What does a liver CT scan with contrast show: how effective is it in diagnosis? Computed tomography (CT) of the liver - normal, with contrast, which shows side effects and contraindications, preparation and implementation, norms, interpretation of results, etc.
What is a CT scan of the liver?
Computed tomography of the liver (CT) is a non-invasive method of radiological diagnostics. With the help of this study, layer-by-layer and fairly accurate three-dimensional images are obtained not only of individual organs, such as the liver, but also of any other part of the human body. This modern method is widely applicable for diagnostics in all areas of medicine, since obtaining high-quality images is usually combined with the absence of discomfort for the patient.
Indications for CT scan of the liver
A liver CT scan may be prescribed to prepare patients for surgical interventions or if it is impossible to determine the diagnosis by other diagnostic methods. Indications for computed tomography of the abdominal cavity itself to visualize the liver may be as follows:
- Planned surgical operations in the abdominal cavity and liver. Especially if you have cancer.
- Acute conditions, the symptoms of which are not diagnosed by other methods.
- In case of unexplained deterioration in health, for example, sudden weight loss, in such cases, liver metastases are likely to be detected.
- In case of injury to the abdominal organs with sharp objects.
- Assessment of the dynamics of the treatment.
This diagnostic method is also actively used in traumatology, as it provides the most accurate image of bones. You should know that even such an advanced method as MRI of the liver, with a similar imaging principle, does not have this property.
This method is highly safe, but liver CT also has some contraindications, for example:
- Contrast contrast should not be used in pregnant women - it can have a detrimental effect on the fetus;
- in people with an illness such as iodine intolerance;
- with existing severe damage to the kidneys and liver.
How to prepare for a liver CT scan?
Preparation is no less important than the procedure itself. Failure to comply with the doctor’s prescriptions can lead to misleading him and cast doubt on the confirmation of the diagnosis.
To prepare for diagnostics (CT of the liver), as for most abdominal organs, there are special recommendations related to its functions and location:
- It is recommended not to eat food that causes excessive gas production in the intestines, as it can compress and obscure the desired organ.
- It is advisable to consume food at least 7 hours before the procedure.
- In rare cases, when a child is prescribed a CT scan, sedatives or anesthesia are used. To conduct the study correctly, the child must not be allowed to move.
- For targeted diagnostics, for example, of the gallbladder and ducts, a CT scan of the liver is performed with contrast, which shows a more accurate picture in a separate area due to an increase in the difference in tissue density in it. In such cases, before starting, the patient is given special drugs that pass through the liver tissue and will retain radiation.
Diet before CT scan of the liver
The diet is not particularly difficult for the patient; it is only suggested to remove the following products from the diet (preferably for 2 days):
- All carbonated drinks.
- Beans, cabbage.
- Lactic acid products and milk.
- Brown bread and baked goods.
How is a liver CT scan performed?
The procedure for performing a CT scan of the liver without contrast or with it consists of several stages:
- The prepared patient lies down on a special tomograph table, which is located in a glass-separated room. Visual contact is maintained, and you can also communicate with the doctor via speakerphone and receive specific instructions from him.
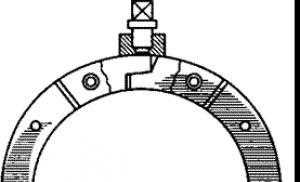
- The table with the patient moves through the ring, the desired angle is selected.
- The diagnostician takes pictures. The patient may be asked to hold their breath for a short time.
- Within 20-30 minutes, images (tomograms) are prepared and a diagnosis is made.
Diagnostic doctors make a diagnosis that indicates the presence of any defects, for example, the presence of a cyst in the liver, so asking about the exact conclusion of your condition or prognosis in most cases does not make sense.
After the procedure, all restrictions that may have existed previously are lifted, and drinking plenty of fluids is also recommended to remove the contrast agent.  Photo: CT scan of the liver is normal
Photo: CT scan of the liver is normal
CT liver indicators and their interpretation
The images obtained during the procedure are issued in the form of films or on a CD.
The pictures are deciphered by the doctor who took them, and then by the one who sent them. It is quite easy to evaluate the result; all pathologies appear in the image as darkening or defects in the filling of the contrast agent. For example, thrombosis of blood vessels - darkening in their lumens. But without medical education, some pathological conditions are simply impossible to determine.
Normal picture
- The hepatic and bile ducts appear as low-density areas, but if contrast is used, the bile ducts become noticeably distinguishable from the surrounding vessels and parenchyma.
