, the parietal sheet of the peritoneum departs from the pancreas and continues forward and downward as the anterior sheet of the mesocolon transversum or, more precisely, the posterior plate of the greater omentum, fused with the mesocolon transversum, forming the lower wall of the omental bag. The left wall of the stuffing bag is made up of ligaments of the spleen: gastro-splenic, lig. gastrolienale, and diaphragmatic-splenic, lig. phrenicosplenicum. The greater omentum, omentum majus, hangs down from the colon transversum in the form of an apron, covering the loops of the small intestine for a greater or lesser extent; It got its name from the presence of fat in it. It consists of 4 sheets of peritoneum, fused in the form of plates. The anterior plate of the greater omentum is served by two sheets of peritoneum extending downward from the greater curvature of the stomach and passing in front of the colon transversum, with which they fuse, and the transition of the peritoneum from the stomach to the colon transversum is called lig. gastrocolicum. These two sheets of the omentum can descend in front of the loops of the small intestine almost to the level of the pubic bones, then they are bent into the posterior plate of the omentum, so that the entire thickness of the greater omentum consists of four sheets; with loops of small intestines, the leaves of the omentum do not normally grow together. Between the sheets of the anterior plate of the omentum and the leaves of the posterior there is a slit-like cavity that communicates with the cavity of the omental bag at the top, but in an adult the leaves usually fuse with each other, so that the cavity of the greater omentum is obliterated over a large extent. Along the greater curvature of the stomach, the cavity sometimes continues in an adult for a greater or lesser extent between the leaves of the greater omentum. In the thickness of the greater omentum, there are lymph nodes, nodi lymphatici omentales, which drain lymph from the greater omentum and the transverse colon.

Middle floor of the peritoneal cavity becomes available for review if the greater omentum and transverse colon are raised upward.
Using the ascending and descending colons on the sides and the mesentery of the small intestines in the middle as boundaries, it can be divided into four sections: between the lateral walls of the abdomen and the colon ascendens and descendens are the right and left lateral canals, canales laterales dexter et sinister; the space covered by the colon is divided by the mesentery of the small intestine, going obliquely from top to bottom and from left to right, into two mesenteric sinuses, sinus mesentericus dexter and sinus mesentericus sinister. On the posterior parietal sheet of the peritoneum, a number of peritoneal pits are noted, which are of practical importance, since they can serve as a site for the formation of retroperitoneal hernias. At the point of transition of the duodenum into the jejunum, small pits are formed - depressions, recessus duodenalis superior et inferior. These pits are limited on the right by the bend of the intestinal tube, flexura duodenojejunalis, on the left by the fold of the peritoneum, plica duodenojejunalis, which goes from the top of the bend to the posterior abdominal wall of the abdomen immediately below the body of the pancreas and contains v. mesenterica inferior.

In the area of transition of the small intestine into the large intestine, there are two pits: recessus ileocaecalis inferior et superior, below and above the plica ileocaecalis, passing from the ileum to the medial surface of the caecum. The deepening of the parietal sheet of the peritoneum, in which the caecum lies, is called the fossa of the caecum and is noticeable when the caecum and the nearest section of the ileum are pulled upwards. The resulting fold of the peritoneum between the surface of m. iliacus and the lateral surface of the caecum is called plica caecalis. Behind the caecum, in the fossa of the caecum, there is sometimes a small opening leading to the recessus retrocaecalis, extending upward between the posterior abdominal wall and the colon ascendens. On the left side there is a recessus intersigmoideus; this fossa is noticeable on the lower (left) surface of the mesentery of the sigmoid colon, if you pull it up. Lateral to the descending colon, sometimes there are peritoneal pockets - sulci paracolici. Above, between the diaphragm and flexura coli sinistra, there is a fold of the peritoneum, lig. phrenicocolicum; it is located just under the lower end of the spleen and is also called the splenic sac.

Lower floor. Descending into the cavity of the small pelvis, the peritoneum covers its walls and the organs lying in it, including the genitourinary ones, so the relationship of the peritoneum here depends on gender. The pelvic section of the sigmoid colon and the beginning of the rectum are covered with peritoneum on all sides and have a mesentery (located intraperitoneally). The middle section of the rectum is covered with peritoneum only from the anterior and lateral surfaces (mesoperitoneally), and the lower one is not covered by it (extraperitoneally). Passing in men from the anterior surface of the rectum to the posterior surface of the bladder, the peritoneum forms a recess located behind the bladder, excavatio rectovesicale. With an unfilled bladder, on its upper posterior surface, the peritoneum forms a transverse fold, plica vesicalis transversa, which is smoothed out when the bladder is filled.
In women, the course of the peritoneum in the pelvis is different due to the fact that between the bladder and the rectum is the uterus, which is also covered by the peritoneum. As a result, in the pelvic cavity in women there are two peritoneal pockets: excavdtio rectouterina - between the rectum and the uterus and excavatio vesicouterina - between the uterus and the bladder. In both sexes, there is a prevesical space, spatium prevesicale, formed in front of the fascia transversalis, covering the back of the transverse abdominal muscles, and the bladder and peritoneum behind. When the bladder is filled, the peritoneum moves upward, and the bladder is adjacent to the anterior abdominal wall, which allows it to penetrate into the bladder through its anterior wall during surgery without damaging the peritoneum. The parietal peritoneum receives vascularization and innervation from parietal vessels and nerves, and the visceral peritoneum receives blood vessels and nerves branching in the organs covered by the peritoneum.