Use of dexamethasone for brain tumors. Treatment of tumor metastases to the brain
15/12/12
Hello. My father has a brain tumor. The pathological diagnosis after surgery in March 2011 was gemistocytic astrocytoma with petrific endothelial proliferation in single vessels. They said that the tumor was deep and they couldn’t remove it all. A week ago he finished his second radiation treatment. After radiation, injections of the steroid dexamethasone were prescribed to relieve swelling. But this drug has so many side effects that it’s scary to start taking these injections. Please tell me what drugs (their names) are used in such situations in Israel. I want to read about them. Reviews about dexamethasone are terrible. Maybe there are better drugs.
Thank you in advance. Natasha
Hello, Natasha.
First of all, please accept my sympathy regarding my father's illness.
Secondly, steroid drugs are given to reduce intracerebral pressure. Dexamethasone, or another steroid in such a situation, is a mandatory drug for use, and there is no alternative to it. But when used correctly, it does not cause any special complications, and if it does, there are ways to combat them.
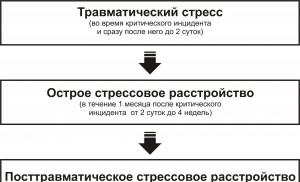
Synthetic fluorinated corticosteroids with pronounced anti-inflammatory, antiallergic, immunosuppressive effects. Inhibits the release of ACTH, has a slight effect on blood pressure levels and water-salt metabolism. 35 times more active than cortisone and 7 times more active than prednisolone. Induces the synthesis and secretion of lipomodulin, which inhibits phospholipase A2, inhibits the formation of arachidonic acid metabolites, prevents the interaction of IgE with receptors of mast cells and basophilic granulocytes and activation of the complement system, reduces exudation and capillary permeability. The immunosuppressive effect is due to inhibition of the release of lymphocyte and macrophage cytokines. Affects protein catabolism, stimulates gluconeogenesis in the liver and reduces glucose utilization in peripheral tissues, suppresses the activity of vitamin D, which leads to impaired calcium absorption and more active excretion. Suppresses the synthesis and secretion of ACTH and, secondarily, the synthesis of endogenous corticosteroids. Unlike prednisolone, it does not have mineralocorticoid activity; inhibits the function of the pituitary gland.
After oral administration, it is quickly and completely absorbed from the digestive tract. The maximum concentration in blood plasma is achieved after 1-2 hours. About 60% of the active substance is bound to blood plasma albumin. The half-life is more than 5 hours. It is actively metabolized in many tissues, especially in the liver under the influence of cytochrome-containing enzymes CYP 2C, and is excreted in the form of metabolites in feces and urine. The half-life is on average 3 hours. In severe liver diseases, during pregnancy, and while taking oral contraceptives, the half-life of dexamethasone increases.
After instillation into the conjunctival sac, dexamethasone penetrates well into the epithelium of the cornea and conjunctiva; therapeutic concentrations are achieved in the aqueous humor of the eye. The duration of the anti-inflammatory effect after instillation of 1 drop of 0.1% solution or suspension into the eye is 4-8 hours.
Indications for use of the drug Dexamethasone
Swelling of the brain caused by a tumor resulting from traumatic brain injury, neurosurgery, brain abscess, encephalitis or meningitis; progressive rheumatoid arthritis during exacerbation; BA; acute erythroderma, pemphigus, initial treatment of acute eczema; sarcoidosis; nonspecific ulcerative colitis; severe infectious diseases (in combination with antibiotics or other chemotherapeutic agents); palliative therapy of a malignant tumor. Also used for replacement therapy for severe adrenogenital syndrome.
Periarticular infiltration therapy is carried out for periarthritis, epicondylitis, bursitis, tendovaginitis, intra-articular administration - for arthritis of non-microbial etiology; in ophthalmology - in the form of subconjunctival injections for inflammatory eye diseases (after injuries and surgical interventions).
Eye drops - scleritis, episcleritis, iritis, optic neuritis, sympathetic ophthalmitis, conditions after trauma and ophthalmic surgery.
Use of the drug Dexamethasone
Orally, administered intravenously and intramuscularly, intra- and periarticularly, subconjunctivally, used in the form of eye drops.
For severe cerebral edema, treatment usually begins with intravenous administration of dexamethasone; when the condition improves, they switch to oral administration of 4-16 mg/day. For milder cases, dexamethasone is prescribed orally, usually 2-8 mg of dexamethasone per day.
For rheumatoid arthritis during an exacerbation, asthma, acute skin diseases, sarcoidosis and acute ulcerative colitis, treatment begins with a dose of 4-16 mg/day. For planned long-term therapy, after elimination of acute symptoms of the disease, dexamethasone should be replaced with prednisone or prednisolone.
For severe infectious diseases (in combination with antibiotics and other chemotherapeutic agents), 8-16 mg of dexamethasone per day is prescribed for 2-3 days with a rapid dose reduction.
For palliative therapy of a malignant tumor, the initial dose of dexamethasone is 8-16 mg/day; for long-term treatment - 4-12 mg/day.
Adolescents and adults with congenital adrenogenital syndrome are prescribed 1 mg/day, and mineralocorticoids are additionally prescribed if necessary.
Dexamethasone is administered orally after meals, preferably after breakfast, with a small amount of liquid. The daily dose should be taken once in the morning (circadian regimen of therapy). When treating cerebral edema, as well as during palliative therapy, it may be necessary to divide the daily dose into 2-4 doses. After achieving a satisfactory therapeutic effect, the dose should be reduced to the minimum effective maintenance dose. To complete the course of treatment, this dose continues to be gradually reduced to restore the function of the adrenal cortex.
For local infiltration administration, 4-8 mg is prescribed, for intra-articular administration into small joints - 2 mg; for subconjunctival - 2-4 mg.
Eye drops (0.1%) are used in a dose of 1-2 drops at the beginning of treatment every 1-2 hours, then, when the severity of inflammatory phenomena decreases, every 4-6 hours. Duration of treatment - from 1-2 days to several weeks depending on the effect obtained.
Contraindications to the use of the drug Dexamethasone
1. Indications
A. Biopsy data. Despite the advances of CT and MRI, these methods cannot replace histological diagnosis. Often, patients with suspected malignant glioma have treatable meningiomas, lymphomas, or brain abscesses. A biopsy also allows one to determine the prognosis and indications for radiation therapy and chemotherapy.
b. Reversibility of neurological defects. If neurological disorders are caused by tumor infiltration or destruction of brain matter, then they persist even after removal of the tumor. If they are associated with compression of the surrounding tissue, then after surgery they may disappear. If it is impossible to completely remove the tumor, partial resection is performed to reduce compression of the brain substance. For benign tumors that cannot be completely removed, periodic reoperations significantly increase the length and quality of life.
V. Possibility of cure. For many extracerebral tumors (meningiomas, schwannomas, pituitary adenomas), it is possible to completely remove the tumor and avoid relapses. At the same time, only a few intracerebral tumors are amenable to surgical treatment.
d. The surgical risk depends on the patient’s condition, concomitant diseases and tumor location. Resection itself, as well as compression, overstretching or devascularization of the brain substance can lead to irreversible damage. If the localization of a benign tumor is unfavorable, even its partial resection can be dangerous, and complete removal impossible. This primarily applies to tumors located in the hypothalamus and third ventricle, trunk, clivus and foramen magnum, and also closely associated with large vessels (for example, the carotid artery or sagittal sinus). On the contrary, even with radical removal of tumors from “silent” areas of the brain (for example, the anterior parts of the frontal and temporal lobes, cerebellar hemispheres), the risk of neurological disorders is low. The surgical risk also depends on the size of the tumor. Resection of large tumors involves significant damage to healthy areas of the brain, which increases the likelihood of an unfavorable outcome.