- Liver tissue has a higher density than tissues of other organs.
- The portal vein is visible, the vessels are less dense and have a round or linear shape.
- The parenchyma is homogeneous.
- The gallbladder may not be visible or may have a round shape with low density.
Signs of pathology
- The contours of the organ have been changed. Primary tumors are visible in the form of round formations.
- Areas with reduced density, which indicate hemangioma - a benign tumor.
- Homogeneous hypoechoic foci are visualized with clear boundaries. This occurs with an abscess.
- The liver is enlarged in size, its edges are uneven.
- Dilation of the bile ducts.
Factors that may affect liver CT results
- Movements during the procedure.
- Use of bismuth and barium in previous studies.
- Presence of metal on the patient.
- Pregnancy (although this is usually a contraindication to CT scanning).

Liver diseases occur at any age. They can be congenital or acquired during life. It is very important to diagnose them at an early stage. Computed tomography of the liver is a very reliable and reliable method for diagnosing diseases of the organ.
Indications for CT scan of the liver are:
- Preoperative study.
- Suspicion of tumor formations, as well as their diagnosis.
- Identifying the consequences of injury.
- Diagnosis of complications after surgery: hematomas, abscesses and others.
- Suspicion of vascular damage to the organ.
- If it is not possible to perform an ultrasound if there is excess fat in the area to be examined.
Contraindications for the study
Due to some limitations to the study, computed tomography of the abdominal organs cannot be recommended for some patients. Thus, it is absolutely prohibited for pregnant women, for whom it poses a threat due to the possible teratogenic effect of X-rays on the fetus.
Also, this diagnostic method is not used in people suffering from obvious obesity. If the subject's body weight is more than 200 kg, the procedure cannot be performed even on the most modern and powerful CT machines. This contraindication is not exclusive to CT scanning; other studies also include restrictions on weight or fat pad thickness. For example, ultrasound is most often impossible for patients weighing about 150 kg, and “average” models of radiography machines are not intended for diagnostics in people weighing over 100-120 kg.
Preparing for diagnosis
Special preparation for liver CT is not required unless the procedure is supplemented with contrast. Preparing for a liver CT scan with contrast is not difficult. It consists in the fact that you should not eat food before the examination.
How is the procedure carried out?
The tomograph is a ring to which a movable diagnostic table is attached. The patient is placed on the table lying on his back. They warn you to remain still. Slide the table inside the device. During the scan, the upper abdominal cavity is irradiated. The absorption of rays by tissues is recorded by sensors. The image is obtained as the computer processes all received pulses.
In most cases, a CT scan of the liver with contrast is performed. The patient is given a contrast agent intravenously. It allows you to clearly visualize the boundaries of all organs in the studied area and separate them from each other. In the presence of neoplasms and anomalies, contrast helps to accurately determine their size and density. Before this test, the doctor should ask the patient about an allergy to iodine.
Normal picture
Normally, liver tissue is homogeneous and has a slightly higher density than tissue of the pancreas, kidneys and spleen. Areas of lower density, linear or rounded, against the background of homogeneous parenchyma correspond to liver vessels. The portal vein is usually visualized, but the hepatic artery is not. Intravenous administration of a contrast agent reduces the difference in density between the vessels and the parenchyma.
Intrahepatic bile ducts are usually not visible on tomograms, but the common hepatic and common bile ducts are often visualized as low-density structures. Due to the fact that bile is close in density to water, intravenous administration of a contrast agent leads to a clearer distinction of the bile ducts from the surrounding parenchyma and liver vessels.
The gallbladder is visualized as a round or elliptical formation, which, like the bile ducts, has low density. The contracted gallbladder may not be visualized (therefore, studies must be performed on an empty stomach).
Deviation from the norm
Pathological formations of the liver in most cases have a lower density than its unchanged parenchyma. CT can distinguish fairly small lesions. Using intravenous contrast scanning, it is possible to better distinguish pathological lesions from normal parenchyma due to increased parenchymal density.
Primary liver tumors or metastases have the appearance of rounded formations with a density slightly less than the density of unchanged parenchyma, and with clear or blurred boundaries. However, sometimes the tumor cannot be detected, since it does not differ in density from the surrounding parenchyma. Sometimes a large tumor deforms the contours of the liver. Liver abscesses have the appearance of homogeneous hypoechoic foci, usually with clear boundaries. Liver cysts are round or oval in shape, have sharply defined boundaries, and are less dense than abscesses and tumors.
