How does ureaplasma affect the fetus? What are the dangers of ureaplasma during pregnancy and how to get rid of the infection
If you have planned a pregnancy, then you must undergo all examinations and tests. This is required to identify various infections and diseases that can harm the child and lead to complications. As a rule, these are infectious diseases of the genital tract, and ureaplasmosis is one of them. Having learned about the pathology before conception, you can undergo the required treatment and get rid of the infection. But this doesn't always happen. Taking into account statistics, the majority of people suffer from an asymptomatic and latent form of ureaplasmosis, without even knowing about it. So, a woman’s problem is often identified already during pregnancy.
It is impossible to ignore the infection, since it threatens with serious consequences, but antibiotics, which need to treat the disease, can also negatively affect the formation of the fetus.
Causes of ureaplasma
 Ureaplasma its properties appear only under favorable conditions or if their concentration exceeds a certain threshold in the body. These bacteria combine with other pathogenic organisms, affecting the genitourinary system, which causes various inflammations and diseases.
Ureaplasma its properties appear only under favorable conditions or if their concentration exceeds a certain threshold in the body. These bacteria combine with other pathogenic organisms, affecting the genitourinary system, which causes various inflammations and diseases.
The microflora of a woman’s vagina consists of various types of microorganisms. Their main part is lactobacilli (about 90%), and the remaining few percent are occupied by other types of bacteria. Among which there may be opportunistic ones.
If your body is functioning normally and is healthy, you will not notice the presence of these bacteria. But during nervous shocks, severe stress or decreased immunity, due to some other reasons, pathogenic organisms appear, beginning to actively develop and provoking various diseases.
During pregnancy, most latent infections, like ureaplasma, begin to worsen. This is due to physiological processes, hormonal changes in the body that occur during pregnancy.
Even if a woman is a carrier of a small amount of ureaplasma, there is a high risk that after conception she will develop ureaplasmosis.
Types of ureaplasma
Today, approximately 15 types of ureaplasma have been discovered in medicine, however, only a few of them require treatment:

In order to determine which type of bacteria is the cause of the infection, ureaplasma typing is used for each case. Only after this the doctor will be able to select and develop a treatment regimen.
 Most often, ureaplasmosis is a female disease. Statistics say that even newborns are carriers of the disease, and the disease is much more common in girls, unlike boys. That is, during childbirth, a woman passes the infection to her child.
Most often, ureaplasmosis is a female disease. Statistics say that even newborns are carriers of the disease, and the disease is much more common in girls, unlike boys. That is, during childbirth, a woman passes the infection to her child.
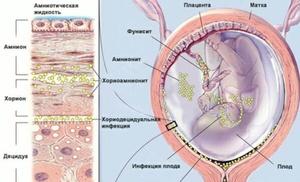
There are cases when the fetus becomes infected through the placenta (transplacental route). It is for this reason that gynecologists recommend treating inflammation before pregnancy.
The main method of infection is unprotected sexual intercourse with a carrier of the infection. Transmission of the disease through household means, for example, through visiting public places (bathhouse, toilet, beach, pool) or personal hygiene items, I did not find any confirmation in the medical data.
Danger of ureaplasma
Ureaplasmosis during pregnancy is a rather dangerous disease, as it leads to many negative consequences and complications:

In order to determine the degree of danger for the fetus or woman, it is necessary to perform special diagnostics.
Symptoms of the disease in a child
During pregnancy in women, ureaplasma manifests itself in the same way as any other pathology of the genitourinary organs. Very often a woman may not feel anything.
If you do not see a doctor, then the disease is already diagnosed in a chronic form, when it affects both the genitourinary organs and the pelvic and abdominal organs. Typically the symptoms ureaplasmosis after infection make themselves felt after a few weeks.
Possible symptoms include:

Often the first symptoms are unnoticed and may disappear even after a certain time. However, microorganisms remain, waiting until the immunity decreases even more, so that next time it can manifest itself with renewed vigor.
Diagnosis of the disease
The best option is to diagnose and treat the disease before pregnancy. After treatment of ureaplasma, pregnancy can be planned only after 3-4 months. It takes time for medications to be completely eliminated from the body.
To date there is a whole combination of different ways, which makes it possible to determine the degree and type of disease.
PCR method
 This method can detect ureaplasma in a smear from an infected area of the mucosa (cervix, urethra, vagina). Using the polymerase chain reaction, the DNA of the pathogen and the content of microorganisms in the resulting material are determined. Most often, many women have them. However, this method will not be able to find out in what quantity they are present.