2. Types of operations. The use of magnifying technology, in particular an operating microscope, has made it possible to stereoscopically visualize previously inaccessible structures and dramatically reduce the incidence of surgical complications and deaths.
A. For tumors located on the surface and deep in the hemispheres, craniotomy is most often performed.
b. Newer CT-guided techniques are expanding the capabilities of stereotactic brain biopsy, making it possible to avoid craniotomy. Stereotactic biopsy is indicated for deep, inaccessible space-occupying lesions, as well as in the absence of neurological symptoms, when the risk of craniotomy outweighs the benefit of the operation. Many primary brain tumors are heterogeneous, and stereotactic biopsy may produce tissue samples that do not provide insight into the structure of the entire tumor.
V. The best method is complete removal of the tumor. If this is not possible, then the most extensive resection of the tumor is desirable, since this reduces ICP and increases the effectiveness of adjuvant therapy (radiation or chemotherapy).
3. Surgical complications
A. Hemorrhages. Intracerebral hemorrhages can occur both in the surgical area and outside it, often due to tension in an artery or vein. Postoperative hemorrhage is usually venous and extracerebral (sub- or epidural). Removal of the hematoma is indicated if it leads to disturbances of consciousness or focal symptoms.
b. Cerebral edema is usually present before surgery, but during surgery it can increase sharply as a result of injury, compression of veins, or overhydration. Prescribing corticosteroids several days before surgery reduces the initial cerebral edema. To combat cerebral edema, mannitol is administered intravenously during surgery.
V. Infection. The risk of wound infection increases with prolonged operations and implantation of foreign materials (for example, a shunt). The causative agents are usually aerobic microorganisms (eg, gram-positive cocci, especially staphylococci). However, prophylactic antibiotics are not indicated during surgery for brain tumors.
d. After supratentorial operations (usually within the first month), partial or generalized epileptic seizures may develop. The likelihood of seizures depends on the location and histology of the tumor, as well as surgical complications. Recommendations for their prevention are as follows:
1) Anticonvulsants during and after surgery are prescribed to all patients with a history of seizures.
2) In other cases, prophylactic anticonvulsant therapy is not indicated. Most studies have demonstrated that prophylactic anticonvulsant therapy does not reduce the incidence of postoperative seizures. With radiation therapy, the risk of side effects from anticonvulsants increases.
3) The risk of postoperative seizures is highest with parasagittal and falx meningiomas. In these cases, prophylactic anticonvulsant therapy is started before surgery and continued for at least 4 months after surgery.
d. Communicating hydrocephalus. Entry of blood into the CSF during surgery can lead to impaired absorption of CSF by the arachnoid villi and to communicating hydrocephalus. This complication usually resolves on its own, with only rare cases requiring bypass surgery.
e. Neuroendocrine disorders
1) ADH hypersecretion syndrome can develop after any brain surgery. In this regard, in the postoperative period it is necessary to carefully monitor the content of electrolytes, since water retention and, as a consequence, hyponatremia lead to severe cerebral edema. Treatment: fluid restriction. This complication usually resolves within 1-2 weeks.
2) Surgeries in the area of the hypothalamus and pituitary gland can cause hypopituitarism of varying severity and diabetes insipidus.
IV. BRAIN TUMORS IN ADULTS
A. Malignant gliomas
1. Prevalence. The most common primary brain tumors in adults are malignant gliomas, which include malignant astrocytoma and glioblastoma. About 5,000 new cases of gliomas are reported annually in the United States. The peak incidence occurs at 45-55 years of age; men get sick more often than women (the ratio between them is 3:2). The tumor can be localized in any part of the hemispheres, but most often in the frontal and temporal lobes. In the cerebellum, brainstem, and spinal cord, malignant gliomas are rare in adults.
2. Forecast. Malignant gliomas are rapidly growing tumors that inevitably lead to death. Although they are highly invasive in the central nervous system, these tumors do not metastasize outside the nervous system. The two-year survival rate from diagnosis is 40% for malignant astrocytoma and 10% for glioblastoma. An important prognostic factor is age. Regardless of treatment, patients under 45 years of age live significantly longer than those over 65 years of age. Unfavorable prognostic signs include mental and neurological disorders.
3. Surgical treatment. The operation of choice is craniotomy with the most extensive resection of the tumor. This operation reduces compression of the brain and is the most reliable way to obtain sufficient samples of tumor tissue for histological examination. After extensive resection of malignant glioma, the postoperative period is more favorable, and life expectancy is higher than after limited resection or biopsy.
On CT or MRI, malignant gliomas often appear circumscribed, but in fact they always infiltrate adjacent tissues or spread to the other hemisphere through cerebral commissures. Therefore, even in cases where neurosurgeons optimistically report complete tumor removal, malignant gliomas almost always recur, usually within a few months. Thus, surgery is not a radical treatment for these tumors.
4. Radiation therapy
A. Radiation doses and fields. Malignant gliomas are insensitive to radiation. However, studies conducted in the 70s showed that life expectancy with postoperative general cerebral irradiation (for 5-6 weeks) at a dose of 55-60 Gy is higher than with a dose of less than 50 Gy. The average life expectancy for glioblastoma multiforme after surgery and radiation is about 40 weeks. Currently, general brain irradiation (at a dose of 40 Gy) is combined with targeted irradiation of the tumor bed (20 Gy) in order to minimize the radiation dose to unaffected areas of the brain. If the dose received by the tumor is less than 60 Gy, life expectancy appears to be reduced; at high doses, neurotoxicity develops, but life expectancy does not increase.
In tissue radiation therapy, radioactive implants are stereotaxically injected into the brain. In this case, the tumor receives a much higher dose of radiation, and healthy tissues receive a much lower dose. The effectiveness of tissue radiation therapy has not yet been sufficiently determined, but sometimes with the help of this method it is possible to improve the quality and life expectancy of tumor recurrences after conventional radiation therapy.
b. Complications
1) When exposed to standard doses of radiation, the risk of ordinary radiation damage to the brain is small. However, approximately 40% of patients with malignant gliomas who survive more than 18-24 months after total brain irradiation develop radiation-induced dementia. In this regard, the dose of general brain irradiation is reduced by adding targeted irradiation of the tumor bed.
2) Radiation may contribute to brain swelling. In this regard, corticosteroids are given throughout the course of radiation therapy, and only a few weeks before its end, when the patient’s condition is stable, they are gradually withdrawn.
3) All patients experience hair loss during radiation therapy, but in many cases it grows back after a few months.
4) Perhaps the most painful thing for the patient is the need to stay in the hospital or come to it every day for another 5-6 weeks. Therefore, when deciding on the advisability of radiation therapy, everything should be carefully weighed, taking into account that the prognosis for glioblastoma is unfavorable.
V. Efficiency. Radiation therapy is not a cure, but it reduces symptoms and increases life expectancy. That is why it is traditionally prescribed after surgery for malignant gliomas (see Table 11.2).
5. Chemotherapy. Due to the ineffectiveness of surgical and radiation treatment of malignant gliomas, new chemotherapeutic drugs are being studied, but the results of their use (as with other solid tumors) are quite modest.