The density of liver cancer depends on its stage. A fresh thrombus is denser than normal parenchyma; the density of an organizing thrombus is less than the density of liver parenchyma. Intrahepatic hematomas have different shapes; subcapsular hematomas are shaped like a sickle and push the liver parenchyma away from the capsule.
In the differential diagnosis of obstructive jaundice and other types of jaundice, attention is paid to the condition of the bile ducts; expansion of the latter is a sign of obstructive jaundice, while their normal diameter indicates non-obstructive jaundice. Dilated intrahepatic bile ducts look like branching linear and round structures of low density against the background of homogeneous liver parenchyma. Depending on the level of obstruction, dilation of the common hepatic duct, common bile duct and gallbladder may also be observed. Mild dilatation of the bile ducts is easier to detect by contrast.
CT scans can usually identify the cause of biliary obstruction, such as gallstones or cancer of the head of the pancreas. However, if it is necessary to know the location of the obstruction before surgery, percutaneous transhepatic cholangiography or endoscopic retrograde cholangiopancreatography (less frequently) is also used.
MRI or computed tomography
Magnetic resonance imaging and computed tomography are based on different technological processes and are intended for different studies. Computed tomography is based on the use of X-ray radiation, so it has the same drawback - during the study the patient is exposed to radiation, although modern devices can reduce the radiation dose to a minimum. The principle is simple, like everything ingenious. X-rays pass through the area of the body that is being examined from different directions, and then, by processing the information received, an image is built - a slice of the body. The monitor screen clearly shows whether all organs are in order, whether their sizes have changed, whether they have moved relative to one another, or whether a tumor has appeared. Unlike a blurry X-ray or a very specific ultrasound image, a CT scanner provides a clear picture. A computer tomograph can also convey the exact dimensions of everything that is inside our body - with an accuracy of up to a millimeter.
And magnetic resonance imaging technology uses magnetic waves rather than x-rays. The patient is placed in a magnetic field generated by an MRI scanner. In a split second, the device emits a radiofrequency pulse, and the molecules of human tissue come into resonance. Therefore, tomography is called not just magnetic, but magnetic resonance imaging. The nuclei of atoms send vibrations in response, they are recorded by a computer, which also projects on the screen an image of a section of tissues and organs in various planes. If necessary, three-dimensional images can be obtained for a more accurate assessment of detected changes. By the way, magnetic resonance imaging was originally called nuclear magnetic imaging - because of the vibrations coming from the nuclei of the atoms of human tissues. However, the word “nuclear” scared many, so it was decided to rename the method, and now it is called magnetic resonance imaging. There is no nuclear reaction, much less radiation, in an MRI scanner. This is generally one of the safest types of diagnostics; if necessary, it can be prescribed to pregnant women and young children.
Examples of liver pathology:
Liver metastases - multiple low-density foci of different sizes, indicating metastatic lesions, are visible in the liver tissue

Hemangioma of the liver. CT

Hepatocellular carcinoma of the liver. KG after contrast.

CT. Fatty liver hepatosis. A pronounced decrease in the density of the liver parenchyma is determined. Against its background, non-contrasted liver veins (arrows) are clearly visible - a symptom of inversion of the vascular pattern.

CT with contrast. Multiple congenital simple liver cysts.

CT scan of the liver with contrast. Liver abscess. A cavity is visible in the liver parenchyma, accumulating a contrast agent and surrounded by a thick, contrasting capsule.

CT scan for focal nodular hyperplasia of the liver: a - on the tomogram before contrast, a local change in the structure of the liver parenchyma is barely noticeable (arrow); b - in the arterial phase of contrast, a hypervascular formation with a scar in the center is clearly visible (arrow).

Hepatocellular carcinoma (arrow):
a - in the liver parenchyma before contrast, an area with reduced density is visible; b - in the arterial phase, its inhomogeneous contrast is noted. The contours of the tumor are lumpy and indistinct
Modern diagnostic methods make it possible to identify pathological processes and changes in the human body at early stages, and therefore increase the effectiveness of treatment. High-precision research methods include spiral computed tomography. What is it, and when is this procedure indicated, what are the contraindications for diagnosis? How is it different from conventional CT and MRI?
What is SCT in modern medicine?