This method can detect ureaplasma in a smear from an infected area of the mucosa (cervix, urethra, vagina). Using the polymerase chain reaction, the DNA of the pathogen and the content of microorganisms in the resulting material are determined. Most often, many women have them. However, this method will not be able to find out in what quantity they are present.
The norm during pregnancy for opportunistic microorganisms is considered to be: less than 10 × 3 per 1 ml. When this titer is higher, only in this case do doctors talk about the inflammatory process and make a diagnosis.
Bacteriological seeding or culture method
In order to carry out this examination, ureaplasma will be grown in the laboratory on a nutritious artificial medium.
The research will require smears from the cervical and vaginal canal. Based on the results obtained, doctors can determine how many bacteria are in the body.
This can only be done using a bacteriological method, which makes it possible not only to talk about the probable degrees of development of the disease, but also helps to identify how sensitive and resistant microorganisms are to certain antibiotics.
Serological method
 This examination is used to determine antibodies to antigens or characteristic structures of ureaplasmas. The analysis requires collecting blood from a vein.
This examination is used to determine antibodies to antigens or characteristic structures of ureaplasmas. The analysis requires collecting blood from a vein.
In addition, a woman is required to undergo examinations by a gynecologist. In order to make a general assessment of the disease, experts in some cases recommend testing for the presence of other infections accompanying ureaplasmosis.
Indications for examination are serious reasons: spontaneous abortions and frequent miscarriages, miscarriage or pathology, signs of acute inflammation, infertility, etc.
Treatment of ureaplasmosis
 This point is a subject of debate in the medical community. Since treatment of infection includes the use of antibiotics and other drugs dangerous to the developing fetus, ureaplasmosis is simply monitored in the early stages.
This point is a subject of debate in the medical community. Since treatment of infection includes the use of antibiotics and other drugs dangerous to the developing fetus, ureaplasmosis is simply monitored in the early stages.
Doctors believe that treatment of the disease is advisable only when symptomatic manifestations of inflammatory processes are present and the microorganisms detected in the titer exceed the norm.
Since doctors do not take into account isolated cases of the consequences of the disease, I do not prescribe treatment during the determination of its individual stamps in analyzes or during the absence of complaints.
If a woman experiences complications, then a step-by-step, slow complex treatment is carried out, which should pursue two objectives: to cure the disease and maintain the pregnancy.
The main condition is abstinence from sexual intercourse (even using contraception). Do not forget also that both partners must be treated, otherwise they will continue to infect each other.
In order to destroy pathogenic microorganisms, you will need to use antibiotics. However, the infection can easily adapt to them. It is absolutely necessary to complete the course of treatment, following all the doctor’s recommendations and the rules of the instructions. Most often, the antibacterial method is used only after 21–23 weeks of pregnancy in order to allow the internal organs and systems of the fetus to form normally and correctly.
Among the drugs that are usually used for ureaplasmosis, the most common are: Vilprafen, Viferon, Erythromycin.
The doctor will also prescribe various accompanying medications, for example, drugs against dysbiosis, in order to normalize the microflora of the vagina and intestines, as well as natural immunomodulators.
Treatment of ureaplasmosis should begin only in the second trimester of pregnancy. In the first trimester, treatment of the disease is not advisable, since the harm from antibacterial treatment will be greater than the presence of infection in the body.
 After long-term treatment, a woman needs to be retested for ureaplasmosis and undergo complex diagnostics to determine the condition of the fetus: Doppler ultrasound, ultrasound, and CTG in the third trimester.
After long-term treatment, a woman needs to be retested for ureaplasmosis and undergo complex diagnostics to determine the condition of the fetus: Doppler ultrasound, ultrasound, and CTG in the third trimester.
The body of any woman will require an individual approach, therefore only a doctor can guide the treatment, taking into account a specific case. If ureaplasmosis has not been cured during pregnancy, then the newborn must be examined, since the consequences of infection can be very serious. Treatment for the child is prescribed taking into account what examinations and tests show.
There is no need to diagnose yourself or make any prescriptions, especially during pregnancy. If you do become infected with ureaplasma, then there is no need to panic: by promptly seeking qualified medical help, you can be cured of the infection forever and give birth to a strong and healthy child.
And they underwent examinations.
This is necessary to identify various diseases and infections that can harm the unborn baby and lead to serious complications.
Basically, these are infectious diseases of the genital tract, which include ureaplasmosis.
By learning about the disease before conception, you can get the necessary treatment and get rid of the infection. However, this does not always happen.