A. Nitrosourea derivatives and related drugs. The small fat-soluble nitrosourea molecules are able to cross the intact blood-brain barrier and appear to reach therapeutic concentrations in the tumor. Nitrosourea derivatives are the only agents that have been shown to be effective in large controlled trials. In a large randomized study of carmustine administration (in addition to surgical and radiation treatment), a significant increase in average life expectancy (from 38 to 51 weeks) and two-year survival (15%) was obtained. Carmustine is the most effective remedy for malignant gliomas. It is administered intravenously at a dose of 200 mg/m2 every 8 weeks (if the blood picture is normalized by the time of the next administration). Leukopenia and thrombocytopenia usually occur in the first 2-4 weeks after each administration of the drug. With repeated administrations, a cumulative inhibition of hematopoiesis occurs. Major side effects also include liver dysfunction and pulmonary fibrosis. Lomustine (for oral use) and the urea-like drugs procarbazine and streptozocin are probably no less effective than carmustine.
b. Recommendations for the use of chemotherapy. Chemotherapy (in particular, carmustine or lomustine) is not recommended for all patients with malignant gliomas - chemotherapy does not significantly improve the prognosis, and the risk of severe side effects is justified only in young patients with minimal neurological disorders.
V. Immunotherapy is theoretically capable of exerting specific antitumor effects without causing significant damage to normal areas of the brain. Methods such as active immunization with irradiated autologous tumor cells, adoptive immunotherapy (intratumoral injection/infusion of immune cells), treatment with humoral immunomodulators (eg, interferons) and monoclonal antibodies are being experimentally studied.
d. Tumor recurrence. Several weeks or months after any type of treatment, neurological symptoms increase in patients, and CT or MRI reveals a recurrence of glioma, usually in the same place or a few centimeters from it. Metastasis to other parts of the central nervous system or beyond is rare. Repeated surgery and the administration of high doses of corticosteroids reduce the displacement of brain structures and reduce ICP, but these measures can prolong life by only 3-4 months. Additional radiation therapy is ineffective and has a damaging effect on normal brain tissue.
d. Experimental methods of treatment. Many medical centers are studying new chemotherapy drugs and other treatments for recurrent malignant gliomas (eg, tissue radiation therapy, hyperthermia, immunotherapy). Patients without severe neurological defects and who agree to any treatment can be referred to one of these centers. Perhaps someday new methods will be able to help patients with malignant gliomas.
B. Supratentorial astrocytomas and oligodendrogliomas
1. Clinical picture. Grade 1 and 2 astrocytomas (well-differentiated astrocytomas) and oligodendrogliomas of the cerebral hemispheres are less common in adults than malignant gliomas, accounting for only 10% of primary brain tumors. These tumors usually manifest as transient disturbances (for example, an epileptic seizure), while there are usually no focal symptoms, and CT and MRI reveals a supratentorial lesion that does not accumulate contrast and hardly displaces adjacent structures.
2. Surgical treatment. Because these tumors may remain silent for many years, some people prefer to withhold surgery and rely only on anticonvulsants until the tumor becomes large or focal symptoms appear. If the tumor is located in an accessible location, then a biopsy followed by extensive resection is indicated. It is usually not possible to completely remove these tumors, since their growth is infiltrative.
3. Postoperative radiation therapy(55 Gy per tumor bed) allows for some time to delay tumor recurrence, but it remains unknown whether it increases long-term (10-year) survival and whether the benefits of radiation outweigh the risk of radiation dementia (see paragraph IV.A.4. b.1). To address the issue of adjuvant radiation therapy for these tumors, prospective studies are being conducted.
4. Chemotherapy is ineffective.
5. The prognosis is highly variable. In studies on large heterogeneous groups of patients, the average life expectancy after surgery was about 5 years, but the range of this indicator is very large. Some patients die within the first year, while others (a minority) live over 10 years without signs of progression. The vast majority eventually develop a relapse with an increase in neurological symptoms. This is often associated with tumor degeneration into glioblastoma. If the tumor recurs, repeat resection is advisable.
B. Primary CNS lymphomas
1. Prevalence. Primary CNS lymphomas are non-Hodgkin, usually B-cell, lymphomas that occur in the absence of generalized lymphoma. Previously, they were rare (1% of all primary brain tumors), but over the past 15 years, the incidence of primary CNS lymphomas, even in people with normal immunity, has tripled. In addition, the risk of lymphoma is higher in patients with immunodeficiency - congenital (for example, with Wiskott-Aldrich syndrome) or acquired (for example, with AIDS or organ transplantation). Primary CNS lymphomas develop in 3% of AIDS patients, including before diagnosis. In the 1990s. A further increase in the incidence of primary CNS lymphomas is expected.
2. Clinical picture. There are four clinical variants of primary CNS lymphomas.
A. The most common are single or multiple (in approximately the same percentage of cases) intracerebral nodes.
b. The second most common is diffuse meningeal or periventricular infiltration (can be combined with a nodular form).
V. Retinal or vitreous infiltration may precede or follow parenchymal or meningeal tumors. Therefore, regular slit-lamp examinations are indicated for primary CNS lymphomas.
d. Lymphomas of the spinal cord (rare).
3. Diagnostics. In the presence of a single parenchymal node, its biopsy and removal are indicated. Unfortunately, surgical treatment is not possible for invasive growth or multiple lesions. Stereotactic biopsy or cytological examination of CSF (including immunocytological tests) is used to diagnose multifocal or diffuse meningeal lesions. In patients with AIDS, differential diagnosis is necessary between primary lymphoma and other multifocal lesions of the central nervous system, including cerebral toxoplasmosis and brain abscesses.
4. Treatment. When prescribing high doses of corticosteroids (for example, 6 mg dexamethasone 4 times a day), improvement and reduction in tumor size on CT and MRI may be observed. This is due not only to the decongestant, but also to the cytotoxic effect of these hormones on lymphoid cells. Various methods of radiation therapy are also used depending on the clinical situation and the extent of the lesion (irradiation of the tumor bed, total irradiation of the brain and spinal cord). Since they are ineffective, methods of pre- and post-radiation chemotherapy are being developed. For diffuse meningeal infiltration, methotrexate is used intrathecally (see section IV.G.2).
5. Forecast. The average life expectancy after a course of corticosteroids and radiation in patients with normal immunity is 12-24 months, with AIDS - much less. After 1 year, 60% of survivors have extensive tumor dissemination throughout the central nervous system, and 10% have generalized lymphoma. This proves the need for chemotherapy. Prescribing nitrosourea drugs, high doses of methotrexate under the cover of calcium folinate, or polychemotherapy can increase life expectancy in primary CNS lymphomas.
G. Meningiomas
1. General information. Meningiomas are histologically benign tumors of arachnoid endothelial cells. They rank second in prevalence among primary intracranial tumors in adults. The peak incidence occurs between 30 and 50 years of age. Unlike other primary brain tumors, meningiomas are more common in women than in men (2:1 ratio). Cytogenetic studies have shown that most patients with meningiomas have multiple deletions on chromosome 22. Progesterone receptors are often found on meningioma cells, which may play a role in tumor growth.
2. Localization. Meningiomas can appear anywhere where arachnoid endothelial cells are present, but most often they are localized on the convexital surface of the brain (50% are found in the parasagittal zone, on the lateral surface of the hemispheres or in the falx region) or on the base of the brain (40% grow in the cribriform plate , wings of the sphenoid bone or in the suprasellar zone). Meningiomas of the foramen magnum, posterior fossa, or ventricular system are rare.
3. Surgical treatment. Meningiomas are well-circumscribed, slow-growing tumors. They can infiltrate the dura mater, its sinuses, or the bones of the skull, but usually do not grow into the brain. In this regard, meningiomas, unlike the tumors described above, can often be completely removed.