In medicine, this type of research, like MRI, has been used for a relatively short time - less than 30 years. When performing a spiral computed tomography, the patient's body is scanned using X-rays. The latter are transmitted to the monitor for analysis after converting them into electrical impulses. The main feature is that both the table on which the patient lies and the tube rotate during scanning. This technique makes it possible to detect tumors up to 0.1 cm in size.
What organs and systems are being examined?
Spiral computed tomography is an effective diagnostic method that can be used to study almost any human organ and system. Thanks to the minimum slice thickness, it reveals the most minor pathological changes in the body, allowing diagnosis to be made at an early stage and therapy to be started in a timely manner. Not always effective when examining soft tissues.
It should be borne in mind that, from a theoretical point of view, spiral computed tomography can be used to examine any patient, since it has no absolute limitations.
However, there is a list of conditions in which it is not recommended and is possible only after the attending physician has assessed the ratio of potential benefits and probable risks. Such contraindications to SCT include:
- effusion in the pleural cavity;
- pregnancy (in this case it is better to do an MRI);
- fear of confined spaces;
- children under 7 years of age;
- body weight exceeding that specified by the device manufacturer as acceptable;
- lack of physical ability to assume a lying position;
- the patient cannot hold his breath for a long time;
- There are mechanical devices in the human body (for example, a pacemaker is installed in the heart);
- with individual intolerance to the contrast agent.

Spiral computed tomography is acceptable for diagnosing pathological changes in almost any human organ and system. If the patient complains of headaches, visual disturbances, loss of sensation in the limbs, clouding of reason and consciousness, or unexpected paralysis occurs, then a spiral CT scan is recommended. SCT of the brain is indicated in the following cases:
- vascular damage;
- pathologies of the lymphatic system;
- suspicion of pathological processes in the structure of the lungs;
- assessment of brain damage in cases of suspected acute stroke;
- pathologies of the auditory canals, temporal region of the skull, nasal sinuses;
- increased ICP;
- to confirm/refute a brain tumor;
- traumatic brain injury;
- neurotic disorders;
- Anomalies in the development of a child are also a reason to perform an SCT scan of the head;
- deformation of the inner ear, causing a decrease in hearing levels;
- epilepsy (epileptic seizures are also an indication for SCT examination of the brain).
Differences between spiral computed tomography and MRI and CT
SCT and MRI are methods for studying internal organs and systems, which differ in 3 important characteristics:
- principle of operation - MRI diagnostics uses an electromagnetic field, and SCT uses x-rays;
- information content - MRI is used to study soft tissues, SCT - in most cases, to examine hard bone structures;
- duration of the procedure - an MRI can last up to an hour and a half, a spiral study on average lasts several minutes.
Both SCT and conventional computed tomography are types of x-ray examination. The basic principle of operation is almost the same - a layer-by-layer scan of the body or an individual organ is carried out. However, there is a difference between them. The main difference is the thickness of the cut. If with CT its minimum thickness is 10 mm, then SCT allows you to obtain a more accurate picture due to the thickness of the layers of about 3 mm. This is achieved due to the fact that the table with the patient enters the device smoothly (with CT this happens step by step, with the “step” being 1 cm), and the radiation source rotates around it in a spiral.
Research stages

Carrying out spiral tomography, taking into account the time spent on preparation, data processing, formation of orders and recommendations by a radiologist, takes no more than 4 hours. No special preparation is required. The patient is recommended to undergo a preliminary MRI and ultrasound, and should not eat, drink or smoke 4 hours before the examination.
Stages of SCT diagnostics:
- administration of contrast (intravenously or orally);
- placing the patient on a mobile table (since you will need to lie still, in some cases the doctor prescribes sedatives);
- the table moves inside the gantry - “pipe” (the irradiation source rotates along a spiral trajectory);
- a scan is performed (usually the procedure takes from 5 to 30 minutes);
- information is displayed on a computer monitor (if desired, it can be recorded on a portable device);
- The radiologist deciphers the diagnostic result and issues a referral for consultation with specialists.
Examination using SCT is absolutely painless and may cause minimal discomfort associated with being in a confined space.
If the abdominal cavity or chest is being examined, the patient will need to hold his breath for a while.
In order for the interpretation of the study results to be as accurate and reliable as possible, you need to provide the radiologist with your medical card or a report from the attending physician indicating a preliminary diagnosis. Then the doctor will be able to take into account all previous diseases and injuries, as well as the individual structural features of the patient’s body.
What does the photo show?