According to medical statistics, most people suffer from a latent and asymptomatic form of ureaplasmosis, without even knowing it. After all, very often a woman’s problem is detected already during pregnancy.
It is impossible to ignore the infection, as it threatens with serious complications and a negative impact on the child, but antibiotics that will have to be used to treat the disease can also negatively affect the formation of the fetus. Therefore, expectant mothers are at a loss in search of the right solution.
The disease takes its name from the pathogenic protozoan microorganism Ureaplasma urealyticum, parvum (ureaplasma urealyticum and parvum). This bacterium is the main causative agent of infection.
Affected by infection, the cervical os of the uterus may open prematurely, expelling the fetus.
- Risk of ectopic pregnancy.
- High risk of developing postpartum endometritis.
After childbirth, ureaplasmosis increases the risk of developing inflammatory processes in the uterine mucosa, that is, endometritis. Also among postpartum complications, inflammation of the appendages is noted.
If the baby was infected while passing through the birth canal, so that the infectious agents got on the mucous membranes of the genital organs or the lining of the respiratory tract, then the consequences can be very serious.
There are rare cases where ureaplasma caused the development of diseases of the brain and lungs, even death.
To determine the degree of danger to a woman or fetus, it is necessary to carry out special diagnostics.
What may be the symptoms of the disease?
During pregnancy, ureaplasma in women manifests itself in the same way as any other classic disease of the genitourinary organs. Often, a woman may not feel or notice anything special at all.
If you do not see a doctor, then the disease is detected in a chronic form, when it affects not only the genitourinary organs, but also the abdominal and pelvic organs. Typically, signs of ureaplasmosis can become apparent several weeks (3-5) after infection.
Possible symptoms include:
- small clear vaginal discharge;
- discomfort when urinating;
- with inflammatory processes in the appendages or in the uterus, a woman may feel pain and cramps;
- in case of oral infection, pharyngitis or sore throat occurs;
- men may experience symptoms of prostatitis;
- The most pronounced symptom is vulvovaginitis in various forms and other inflammatory processes.
Often the first symptoms go unnoticed, and they may even disappear after some time. But the microorganisms remain, waiting for an even greater decrease in your immunity in order to manifest themselves with renewed vigor the next time.
Diagnosis of a dangerous infection
The ideal option is to identify and treat the disease before pregnancy.
You can plan a pregnancy after treatment for ureaplasma only after 2-3 months. It takes time for the drugs to be completely eliminated from the body.
 If a woman is already expecting a child, but the examination has not been previously carried out, then the diagnosis is made only in cases where there is a suspicion of the presence of infection.
If a woman is already expecting a child, but the examination has not been previously carried out, then the diagnosis is made only in cases where there is a suspicion of the presence of infection.
Now there is a whole combination of different methods to determine the presence, type and extent of the disease. Only a doctor can recommend which examination you should undergo.
PCR method
This test can detect ureaplasma in a smear from the affected area of the mucosa (vagina, urethra, cervix). Thanks to the polymerase chain reaction, it is possible to identify the DNA of the pathogen and understand whether the resulting material contains microorganisms.
As a rule, most women have them. True, it will not be possible to determine in what quantity you have them.
The norm for opportunistic microorganisms during pregnancy is considered to be: less than 10*3 per ml. If this titer becomes higher, only then do doctors talk about inflammation and diagnose “ureaplasmosis”.
Cultural method or bacteriological culture
To conduct this research, ureaplasma will be grown in an artificial nutrient medium in the laboratory.
For the analysis, you will need your smears from the vagina (or urethral mucosa), from the cervical canal, as well as collection of morning urine.
Thanks to the results obtained, specialists will be able to determine how much ureaplasma is present in your body.
This can only be done using the bacteriological method, which allows us not only to talk about the possible degrees of development of the disease, but also to reveal how resistant and sensitive microorganisms are to specific antibiotics. This is how the effectiveness of the treatment is checked.
At the same time, the doctor will ask you to undergo general tests.
Detection of antibodies in blood or serological method
This test is used to detect specific antibodies to characteristic structures or antigens of ureaplasmas.
This will require donating blood from a vein.
In addition, the woman should undergo examinations by a gynecologist. To make a general assessment of the disease, experts sometimes recommend testing for the presence of other infections that may accompany ureaplasmosis.
Indications for tests are serious reasons: pathologies or miscarriage, frequent miscarriages and spontaneous abortions, infertility, signs of acute inflammation, etc.
How to treat ureaplasmosis during pregnancy?