4. Forecast, usually favorable; After tumor removal they usually live a long time. However, the likelihood of recurrence and life expectancy vary depending on the location of the tumor and the possibility of complete removal. In one large study, meningioma was resected within apparently healthy tissue in approximately 60% of cases. Meningiomas of the convexital surface, parasagittal region, area of the wings of the sphenoid bone and cribriform plate were more often able to be completely removed than tumors of the base of the brain. In the vast majority of patients with meningiomas of the convexital surface of the brain, a complete cure was achieved. 10% of patients with “completely removed tumor” experienced recurrence, probably because tumor cells were still left behind during surgery. The period from surgery to detection of relapse was 1 year - 13 years (average 4-5 years). In many cases, reoperation was successful. In the group with obviously incomplete resection, relapses were noted in 40% of cases, but even in this group the results of the operation were good: 25% of patients lived more than 10 years.
5. Histologically meningiomas are divided into endotheliomatous, transitional and angiomatous. The prognosis for all these options is the same. Rarely occurring hemangiopericytoma and malignant meningioma recur much more often and faster than benign meningiomas.
6. Radiation therapy performed if tumor recurrence is accompanied by neurological symptoms, and reoperation is contraindicated or cannot be performed in full. Retrospective studies show that in patients with subtotal resection of meningioma, life expectancy can be increased and recurrence delayed with adjuvant local irradiation.
7. Incidentally discovered meningiomas. With the advent of CT and MRI, meningiomas are sometimes detected during examinations for other diseases (for example, traumatic brain injury or stroke). The tactics of their treatment depend on the size and location of the tumor, the presence or absence of edema and displacement of brain structures, and the age of the patient. If there is severe perifocal edema, the meningioma can be removed immediately. In the case of small asymptomatic tumors, dynamic monitoring, including CT, is recommended, and surgery is indicated only if signs of progression appear.
D. Schwannomas(neurinomas) of the vestibulocochlear nerve
1. Prevalence. Schwannomas, tumors growing from Schwann cells of peripheral nerves, are often found in the cranial cavity. They usually arise from the vestibulocochlear nerve and are localized in the cerebellopontine angle. Schwannomas are the most common tumors of the cerebellopontine angle, but meningiomas, gliomas, and cholesteatomas also occur in this region. Schwannomas of the vestibulocochlear nerve account for 8% of brain tumors. They appear more often in middle age, less often in children. In 5-10% of cases they occur against the background of the central form of neurofibromatosis; however, they are often bilateral and can be combined with multiple schwannomas of the cranial and spinal nerves, meningiomas or gliomas.
2. Diagnostics. Early symptoms of the tumor are associated with damage to the vestibulocochlear nerve (hearing loss, tinnitus, imbalance); damage to the trigeminal nerve (lack of corneal reflex, numbness of the face), facial nerve and ataxia join later. The best diagnostic method is MRI with contrast, which detects even small intracanalicular tumors.
3. Treatment
A. Surgery
1) Schwannomas grow slowly, and diagnosis is often made several months or years after the first symptoms appear. Typically, the tumor is surrounded by a capsule and therefore compresses, but does not infiltrate, the adjacent nervous tissue. Tumors smaller than 2 cm can be completely removed, but larger tumors can only be partially resected in most cases. Therefore, the condition for complete tumor removal and cure is early diagnosis.
2) The frequency of surgical complications also depends on the size of the tumor. For tumors smaller than 2 cm, the incidence of serious complications is below 5%, for tumors larger than 4 cm - above 20%. Without treatment, intracranial hypertension and brainstem compression eventually develop, leading to death. All this emphasizes the importance of early diagnosis.
3) Surgical tactics depend on the size of the tumor, the preservation of hearing and the experience of the surgeon. Recent advances in diagnostics and surgical technique have made more complete resection possible. During the operation, it is usually possible not to damage the nearby facial nerve, although irreversible paresis of the facial muscles often develops after the operation. The vast majority of patients lose hearing as a result of the operation.
b. Standard radiation therapy does not improve prognosis unless the tumor is completely removed.
V. Stereotactic radiation surgery using a gamma knife, a beam of finely focused gamma rays aimed at the tumor, is a promising treatment option, especially in the elderly and those with severe comorbidities that increase the risk of surgery.
E. Pituitary adenomas
1. Classification. Pituitary adenomas are classified according to functional (depending on the secreted hormone) or anatomical principle.
A. Functional classification
1) Hormonally inactive adenomas.
2) Hormonally active adenomas (secreting increased amounts of prolactin, ACTH or growth hormone). The most common are prolactinomas and hormonally inactive adenomas.
b. Anatomical classification
1) Microadenomas (diameter less than 10 mm).
2) Diffuse macroadenomas (surrounded by the dura mater and spreading supra- and parasellar).
3) Invasive macroadenomas (infiltrating the dura mater, bone tissue or brain matter).
2. Clinical picture
A. Microadenomas
1) With hormonally inactive microadenomas, the course is asymptomatic.
2) Hyperprolactinemia is diagnosed by measuring the morning basal prolactin level (normally less than 15 ng/ml). A level above 100 ng/ml almost definitely indicates a tumor. Levels of 15 to 100 ng/mL can also result from a pituitary tumor, but are more often due to medications (eg, phenothiazines, antidepressants, estrogens, metoclopramide) or diseases that impair the suppression of prolactin secretion by the hypothalamus.
3) Hyperprolactinemia may be asymptomatic, but usually causes amenorrhea and galactorrhea in women. Approximately 25% of cases of secondary amenorrhea and galactorrhea are caused by prolactinoma. In men, the first signs of hyperprolactinemia are impotence and loss of libido. Later they are joined by gynecomastia and galactorrhea.
b. Macroadenomas. Large tumors compress healthy pituitary tissue, causing hypopituitarism of varying severity. First, deficiency of gonadotropic hormones usually develops, later ACTH deficiency develops. Tumor spread beyond the sella turcica leads to compression of the optic chiasm and progressive visual impairment, often beginning with bitemporal upper quadrant hemianopsia. Subsequently, the tumor can invade the cavernous sinus, third ventricle, hypothalamus and temporal lobe. Usually the first complaint is blurred vision, in 20% of cases - headache.
V. Even small tumors that secrete ACTH or GH cause severe endocrine disorders (Cushing's disease or acromegaly).
3. Diagnostics. High-resolution CT (with or without contrast) allows you to see on horizontal or frontal sections a space-occupying formation in the area of the sella turcica, the bone structure of the sella and the sphenoid sinus. Using MRI, in addition to horizontal and frontal images, you can also obtain sagittal images of the brain. MRI gives worse images of bone tissue than CT, but it shows the arteries adjacent to the pituitary gland. This allows us to exclude an aneurysm, which sometimes imitates a tumor.
4. Treatment depends on the size of the tumor and the endocrine and visual disturbances it causes.
A. Surgical treatment is indicated for tumor spread beyond the sella turcica, signs of which may include damage to the optic chiasm or involvement of other cranial nerves. The introduction of the dopamine agonist bromocriptine into practice made it possible to manage conservative therapy in many patients with prolactinomas (see paragraph IV.E.4.c).
1) With the transsphenoidal approach, the incidence of complications and mortality is significantly lower than with the transcranial approach. The use of an operating microscope makes it possible to remove both macro- and microadenomas without damaging normal pituitary tissue.
2) Modern microsurgical techniques have reduced the incidence of postoperative complications to 1%. After decompression and tumor removal, vision improves in 70-80% of patients, and is completely restored in almost 50%. The likelihood of vision restoration depends on the duration of the visual impairment. Endocrine disorders can also regress (for example, after removal of a tumor, infertility is cured in 70% of cases).
3) During surgery, corticosteroids are administered to prevent adrenal insufficiency. After surgery, the degree of dysfunction of the pituitary gland is assessed and, if necessary, replacement therapy is prescribed. In the postoperative period, diabetes insipidus may develop, usually transient.