What does the image that the doctor receives as a result of the procedure show? It allows you to visualize injuries to bones and internal organs, determine the state of lymphoid tissues, identify a tumor, and diagnose pathological processes of both acute and chronic courses. The study also makes it possible to monitor the patient’s condition over time and thus evaluate the effectiveness of the prescribed treatment.
For example, when examining the kidneys, it is possible to identify not only malignant or benign formations in their structure. Polycystic kidney disease, abscesses, and developmental abnormalities are also diagnosed. Kidney tomography is indicated in the postoperative period (if transplantation or removal was performed), as well as during organ biopsy.
How much does SKT cost?
The average cost of spiral computed tomography in Russian clinics is 5 thousand rubles. For scanning one organ you will need to pay from 4 thousand rubles, while diagnostics of the whole body costs three times more - about 13 thousand rubles. The price may vary depending on the region, the qualifications of the specialist and the equipment itself - the results of the study on the latest generation tomograph will be more accurate, but it costs more.
Computed tomography of the liver is a non-invasive and painless procedure for studying this organ. Having received a tomographic report from a radiologist, the attending physician can assess the general condition of the patient, the structural features, development and functioning of the liver. In a short period of scanning time, special X-ray equipment allows you to obtain high-precision images of the organ in different projections layer by layer. The entire operating principle of the tomograph is based on the use of the properties of X-rays, and this method of examining the body is considered safer than conventional radiography due to the lower level of radiation received by the patient in the process.
Computed tomography: what it is, why do it?
Tomographic scanning is the process of passing x-rays through the human body at certain intervals. Specialized equipment - a tomograph ring - rotating around the patient, manages to take a series of images of the organ in sections with a step of 0.5 to 10 mm in one cycle lasting one second. A series of images recorded by a tomograph enters a computer, where the corresponding program creates a three-dimensional, three-dimensional image of the liver and all its deep tissues.
To visualize in more detail the network of blood and lymphatic vessels, as well as neoplasms of any etiology, the method of computed tomography of the liver with contrast is used. The subject is injected with a dye that contains iodine. The drug does not transmit x-rays, so it has a characteristic contrast appearance in the pictures. Based on the characteristics of its distribution in the organ, the radiologist can judge the presence of narrowings or other pathologies in the liver vessels, the degree of spread of metastases, and the possible presence of neoplasms when they are still at the very first stage of their development.
Self-medication has never been welcomed by doctors, and the same statement is true for such specific diagnostic methods as CT. To do a CT scan of the liver, you must first consult with a therapist or specialist and receive an appropriate referral. Tomography is practically not carried out as a preventive manipulation - ultrasound is sufficient for these purposes.
If the doctor has decided on the need for a computed tomography scan of the liver, then he sees an objective need:
- assess the condition of the organ and associated tissues and structures;
- identify tumors, lesions, injuries, bleeding, abscesses, and other types of liver disorders, if radiography or ultrasound cannot provide enough information to make a diagnosis and prescribe treatment;
- carry out preparatory measures for biopsy or aspiration of liver tissue;
- analyze the effectiveness of the treatment or surgical intervention performed;
- clarify the condition of the liver if previously obtained test results, for example, liver tests, are unsatisfactory.
Indications and contraindications for CT scan of the liver
An unpleasant feature of the development of liver diseases is the fact that it contains a small number of nerve endings, so a person cannot always feel that something abnormal is happening to the organ. However, if the patient often complains of pain and heaviness in the liver area, bloating, metallic taste, nausea and bitterness in the mouth, such symptoms are an indication for an ultrasound, based on the results of which the doctor may prescribe a referral for a computed tomography scan.
Other indications for liver CT include:
- detection of organ enlargement for unknown reasons;
- the need to clarify the preliminary diagnosis, for example, cirrhosis or hepatitis;
- identification of pathological formations, the need to clarify their size and extent of distribution;
- suspicion of tumor diseases, the appearance of metastases;
- presence of disturbances in the functioning of liver vessels;
- conducting surgical interventions: doctors prescribe CT scans before surgery, in preparation for it, and after it to assess its effectiveness;
- impaired blood flow and thrombosis in this part of the body;
- infectious and inflammatory processes, polycystic liver disease;
- chronic alcoholism, which, as is known, often provokes irreversible processes in the liver;
- previous abdominal injuries.