 This point remains a subject of controversy in the medical community.
This point remains a subject of controversy in the medical community.
Since treatment of infection includes taking antibiotics and other medications that are unsafe for the developing baby, ureaplasmosis is simply monitored in the early stages of pregnancy.
Experts believe that treatment of infection is advisable only when clinical manifestations of inflammatory processes are present, and when microorganisms are found in a titer that exceeds the norm.
Since doctors do not focus on isolated cases of the consequences of an infection, if single signs of infection are detected in tests or in the absence of complaints, treatment is not prescribed.
If a pregnant woman has complications, then they begin a slow, step-by-step complex therapy, which must pursue two goals: to maintain the pregnancy and cure the disease.
The most important condition is abstinence from sexual contact (even with contraception). Also remember that both partners must be treated, otherwise they will continue to infect each other.
To destroy harmful microorganisms, you will have to take antibiotics.
True, the infection may well adapt to them. As already described above, the effectiveness of treatment can be confirmed by bacterial culture.
You will definitely need to complete the full course of treatment, following all the rules of the instructions and doctor’s recommendations. As a rule, the antibacterial method is used only after 20-22 weeks of pregnancy to allow all the main systems and internal organs of the baby to form correctly and normally.
Among the medications that are usually prescribed for ureaplasmosis, the most common are: Erythromycin, Viferon, Vilprafen and others.
Treatment of ureaplasmosis should begin only in the second trimester of pregnancy.
In the 1st trimester, treatment of ureaplasma is not advisable, since the harm from antibacterial therapy will be greater than the presence of infection in the body.
After long-term treatment, a woman needs to undergo repeated tests for ureaplasmosis, as well as conduct a comprehensive diagnosis of the condition of the fetus: in the 3rd trimester.
Each woman’s body requires an individual approach, so only a doctor can guide treatment based on a specific case. If ureaplasmosis has not been cured during pregnancy, then the newborn must be examined, since the consequences of infection can be very severe. Treatment for the baby is prescribed depending on what tests and examinations show.
Disease prevention
It will help you get rid of many unpleasant moments. This way, you can safely undergo examination and treatment without much fear if an infection is detected.
The expectant mother should be attentive to her health: avoid promiscuity, use protection during sexual intercourse, maintain her immunity at the proper level, and regularly visit a doctor for preventive examinations.
Do not diagnose yourself and do not make any prescriptions yourself, especially during pregnancy. If infection with ureaplasma does occur, do not panic: by seeking qualified medical help in time, you can recover from the infection and give birth to a healthy and strong baby.
For genital tract infections. However, this is not always possible, so some diseases may appear directly during pregnancy.
The vaginal microflora has more than 30 types of microorganisms. The vast majority of them are lactobacilli. Other pathogenic microorganisms make up only 5-10%. If the body functions normally, then even pathogenic microflora may not cause any diseases. But when immunity decreases or under any stress, these opportunistic microbes lead to illness.
Analysis for ureaplasma during pregnancy
Ureaplasma also belongs to opportunistic microorganisms. This means that small amounts of ureaplasma can be present in the body without causing damage.
But during pregnancy, ureaplasma can worsen. This is a threat to the fetus and pregnancy. Over the past years, more and more women have heard a disappointing diagnosis - ureaplasmosis. However, you should know how much this disease can interfere with the birth of a healthy baby.
Symptoms of ureaplasmosis appear 4 weeks after entering the body. However, if in men it is similar to urethritis: the same pain when urinating, the appearance of mucous discharge, then in women only small ones can be observed. These symptoms pass very quickly and, it would seem, there should be no problems. But, you need to remember: the virus settles in the vagina and is simply waiting for its time, when the body weakens a little. During pregnancy, immunity decreases and as a result the virus progresses.
To diagnose ureaplasmosis, modern medicine provides a whole combination of methods, the choice of which lies with the doctor. Thus, analysis for ureplasma during pregnancy can be carried out using the bacteriological method, as well as the polymerase chain reaction (PCR) method.
The bacteriological method involves taking a smear from the pregnant woman from the mucous membrane of the urethra, vaginal vaults and from the ecclesiastical canal. A study of morning urine is also provided - all this together will make it possible to determine the amount of ureaplasma, as well as the resistance and sensitivity of the pathogen to certain medications before their prescription.
PCR (polymerase chain reaction) is a reliable confirmation of the presence of ureaplasma, because it detects DNA particles of the pathogen. The PCR test for ureaplasma during pregnancy also involves taking samples from the vagina, cervix and urethra. And, although it is possible to determine the presence of ureaplasma in a smear using PCR within five hours, however, this analysis is not capable of determining in what quantities they are present.