4) If the adenoma extends beyond the sella turcica, it often cannot be completely removed; in these cases, relapse is likely.
b. Postoperative irradiation can significantly reduce the recurrence rate after partial resection (in one study - from 42 to 13%). Usually 50-60 Gy is prescribed over 5-6 weeks. The magnitude of the irradiation field is determined depending on the results of CT and MRI and operational data. Gamma Knife is used for small tumors (especially those causing acromegaly or Cushing's disease) that have recurred after surgery.
V. Conservative treatment with bromocriptine. Normally, the secretion of prolactin is suppressed by the hypothalamic neurotransmitter dopamine. The synthetic dopamine agonist bromocriptine causes a significant decrease in prolactin levels in both healthy people and patients with prolactinoma.
1) Treatment of patients with prolactinoma begins with the use of bromocriptine (usually 2.5-5 mg 3 times a day). In most cases, success can be achieved without surgery. In 80% of women with amenorrhea and galactorrhea, symptoms disappear and infertility is cured.
2) Women suffering from infertility should be reminded of the possibility of pregnancy during treatment. They should use non-hormonal methods for contraception. If you want to get pregnant, contraception methods are not used. If menstruation is delayed by 48 hours, bromocriptine can be discontinued. At the same time, during pregnancy, the condition of patients can worsen due to tumor growth and progression of symptoms (during pregnancy, even in healthy people, the volume of the pituitary gland can double). In such cases, bromocriptine can be prescribed again, since it does not have a damaging effect on the fetus. Such exacerbation during pregnancy with microadenomas develops in 1% of cases, but with macroadenomas - in 25%. Therefore, if a patient who wants to become pregnant has a macroadenoma, it is usually recommended to remove it.
3) Large diffuse or invasive prolactinomas can be significantly reduced as a result of treatment with bromocriptine, while visual impairment and endocrine disorders regress. In most clinics, surgery is still considered the method of choice for such adenomas, but even in this case, bromocriptine can be used as adjuvant therapy; For many patients, bromocriptine alone is sufficient.
4) After subtotal resection of large tumors, bromocriptine is used in combination with or instead of radiation therapy.
5) Sometimes, under the influence of bromocriptine, somatotropinomas and hormonally inactive adenomas can decrease, but in these cases the effect of the drug is less predictable. Somatotropinomas can decrease with the administration of octreotide, an analogue of somatostatin.
G. Metastatic brain tumors. Metastases into the substance and membranes of the brain are a common complication of malignant neoplasms. At autopsy they are found in 15-20% of patients who died from malignant neoplasms. Brain metastases are most common in lung cancer, breast cancer and melanoma, but are possible in almost all malignant tumors. At the same time, the development of neurological symptoms in a cancer patient can be caused not only by metastases, but also by a number of other reasons (see Table 11.3).
There are two main types of metastatic brain lesions: intracerebral nodes and diffuse tumor infiltration of the meninges. Sometimes they can be combined. However, their clinical presentation and treatment methods differ significantly, and therefore they are considered separately.
1. Intracerebral metastases
A. Diagnostics. Intracerebral nodes are the most common type of brain metastases. Metastasis occurs by hematogenous route. The frequency of lesions in a particular part of the brain approximately corresponds to the intensity of its blood supply (cerebral hemispheres, less often the cerebellum, and even more rarely the brain stem). Clinical manifestations of metastases, as with primary brain tumors, are caused by increased ICP, damage to pathways, cerebral edema or epileptic seizures. The most common symptoms are headaches, mental disorders, paresis and imbalance. In approximately 40% of cases, CT detects a single metastasis, in 60% - multiple nodes. MRI has higher sensitivity and detects small multiple metastases even in cases where only one lesion is visible on CT.
b. Intracerebral metastases as the first manifestation of a malignant neoplasm. If a patient with an established diagnosis of a tumor develops neurological symptoms, an immediate examination is necessary to identify intracerebral metastases. However, sometimes such metastases are the first manifestation of a malignant neoplasm. Therefore, when a brain tumor is detected, its metastatic nature should be excluded.
Before surgery for a suspected primary brain tumor, it is necessary to conduct a thorough general examination and laboratory and instrumental studies (complete blood count, urine test, fecal occult blood test, biochemical indicators of liver function, chest x-ray). Since almost all intracerebral metastases are of hematogenous origin, there is a high probability that either the primary tumor or metastases will be found in the lungs. If routine tests and chest X-ray are inconclusive, a chest CT scan is indicated. Other research methods rarely help in diagnosing the primary tumor unless the history or general examination reveals any additional symptoms.
V. Corticosteroids (see also section III.A.1). High doses of corticosteroids reduce brain swelling, thereby providing temporary relief. Indications for corticosteroid therapy are the detection of displacement of brain structures or cerebral edema on CT or MRI; If such therapy is started, it is continued in the pre- and postoperative period and during radiation therapy. If usual doses of dexamethasone (4-6 mg every 6 hours) do not relieve intense headaches or prevent further progression of symptoms, ultra-high doses (25 mg every 6 hours) sometimes help.
d. Surgical treatment of single metastases. Sometimes it is possible to completely remove single metastases located in relatively safe areas of the brain (for example, in the frontal lobe, temporal lobe of the non-dominant hemisphere, cerebellum). After surgery, total brain irradiation (25-40 Gy over 2-4 weeks) is performed to suppress remaining tumor cells or undetected micrometastases. Single metastases are removed if there is no severe general disease or if there is doubt about the nature of the brain tumor. Recent randomized trials have shown that resection of single metastases is associated with greater symptomatic improvement and longer survival than radiotherapy alone.
e. Radiation therapy is performed for multiple metastases and single inoperable metastases. This is one of the few cases when radiation therapy is possible without histological examination of the tumor. The presence of intracerebral metastases is preliminarily confirmed using CT. Typically, total brain irradiation is performed at a dose of 2500-50 Gy for 2-4 weeks.
The response to radiation therapy depends on the histological structure of the tumor. Metastases from breast or lung cancer usually respond better to treatment than metastases from melanoma or sarcoma. The condition of patients is usually severe, and 20-30% of them die within the first month after radiation therapy or even before its completion. However, most patients who are able to complete the full course of radiation experience some improvement. The 6-month survival rate in this group reaches 30%, and 10% of patients survive up to 1 year. Death usually occurs as a result of extensive metastasis rather than due to brain damage. If a relapse occurs after a standard course of radiation therapy, repeated courses are usually ineffective.
e. Stereotactic radiation surgery using a proton beam or gamma knife can be used for the initial treatment of small metastases, as an adjunct to total brain irradiation, and also for the treatment of relapses. This method involves irradiating a very limited volume of brain tissue at a single, high dose. Such irradiation is usually well tolerated due to the fact that the volume of irradiated tissue is small and the dose quickly decreases with distance from the “target”, which avoids radiation necrosis of healthy areas of the brain. The indications, complications and benefits of this method have not yet been determined.
and. Chemotherapy (methotrexate, fluorouracil, chlormethine, vincristine or cyclophosphamide) is ineffective. Often, during chemotherapy, metastases in the lungs and liver decrease, but in the brain they continue to grow. This may be due to the fact that many of these drugs are unable to cross the blood-brain barrier. On the other hand, nitrosourea derivatives (carmustine and lomustine) can penetrate the CSF at therapeutic concentrations, but intracerebral metastases are rarely sensitive to these drugs.