There are also situations where the potential risks of tomography are higher than the likely value of the data obtained in the process, or when, due to the nature of the human body, the information content of the study will be too low. In the presence of certain diseases and conditions, CT scanning can generally harm a person. Tomographic scanning of the liver is prohibited:
- for pregnant women and nursing mothers, due to the risk of exposure to the fetus;
- for children under 3 years of age, so as not to expose a very young body to x-rays;
- for diabetes mellitus, acute forms of bronchial asthma;
- in the presence of iodine intolerance, kidney or liver failure, if we are talking about computed tomography with contrast;
- in case of severe general condition of the patient, for example, if he is connected to life support devices;
- in diseases and pathologies associated with the manifestation of hyperkinesis: in such cases, the patient will not be able to ensure complete immobility during the scan, which is why the value of the resulting images will be almost zero.
For obese patients, liver CT remains questionable. On the one hand, it is known that ultrasound is practically uninformative for them, since it poorly visualizes the organ due to the presence of fatty deposits. On the other hand, computer tomographs, in general, are simply not designed to weigh more than 140-180 kilograms. In such cases, the doctor decides at his own discretion how exactly the patient will be examined.
What pathologies can a computed tomography scan of the liver detect?
The results of a CT scan of the liver are pictures and images, analyzing and studying which, a radiologist can identify the following diffuse changes in the liver:
In addition to pathologies and disorders, CT scan of the liver also shows the functional characteristics of the organ, as well as the lesions found in it - tissue density, size, location of tumors or metastases, their depth.
Do I need to prepare for a CT scan of the liver?
Preparation for computed tomography of the liver does not have any features that distinguish it from other types of tomography. It is recommended to conduct the examination on an empty stomach, so you should not eat 2-4 hours before the examination. During the day, you should reduce your fluid intake and completely eliminate alcohol intake.
It is imperative to inform the doctor about all medications used by the patient. It may be necessary to take a break from taking them for a while before the study.
Patients undergoing a contrast-enhanced CT scan will need to have their creatinine tested. In some cases, if the patient cannot give an accurate answer about whether he is allergic to iodine or other substances, the doctor may additionally prescribe appropriate tests - allergy tests.
How does the CT scan process work?
The person being examined must remove all metal objects, accessories and jewelry and leave them along with all gadgets outside the door of the diagnostic room. He changes into special clothes - spacious, comfortable, made of cotton fabric and without metal parts, after which he is placed on the tomograph table and takes a comfortable, relaxed position.
If the procedure involves the introduction of a contrast agent, it is injected with a syringe or catheter before moving the table with the subject deep into the tomograph arch. For 15 minutes (in rare cases - up to half an hour) the patient is under the targeted influence of x-rays. All that is required of him is not to move, and strictly follow the doctor’s instructions when he asks him to hold his breath.
During the process, the device buzzes, crackles, and makes a characteristic noise. For patients for whom this fact causes discomfort, the nurse has earplugs or headphones prepared.
Doctors and technicians are in the next room - from there they monitor the progress of the procedure and can communicate with the patient. If a person feels a sharp malaise, pain, or deterioration of health during the process, he immediately reports this to the doctor.
A series of images taken during the examination are recorded in computer media and processed by a special program that produces ready-made layer-by-layer images.
Tomographic scanning of the liver occurs in segments closely related to the duct system, of which there are five in the liver. This technique greatly simplifies the examination, further reading of the results and the radiologist’s conclusions.
Benefits of performing a liver examination using a CT scanner
The development of this device at one time became a real breakthrough, and CT is still considered a way to obtain the clearest and most informative images of human internal organs and their deep structures. A qualified radiologist can not only detect the presence of diseases and pathologies in images, but also outline the range of reasons that led to their appearance.
Examination using a tomograph is non-invasive, painless and more accessible than, for example, MRI. Its implementation usually does not threaten the patient with any complications if all preparation requirements have been met and the absence of contraindications has been determined.
In some emergency cases, the fact that the examination itself takes 15 minutes also plays an important role. If a patient has acute injuries, bleeding and damage, every second of delay becomes fatal for him, so the ability to obtain examination results in such a short period of time is highly valued by doctors.
Computed tomography is undoubtedly safer than radiography, as it exposes the patient to significantly less radiation.
The diagnosis of liver tumors has made great progress with the advent of computed tomography. In cases where tests, ultrasound and radiography cannot provide the doctor with complete and accurate information about the presence, extent and nature of liver damage, prescribing a CT scan is a real way out. Computer diagnostics using the properties of X-rays makes it possible to identify pathological processes in the liver even at the early stages of their development, and with minimally noticeable manifestations.