How does ureaplasma affect pregnancy?
It should be remembered that ureaplasmosis can cause termination of pregnancy, moreover, in its early stages. Especially if the disease first occurred during pregnancy: the formation of defects in fetal development leads to miscarriage in.
If the disease first appeared in the second or third trimester of pregnancy, then ureaplasma can lead to fetoplacental insufficiency - a condition when the baby lacks oxygen and nutrients. In turn, this can also cause the threat of termination of pregnancy. The danger of ureaplasma for pregnancy also lies in the fact that the disease must be treated with antibiotics. As doctors always warn, taking medications while carrying a child is extremely undesirable - antibiotics are highly likely to negatively affect the fetus and cause a miscarriage.
Ureaplasma during pregnancy: consequences
The consequences of ureaplasmosis during pregnancy can be very unpredictable and even very, very serious. There are, for example, cases where ureaplasma causes inflammation of the uterus and which are quite severe postpartum complications.
The consequences of ureaplasma are also dangerous for the baby. Firstly, there is a risk of developing intrauterine infection of the fetus. However, even if infection was avoided during pregnancy (the fetus is relatively protected from ureaplasma by the placenta), then at the moment of passage through the birth canal, the child becomes infected in almost half of the cases. And this, in turn, entails damage to various organs and systems of the newborn, most often inflammation of the respiratory tract.
Miscarriages in the presence of ureaplasmosis during pregnancy occur due to the “looseness” of the cervix and softening of the external pharynx under the influence of ureaplasma. But, at the same time, there is another serious risk for the mother associated with ureaplasma: ureaplasmosis can lead to infection of the uterus and the development of endometritis in the postpartum period - a complex and severe purulent complication.
Should ureaplasma be treated during pregnancy?
But you should not terminate the pregnancy if ureaplasmosis is detected. Correct and timely treatment will help a woman bear a child.
Ureaplasma should be treated in any case, even during pregnancy. Start doing this depending on the duration and characteristics of the pregnancy. If complications arise or the threat of miscarriage occurs, treatment should begin immediately. However, when everything is normal, doctors recommend treating ureaplasmosis after the 30th week. This will ensure that at the time of birth the baby will not become infected with ureaplasma during passage through the birth canal. Otherwise, ureaplasma may be detected in the nasopharynx in newborns, and also on the genitals in girls. Some gynecologists insist that it is better to treat the disease from 20-22 weeks of pregnancy, then all the baby’s organs will already be formed. Each organism is unique, so the doctor selects drugs individually, guided by the course of a particular pregnancy.
It is imperative that both sexual partners undergo treatment and limit sexual contact during treatment.
At the end I would like to add just one thing. Ureaplasma during pregnancy is not a death sentence for your child’s life. Contact an experienced doctor, and you will still be able to cure ureaplasma without harm to the body.
Especially for- Maryana Surma
From Guest
I had a miscarriage for 8 weeks and started looking for the cause of ureoplasma 10*4, probably it still needs to be treated and on time, it’s a shame
From Guest
I had ureaplasma before pregnancy, during pregnancy I took a test, it showed 10 to 6 degrees, they said I needed to treat it, I took antibiotics from 24 weeks and inserted suppositories rectally, the baby was born healthy, everything is fine, it didn’t affect him in any way, even though I I was very worried, I went to consult 3 doctors, they told me to treat and that by 24 weeks the main development of the child’s organs ends and treatment can begin, then I took the test again, it showed 10 to 4 degrees, and the 4th is considered no longer high
From Guest
I had ureaplasma before pregnancy, and I even treated it, but it still remained. Then she became pregnant unplanned and was very worried about this; she was treated with approved antibiotics after 22 weeks - the analysis remained the same, with the same amount. But after giving birth, it doesn’t show up in me... That’s it.
During pregnancy, the health of the expectant mother is under close control. Regular laboratory tests and instrumental procedures are carried out. If conception is planned in advance, the woman first undergoes a full medical examination, which allows us to exclude pathologies or inflammatory processes.
In most cases, diseases and inflammations are diagnosed already during pregnancy. Various infections of the genitourinary system are especially dangerous. What is ureaplasmosis, what danger does it pose to the health of the expectant mother and baby? How is pathology diagnosed and treated?
Characteristics of the disease
Ureaplasmosis is an infectious disease characterized by inflammation of the genitourinary system. The causative agent of the pathology is ureaplasma. This is a simple bacterium that was discovered in the 70s.