2. Diffuse tumor infiltration of the meninges
A. Prevalence. Diffuse tumor infiltration of the meninges, previously considered a rare disease, is actually quite common. Most often it develops in non-Hodgkin lymphomas, small cell lung cancer, breast cancer, melanoma, gastrointestinal tumors and acute leukemia. Damage to the meninges occurs so often in acute lymphoblastic leukemia and blast forms of lymphomas that mandatory prevention of neuroleukemia is carried out for these diseases.
b. Clinical picture. Neurological manifestations include symptoms caused by damage to cranial or spinal nerves (for example, radicular pain and paresis, weakness of facial muscles, oculomotor disorders) and general cerebral symptoms (headache, mental disorders). This clinical picture differs significantly from the manifestations of intracerebral metastases, which are more characterized by symptoms of damage to the pathways (for example, hemiparesis or hemianopsia). About a third of patients with diffuse tumor infiltration of the meninges also have intracerebral metastases.
V. Diagnostics
1) The diagnosis of diffuse tumor infiltration of the meninges is confirmed by detecting tumor cells in the CSF. In some patients, such cells are detected only during repeated cytological examinations of the CSF. In purely intracerebral metastases, there are no tumor cells in the CSF, so the detection of these cells clearly indicates involvement of the meninges.
2) With diffuse tumor infiltration of the meninges, the CSF often has increased protein content and decreased glucose content, but these changes are nonspecific. Moderate cytosis and protein-cell dissociation are possible.
3) With CT and MRI, the accumulation of contrast in the subarachnoid cisterns of the base of the brain is of diagnostic significance. However, in most patients these methods either do not detect changes or detect only mild hydrocephalus. MRI of the lumbar region with gadolinium or myelography may reveal tumor nodules on the roots of the cauda equina.
4) Early diagnosis of diffuse tumor infiltration of the meninges requires high alertness and cytological studies of the CSF, including repeated ones.
d. Treatment. Due to diffuse damage to the meninges, treatment is effective only when affecting the entire central nervous system.
1) Craniospinal irradiation at a dose of 40 Gy to the brain and 30 Gy to the spinal cord can be quite effective. However, in the majority of cancer patients, such powerful radiation leads to severe suppression of hematopoiesis, and in the rest, the possibilities of subsequent chemotherapy are sharply limited. Therefore this type of treatment is not recommended. On the other hand, intrathecal administration of antitumor agents may be effective (unlike other brain tumors), since the meninges themselves are affected.
2) Intrathecal chemotherapy. Currently, local irradiation of lesions (for example, with facial nerve involvement or cauda equina syndrome) is combined with frequent intrathecal administration of methotrexate, cytarabine, thioTEP, or a combination of these. In most cases, especially when there are intracerebral metastases, general irradiation of the brain is also performed. Typically, 12 mg of methotrexate, 50 mg of cytarabine or 10 mg of thioTEF are administered 2 times a week. Methotrexate enters the blood and can cause inflammation of the mucous membranes and suppression of hematopoiesis. These complications can be prevented by taking calcium folinate. The drugs are diluted in solvents that do not contain preservatives, since the latter can cause severe damage to the central nervous system.
Recent pharmacokinetic studies have shown that more frequent administration of smaller doses prolongs the residence of the drug in the CSF, but does not produce excessively high peak concentrations causing toxic effects on the nervous system. When administering 1 mg of methotrexate every 12 hours, the same effect is achieved as when administering 12 mg of the drug 2 times a week, but the total dose and the likelihood of side effects are less.
3) Duration of treatment. Clinical and cytological (according to CSF examination) improvement usually occurs after the first 2-4 injections. Intrathecal chemotherapy is continued until tumor cells disappear from the CSF, after which one or two consolidation doses are administered. Then, for 6-12 months (if a relapse does not occur), maintenance therapy is carried out (1 injection per month).
4) Methods of intrathecal administration. After multiple lumbar punctures, the pressure (due to loss of CSF) often becomes very low, and it is often difficult to determine whether the drug has entered the subarachnoid space. In addition, even after successful endolumbar administration, the drug is unevenly distributed in the CSF. Intraventricular administration through the Ommaya reservoir is certainly more effective because the drug is likely to enter the subarachnoid space, is distributed more evenly in the CSF, and repeated lumbar punctures are not necessary to inject the drug or obtain CSF samples. However, in inexperienced hands, the use of the Ommaya reservoir is fraught with serious complications (eg, infection, displacement of the ventricular cannula).
A study of liquorodynamics using diethylenetriaminepentaacetic acid labeled with 111In through the Ommaya reservoir allows us to identify a violation of the outflow of CSF from the ventricular system, at the level of the spinal canal or on the convexital surface of the hemispheres.
5) Method of intraventricular administration of drugs through the Ommaya reservoir
a) The patient is placed in the Trendelenburg position with a slight angle of inclination of the table. In this case, the outflow of CSF when taking a sample under the influence of gravity improves.
b) At the location of the reservoir, the hair is shaved off, the skin is carefully treated and covered with napkins to ensure sterility.
c) To reliably close the puncture hole, the reservoir is pierced at an angle to the surface with a thin (23 or 25 G) needle. Local anesthesia is not used.
d) Collect CSF flowing due to gravity. The cell content in the sample is determined and cytological and bacteriological studies are carried out.
e) Carefully, maintaining sterility, attach the syringe with the drug. The injection is performed slowly (over several minutes). The volume of fluid injected should be less than the volume of CSF withdrawn.
f) Reservoir capacity - 1.4 ml; it should be flushed with 2-3 ml of CSF or preservative-free saline.
g) With proper use, the Ommaya reservoir can be punctured over 100 times without fear of CSF leakage. The procedure is relatively painless, although transient dizziness, headache, and nausea are possible. If local soreness, fever, meningismus, or persistent headache appear, it is necessary to exclude infection of the system.
6) The main side effect of intraventricular chemotherapy is neurotoxic; its likelihood increases when chemotherapy is combined with general brain irradiation. Many patients develop leukoencephalopathy with dementia over the next year.
7) Forecast. Early intensive treatment leads to significant clinical improvement and increased life expectancy in diffuse tumor infiltration of the meninges caused by breast cancer (in approximately 50% of cases), as well as leukemia and lymphoma (in more than 80% of cases). For lung cancer and melanoma, treatment is ineffective. Intrathecal chemotherapy and radiation therapy are accompanied by severe complications, so they are indicated only in situations where the general condition of the patient and the unfavorable prognosis of the disease require active therapy. Without treatment or if it is ineffective, the disease progresses steadily and leads to death within a few weeks from the onset of neurological disorders.
V. CNS TUMORS IN CHILDREN
Malignant neoplasms are the second leading cause of death in children aged 1 to 15 years, and central nervous system tumors are the second most common among other childhood cancers. Most often, brain tumors in children are found in the posterior cranial fossa and in the area of the sella turcica. Early diagnosis of tumors of this localization can be difficult, since their focal symptoms appear late.
A. Cerebellar astrocytoma
1. Prevalence. Cerebellar astrocytoma is the most common brain tumor in children. It is characterized by slow growth and a favorable prognosis.
2. Clinical picture. Cerebellar astrocytoma usually occurs in children aged 5-10 years. In young children, the only signs may be irritability, repeated vomiting, and an enlarged head (due to noncommunicating hydrocephalus). More often, symptoms of damage to the cerebellar hemispheres (impaired coordination of movements and ataxia) appear first.
3. Surgical treatment. Astrocytomas are usually located in the cerebellar hemispheres, much less often in the vermis. In at least half of the cases, the tumors have a cyst-like structure, sometimes with the entire tumor mass contained within a relatively small parietal nodule. Removal of such a nodule leads to a complete cure.
4. Relapses. After tumor removal, relapses are rare, even after decades. Thus, successful removal of cerebellar astrocytoma often leads to recovery, but observation (including CT and MRI) is nevertheless necessary for timely diagnosis of recurrence. In case of relapse, repeat surgery is performed followed by radiation therapy.