Initially, the infection was classified as an STD (sexually transmitted diseases), but over time and the development of medicine, the opinion of doctors has changed. Ureaplasmosis has become a simple sexually transmitted infection.

The bacterium does not have cell walls. It is a conditionally pathogenic microorganism. This means that ureaplasma can live in the body for a long time without causing any problems or showing symptoms. That is why very often the pathogen is diagnosed only during routine examinations. Clear signs of the inflammatory process appear in the presence of a kind of catalyst.
This means that several decisive factors must be present that trigger the pathogenic activity of the bacterium. Inflammation develops against the background of reduced immune defense of the body. Usually, another genitourinary infection occurs in parallel with ureaplasmosis.
Routes of infection
The disease applies to women, but also occurs in men. An adult woman can become infected in one way - through sexual intercourse (both vaginal and oral). Ureaplasma during pregnancy is a serious pathology, as it is likely to be transmitted to the baby and affect his health.
The infection is common in newborn babies, especially girls. The ratio of infected girls to boys is 5:1. There is a high chance that a woman will pass the disease to her child during childbirth.
Less commonly, ureaplasma during pregnancy is transmitted in other ways, for example through the placenta. Sometimes microorganisms penetrate the amniotic sac into the amniotic fluid and then into the fetal lungs. Infection through household contact (through touch, personal hygiene items, shared bedding) has not been scientifically proven.
Types of microorganisms
More than 10 types of microorganisms are identified. Only 2 of them lead to pathological processes and require treatment.
Types of pathogenic bacteria:
- Ureaplasma parvum. Ureaplasma parvum during pregnancy is a less dangerous type. Bacteria concentrate on the genital mucosa and lead to inflammation. Sometimes pathology causes the formation of stones and a decrease in immune defense.
- Ureaplasma urealiticum. Aggressive type of bacteria. Penetrates not only into the mucous membranes, but also into the blood. Reduces immunity and can lead to infertility in women.
Other types of infection are not dangerous. They can be present in the body without causing problems. For example, Ureaplasma spices is part of the normal and healthy microflora of a woman.

Symptoms of ureaplasmosis
Symptoms can be vague and indistinct, which confuses many pregnant women. Also, the signs depend on the location of the inflammation and how far the infection has progressed. After the incubation period, the woman develops early stage symptoms. They are characteristic of the disease, but are not always informative.
First, 2 main symptoms appear - inflammation of the mucous membrane and whitish discharge. However, both of these signs are often attributed to pregnancy or thrush. Many women do not consider it necessary to see a doctor, consider it a trifle and self-medicate.
After the symptoms subside, the infection “falls asleep” until favorable conditions arise. With stress, decreased immunity, and chronic fatigue, microorganisms wake up and lead to serious problems.
Symptoms of pathology depending on the location of inflammation:
- Damage to vaginal tissue. The patient experiences colpitis, that is, inflammation, as well as white, dense discharge.
- Uterus. When the infection has reached the uterus, the pregnant woman suffers from pain in the lower abdomen. This indicates endometritis.
- Bladder. Characterized by the manifestation of cystitis. A woman feels a frequent urge to urinate. The process itself is not very effective and causes pain.
- Oral cavity. If the infection was caused by oral contact, the standard signs of a sore throat will be observed.

How does infection affect pregnancy?
How does the disease threaten the fetus? How does it affect the pregnancy process and a woman’s health? This question worries all women.
Previously, it was believed that urogenital infections were incompatible with pregnancy, and that a woman should have an abortion. At the moment everything has changed. Doctors are confident that pregnancy with pathology is quite possible. With proper and timely treatment of ureaplasma, the child is born completely healthy. However, dangerous consequences cannot be ruled out.
Consequences for a woman
Possible consequences for women:
- Reproductive dysfunction. Pathological processes in the vagina and cervix do not allow the embryo to attach to the uterine wall. Without treatment, infertility is possible.
- Inability to bear a child. This includes both premature birth and fetal death.
- Increased risk of ectopic pregnancy. This possibility occurs when the fallopian tubes are infected.
- Postpartum endometritis (inflammation of uterine tissue). After childbirth, the risk of inflammation of the uterine lining and appendages increases.

Consequences for the child
What are the possible consequences for the baby? The potential threat depends on when the baby became infected - during intrauterine development or during childbirth.
Complications during intrauterine development:
- Fetal blood infection. This rarely happens, since the mother’s body reliably protects the baby. This happens if the mother becomes infected at an early stage, when the embryo does not yet have its own blood flow. Serious pathologies are possible with a small probability.
- Miscarriage or premature birth. Ureaplasmosis softens the walls of the uterus, which complicates the process of pregnancy. In the early stages there is a risk of miscarriage, and in the later stages there is a high risk of premature birth.
- Lack of oxygen and essential nutrients. This happens when infection occurs in the 2nd or 3rd trimester.
- Consequences of treatment. During therapy, antibiotics are necessarily used, which are undesirable for the fetus.
If a child becomes infected during childbirth, the consequences may be as follows:
- pneumonia;
- conjunctivitis;
- pyelonephritis or nephritis;
- bronchopulmonary dysplasia;
- meningitis.
Is it possible to conceive a child with ureaplasmosis?
All experts say unequivocally that it is quite possible to conceive a child. There are no physiological barriers to ureaplasmosis. However, it was previously mentioned about the possible danger of developing pathologies, both for the fetus and for the expectant mother.
Pathological processes in the vagina, cervix and os of the uterus or appendages can interfere with conception. There is a possibility that the embryo will not implant. However, Ureaplasma parvum will not interfere with a normal and healthy pregnancy. It is best to have a medical examination before conceiving.
Diagnosis of the disease
The ideal option is to undergo a diagnostic test before planning a pregnancy. If the disease is detected, attempts to conceive can be resumed only after 2-3 months. In this case, all the drugs will definitely leave the body.
If a woman is already pregnant, diagnostics are prescribed when there is a suspicion of a problem. Diagnostic measures are completely safe.
Examination methods:
- PCR (polymerase chain reaction). Doctors take a swab from the affected area. The method allows you to determine the presence of pathogenic DNA. It does not show the number of microorganisms.
- Bacteriological culture. Allows you to determine the level of resistance of bacteria, as well as their exact quantity. The norm for the content of conditionally pathogenic microflora is less than 10,000 per 1 ml.
- Serological study, antibody test. To do this, blood is taken from a vein. The presence of certain antibodies or antigens is determined. Used when severe symptoms are present.
Treatment methods
How to treat ureaplasma at different stages of pregnancy so as not to harm either the mother or the baby? You need to know that therapy is for both partners. Otherwise, after recovery, the woman will become infected again from the man.
During therapy, you must abstain from sexual activity or be sure to use a condom. Otherwise, it will be a vicious circle - partners will take turns infecting each other.
The only way to treat ureaplasmosis is to take antibiotics, because the infection is bacterial in nature. It is impossible to do without antibacterial drugs. The whole difficulty is that antibiotics are extremely undesirable during pregnancy.

To reduce the risk of side effects, therapy begins no earlier than 20 weeks. During this period, the fetus has already formed vital organ systems, so the negative impact of the drugs is reduced.
Many women do not understand why doctors prescribe a long list of medications that are not directly related to the infection. Among them are immunomodulators, immunostimulants, probiotics and other means for normalizing microflora.
Antibiotics act indiscriminately; they destroy all bacteria, including beneficial ones, and reduce the body's immune defense. He becomes susceptible to infections and diseases. The condition of the expectant mother is deteriorating. This is why medications are prescribed that will support the immune system. Probiotics will help avoid dysbiosis and normalize the balance of microflora.
Prevention measures
To avoid the development of ureaplasmosis and other urogenital diseases, you need to follow preventive measures and be attentive to your health. First of all, plan your pregnancy in advance and undergo medical examination and treatment.
Casual sexual contact should be avoided. If you are unsure about your partner, use condoms. Twice a year you need to visit a gynecologist for examination and tests. This will help to diagnose any inflammation in a timely manner. Women's health is extremely important.
It is prohibited to independently diagnose and treat pathology. Self-medication has a negative impact on health. Firstly, it will not help, and secondly, it can harm mother and child.
Greetings to all regular and new readers of our site! We have already devoted more than one topic to pregnancy and preparation for it. But many questions still remain. Recently, one of my readers contacted me: during a gynecological examination, she was diagnosed with ureaplasma at 6 months of pregnancy. The girl was very frightened by the fact that now all she could do was pray: ureaplasma during pregnancy can have the most serious consequences for the child. Is it so? We'll find out at the end of today's conversation.
Share, dear girls and women, how many times a year do you visit our chief doctor, a gynecologist? Some people are regularly checked for infections and various pathologies twice a year, while others have never been examined for 5 years. And how negligently many people treat pregnancy! I won’t tire of repeating: it’s better to play it safe three times and calmly enjoy bearing a baby than to underexamine, not notice the “sore” and then be afraid that it will harm the baby.