5. Radiation therapy. In some cases, cerebellar astrocytomas grow so slowly that even with partial resection of the tumor, its further growth does not occur, and patients live a long time. More often, however, after partial resection, tumor growth resumes, which can lead to death. According to some data, if repeated surgery is not possible, radiation therapy increases life expectancy.
B. Medulloblastoma
1. Prevalence. Medulloblastoma ranks second in frequency among brain tumors in children. It occurs predominantly between the ages of 2 and 10 years, but in approximately 30% of cases it occurs in adolescence and young adulthood.
2. Clinical picture. Medulloblastoma develops from embryonic neuroectodermal cells of the cerebellum. Most often it is located in the midline, involving the cerebellar vermis and fourth ventricle, and the initial manifestations are caused by non-communicating hydrocephalus and increased ICP. However, in children over 6 years of age, medulloblastoma is often localized in the cerebellar hemispheres, resulting in cerebellar disorders (abasia, astasia, ataxia).
3. Growth and metastasis. Medulloblastoma, developing from the cerebellar vermis, often occludes the cavity of the fourth ventricle and infiltrates the brain stem. The tumor may also spread over the surface of the cerebellum in the form of plaques. In 25% of cases, by the time of detection, infiltration of the meninges and metastatic spread of medulloblastoma along the cerebrospinal fluid pathways (in the spinal cord, in the base or hemispheres of the brain) are detected.
4. Surgical treatment. Due to its unfavorable location, invasive growth and tendency to metastasize, it is usually impossible to completely remove the tumor. Nevertheless, the operation is performed on all patients in order to establish an accurate histological diagnosis, remove tumor tissue as much as possible and restore the patency of the liquor-conducting tract. Sometimes bypass surgery is necessary.
5. Radiation therapy. Unlike most other brain tumors, medulloblastoma is very sensitive to radiation. Due to the tendency of medulloblastoma to metastasize along the CSF pathways, craniospinal irradiation is performed. Recently, the maximum tolerated doses of radiation have been used: 50-60 Gy to the tumor area and 36 Gy to the brain and spinal cord. In children under 3 years of age, doses are lower.
6. Forecast. For localized lesions, a 5-year disease-free period after extensive tumor resection and craniospinal irradiation is observed in 60% of patients. It is believed that in most of these cases a complete cure has been achieved. More than 80% of patients who live long after treatment lead a normal life and do not have severe neurological disorders. If there is tumor dissemination, then the 5-year survival rate after craniospinal irradiation is less than 40%.
7. Chemotherapy. Due to its rapid growth and other biological characteristics, medulloblastoma is sensitive to chemotherapy. Combining radiation with chemotherapy such as vincristine, lomustine, cyclophosphamide, procarbazine, chlormethine, or cisplatin can significantly improve the prognosis of patients with disseminated disease. Collaborative studies are being conducted to develop indications and optimal chemotherapy regimens, in particular in patients with tumor recurrence.
8. Intellectual impairment after craniospinal irradiation can be quite pronounced, especially in young children. Adjuvant chemotherapy can reduce the radiation dose, thereby reducing the risk of this complication.
B. Ependymoma
1. General information. Ependymomas (tumors of ependymal cells) are common in childhood. About 70% of ependymomas in children develop in the fourth ventricle, 20% in the lateral ventricles, and 10% in the cauda equina region. The average age of tumor onset in these areas is 2, 6 and 13 years, respectively. In adults, ependymomas are sometimes also found, usually in the spinal cord and lateral ventricles. Most ependymomas are histologically benign. Malignant ependymoma, or ependymoblastoma, is rare.
2. Surgical treatment. Resection of the tumor to the maximum extent possible is necessary. Unfortunately, ependymomas of the fourth ventricle often grow into the base of the medulla oblongata, making their complete removal impossible. Often, by the time of diagnosis, ventricular obstruction and hydrocephalus are present, requiring shunting.
3. Radiation therapy. Ependymomas in almost all cases recur after surgery, regardless of their location or the extent of resection. Postoperative radiation therapy (45-60 Gy over 4-6 weeks) significantly increases life expectancy.
4. Forecast. 5-10 years after extensive resection and radiation therapy, 70% of patients with benign ependymoma survive. The prognosis is less favorable after partial resection; in this situation, the 5-year survival rate is 30-40%.
5. Metastasis. Like medulloblastomas, malignant ependymomas metastasize along the CSF pathways. Therefore, to reduce the likelihood of tumor dissemination throughout the central nervous system and improve the prognosis, craniospinal irradiation is used. With histologically benign tumors, the risk of metastasis is low, so irradiation of the tumor bed is sufficient. The quality of life after successful treatment is usually satisfactory, and therefore early diagnosis and active therapy are necessary. Cooperative studies of the effectiveness of pre- and post-radiation chemotherapy are being conducted.
G. Brainstem gliomas
1. Prevalence. Brainstem gliomas most often occur before the age of 10 years. They account for approximately 15% of all childhood brain tumors.
2. Diagnostics. The favorite location for brainstem gliomas is the pons. Characterized by a gradual increase in signs of damage to the cranial nerves (especially VI, VII, IX and X), ataxia, hemiparesis and headache. High-resolution CT and MRI are often helpful in diagnosing a tumor.
3. Surgical treatment. Because the tumor is located inside the brainstem, it is not accessible to surgery and therefore a biopsy is not performed in most cases. Diagnosis is based mainly on the clinical picture and CT and MRI data.
4. Radiation therapy. Brainstem irradiation (40-60 Gy over 4-6 weeks) causes significant clinical improvement in 70% of patients with suspected brainstem glioma. A five-year disease-free period is observed in 25-30% of patients. However, it is difficult to interpret these results, since in most cases the diagnosis was not histologically confirmed. It should be taken into account that the natural history of brainstem gliomas varies greatly. Most patients experience a relapse within 18 months after irradiation.
5. Corticosteroids in high doses they alleviate the condition of patients for several weeks or months, but do not prevent death.
D. Craniopharyngioma
1. Prevalence. Craniopharyngioma is a tumor of the epithelium of Rathke's pituitary recess. It occurs in both children and adults, accounting for approximately 3% of all brain tumors.
2. Clinical picture. Clinical manifestations of craniopharyngioma are caused by compression of the optic chiasm and optic tracts, dysfunction of the hypothalamus and pituitary gland, and increased ICP. More than 80% of children and 40% of adults with craniopharyngioma have calcifications within or above the sella turcica.
3. Surgical treatment. From a biological and histological point of view, craniopharyngioma is a benign tumor, but its location near vital nerve and neuroendocrine centers prevents its complete removal. Sometimes the tumor can still be completely removed using an operating microscope, but inevitable complications and the need for constant hormone replacement therapy make the success of surgical intervention relative. Even in the case of apparent complete removal, 20-30% of patients develop a relapse within several years. In most cases, only partial resection is possible, after which the likelihood of relapse is very high.
4. Radiation therapy. After partial resection, radiation therapy can significantly delay and, in some cases, prevent recurrence. Recent studies have shown that the disease-free period after subtotal resection and irradiation is more than 10 years.
E. Tumors of the pineal region
1. Clinical picture. Tumors of the pineal region usually occur in adolescence or young adulthood. Their clinical manifestations are caused by compression of the tegmentum of the midbrain (Parinaud's syndrome) or obstruction of the Sylvian aqueduct with the development of non-communicating hydrocephalus. Such tumors may also spread forward, causing damage to the hypothalamus, manifested by diabetes insipidus and precocious puberty, and to the visual tract.