I have already talked about what tests you need to take when planning a pregnancy in previous topics. In a good way, STIs should be identified at the stage of preparation for conception in order to have time to be treated. Normally, in addition to beneficial lactobacilli, our body contains about 5-10% pathogenic microorganisms. For the time being, they “sit” quietly, without making themselves known.
Pregnancy reduces immunity, as all efforts are devoted to preservation and gestation. And here the “sores” begin to manifest themselves in all their glory. Ureaplasmosis is detected in approximately 70% of women! Its first symptoms appear after 4 weeks in the form of slight mucus discharge. Sometimes we don’t even notice them, they pass, but during pregnancy the virus begins to act with a vengeance.
Ureaplasma during pregnancy: consequences for the child
How is ureplasma transmitted? First of all, sexually. Infection through personal hygiene items (towels, patient underwear) is also possible. But there are two more ways: intrauterine (when the baby becomes infected through infected amniotic fluid), and during the passage of the fetus through the birth canal.
For the mother, the disease can threaten inflammation of the appendages and uterus, purulent endometritis after childbirth. The baby may be even worse off. Ureaplasmosis often causes miscarriage due to loosening of the cervix. This is the most dangerous consequence. If the infection affects the placenta, then fetoplacental insufficiency will almost certainly develop, and the development and growth of the baby will proceed more slowly.
During childbirth, babies become infected more often than in the mother's belly. The bacterium begins to attack the sterile body and as a result, infants develop, the respiratory system is affected, and the central nervous system suffers. Such children subsequently begin to have headaches, they become nervous and easily excitable, and the syndrome develops. In girls, the genitals become infected with their mother's viruses.
Ureaplasma: treat or cripple
All the consequences of ureaplasmosis during pregnancy have not yet been sufficiently studied, but there is enough already known information to confidently say: it is necessary to treat ureaplasma! But what to treat, you ask, is it really antibiotics, like most sexually transmitted infections? Yes, including them. Previously, this virus was considered almost a 100% indication for abortion, of course, in the early stages. It was believed that if the fetus survived the infection, it would be born with serious pathologies.
Indeed, infection in the first trimester can lead to consequences, but modern medicine is against termination of pregnancy and in favor of treating ureaplasmosis. Moreover, new generation drugs make it possible to do this with virtually no harm to the child.
If there is no threat of miscarriage or other serious complications, then doctors recommend starting treatment after the 30th week of pregnancy so as not to harm the fetus. Some doctors say that you can start therapy at 20 weeks, when all the baby’s organs are already formed. In any case, you will take all actions only after a thorough examination, following the recommendations of your gynecologist. Typically, PCR (polymerase chain reaction) and BAC culture are used to diagnose ureaplasmosis in medicine.
Prepare for the fact that both you and your spouse will have to undergo treatment to avoid re-infection.
Treatment will be comprehensive and include:
- Antibiotics (usually the safest ones are prescribed, from the macrolide class, for example, Erythromycin)
- Immunomodulators to support normal immunity
- Restorative agents for vaginal microflora.
Before treatment, bowel cleansing with enterosorbents may be required. The course lasts about 4 weeks. Throughout this period, doctors recommend carefully monitoring your diet, eating more fruits and vegetables, as well as dairy and sour-milk products. After a couple of months, the gynecologist will take a smear again. If it turns out to be clean: hooray! Ureaplasma was expelled from the body.
Hygiene and prevention
If you are one of the lucky 30 percent of women who are not familiar with ureaplasma, then you probably follow personal hygiene and prevention measures. I tell the rest. Again, common truths, but it’s better to repeat them again and remember them than to be at risk during pregnancy.
- Always maintain personal hygiene and wear underwear only made from natural materials.
- Use only your own hygiene products, including toothbrushes, washcloths, and towels.
- Don't change sexual partners too often. I’ll keep silent about casual relationships; I hope you and I are not so frivolous.
- Protect yourself with condoms.
- Check with a gynecologist once every six months.
- Plan your pregnancy in advance and go through it with your partner or spouse
Be careful and consult a doctor at the slightest symptoms. I suggest you conclude today's topic. To do this, please visit the forum and leave feedback on the topic of various genital “sores” during pregnancy. Tell us how you managed to detect and treat them, and what consequences awaited you afterwards.
If you have any questions after reading, I will be happy to answer! Until new publications, stay safe everyone!