2. Histology. Several types of tumors can develop in the pineal region, biologically and histologically different from each other, but causing a similar clinical picture.
A. Dysgerminoma is the most common (more than 50% of cases) tumor of the pineal region. It grows from undifferentiated germ cells of the pineal gland or hypothalamus.
b. Other germ cell tumors, including teratomas and embryonal carcinomas, can arise in this area. With germ cell tumors, the level of alpha-fetoprotein may increase in the CSF, and the beta subunit of hCG in the plasma.
V. In addition, there are tumors developing from the parenchyma of the pineal gland (pineocytoma and pineoblastoma), glial tumors (astrocytoma, ganglioneuroma) and epidermoid cysts.
3. Treatment. When increased ICP is associated with non-communicating hydrocephalus, ventricular bypass is performed first. Radiation therapy is indicated for germ cell tumors because these tumors are highly sensitive to radiation. In any case, surgery is indicated.
4. Metastasis Malignant tumors of the pineal region can metastasize along the cerebrospinal fluid pathways, so treatment depends on the data of a cytological examination of the CSF. If the spinal cord is damaged, craniospinal irradiation is performed. If the tumor recurs after surgery and radiation therapy, chemotherapy is administered, which can alleviate the patient's condition.
Dexamethasone is used for brain tumors as one of the principles of treatment.
If a patient has signs of increased ICP on CT scan, and an intracranial formation with edema is detected, then dexamethasone is prescribed without waiting for the results of a histological examination.
Dexamethasone in brain oncology reduces perifocal edema, this leads to a partial reduction in focal symptoms and a decrease in ICP. In patients with brain tumors, symptoms of intracranial hypertension and focal disorders decrease within two days after dexamethasone therapy. After five days, patients show complete improvement.
But it is prohibited to prescribe it for a long period, as this can lead to complications: facial edema or proximal myopathy. It is recommended to gradually discontinue the drug over the course of a month. However, if the medication is abruptly discontinued, an increase in ICP with characteristic symptoms may be observed. In such cases, it is necessary to increase the dose of the medicine again.
The reaction to drug withdrawal may vary in intensity: in some people it is faster, in others it is slower.

Contraindication for the drug: diabetes, severe hypertension, bleeding ulcer of the digestive tract.
Other treatments
- The use of osmotic agents. To urgently reduce ICP, mannitol is prescribed. The administration of the drug reduces the water content in the brain tissue.
- . Recommended for patients with secondary brain tumors.
Patients who may benefit from radiation therapy include those with radiosensitive tumors and multiple secondary tumor sites and those who benefit from dexamethasone. - Surgical method. This method can be recommended for young patients if they have single metastases and in the absence of signs of an extensive tumor process.
- . To carry out this method, drugs of natural origin, synthetic and semi-synthetic drugs, antibiotics, and antimetabolites are used. This method consists of using one or more drugs according to a regimen.
- Endoscopic intervention. Recommended for pathological diseases after traumatic brain injuries. The method avoids injury to nerves and blood vessels.
Most glioblastoma patients are exposed to dexamethasone because this corticosteroid is the first-line treatment for controlling brain swelling. Many people also take dexamethasone during radiation therapy, and possibly further if significant tumor remains after surgery. Dexamethasone is an analogue of the body's own cortisol, but about 25 times stronger. Dexamethasone has a long list of adverse potential side effects with long-term use, including muscle weakness, bone loss, steroid-induced diabetes, immunosuppression, weight gain, and psychological effects.
New Data Shows Link Between Dexamethasone Use and Shorter Survival Time for Glioblastoma! This evidence must be weighed against the fact that uncontrolled acute cerebral edema can be fatal in itself and that dexamethasone is often required to control it.
However, an attempt should always be made to use dexamethasone at the lowest effective dose and reduce its use once edema is controlled under the guidance of a physician. However, in the Russian Federation, as a rule, the oncologist prescribes dexamethasone for life and in a large dose!
In a retrospective study 622 patients with glioblastoma
, treated at Sloan Kettering Cancer Center, the analysis showed an independent negative association of steroid (dexamethasone) use at the start of radiation therapy with survival.Patients not taking dexamethasone at the start of radiotherapy had a median survival of 20.6 months, whereas patients taking dexamethasone had a median survival of 12.9 months. There were no significant differences in age, gender, duration of symptoms, or temozolomide use between patients who did or did not receive steroids at the start of therapy. Steroid use was significantly more common in patients with lower Karnofsky performance scores, altered mental status, altered neurological function, less extensive surgery, and lower radiation dosage. Accordingly, steroid use was significantly more common in groups with more recursive divisions. However, multivariate regression analysis showed that overall survival was independently associated with the use of steroids at the start of radiotherapy.
A similar negative association with survival outcomes was found in patients in a phase-3 study of temozolomide in 2005 for a cohort of 832 patients with glioblastoma
, registered in the German Glioma network.Progression-free survival and overall survival were lower in patients exposed to steroids.
The relationship betweensteroid use and outcome 573 patients from the EORTC NCIC main study (Gorlia et al., 2008; Stupp et al., 2014). Steroids were a prognostic factor for both disease-free survival and overall survival, and higher doses of steroids were a negative prognostic factor (in patients treated with radiation alone, more so than in patients treated with radiation + temozolomide followed by temozolomide).
The review authors conclude:"Given that controlled clinical trials to address the steroid question in glioblastoma are unlikely to ever be performed, we believe that our retrospective clinical data and corresponding data from animal models provide The strongest evidence is against the traditional, often uncritical use of steroids in patients with brain tumors."
Subsequent studies in mice helped substantiate these retrospective clinical observations. In a PDGFB-based genetically engineered mouse model of glioblastoma, dexamethasone alone had no effect on survival, but pretreatment with dexamethasone 3 days before a single dose of 10 Gy of radiation negatively affected radiation efficacy. This negative effect of dexamethasone on radiation efficacy was even more dramatic when multiple doses of dexamethasone were used. , which were given up to 5 treatments using 2 Gy radiation, which more closely mimics standard radiation therapy for patients with glioblastoma. In contrast, anti-VEGF antibody, which could be considered a mouse surrogate for Avastin, did not affect radiation efficacy.
An in vivo study showed that Dexamethasone may affect radiation , slowing proliferation, resulting in more cells in the more radioresistant G1 phase of the cell cycle and fewer cells in the more radiosensitive G2/M phase. This finding has far-reaching implications for the potential interference of drugs with cytotoxic mechanisms of action on the efficacy of radiotherapy. The authors conclude that anti-VEGF antibodies, most notably bevacizumab (Avastin), may be used as an alternative decongestant during radiation therapy instead of steroids.
Additionally, it can be noted that dexamethasone is an inducerp-glycoprotein (which helps to “squeeze” chemotherapy out of tumor cells) increases blood glucose levels.
To control cerebral edema and try to reduce the dose of dexamethasone (or completely stop it), you can consider taking and.
No more harmful than sites of stasis in the brain.
In principle, there are four main methods of treating cancer metastases in the brain, which are used independently or in which have an extremely adverse effect on the general condition of the body. Dexamethasone... this is basically lifelong with this...
In this situation, nothing is harmful, which improves the patient’s condition.
Do animals have epilepsy? My rat twitches strangely.
Yes, epilepsy does happen, sad as it is, animals suffer more than they live, there are periods of remission for everyone individually
In the treatment of melanoma metastases in the brain, there are several main directions. In patients with cerebral metastases of melanoma, the positive effect of dexamethasone was obtained at a dose of 4-6 mg 4 times a day intramuscularly or intravenously.
Yes, they are the same people
Yes, sometimes. A friend's pug suffered from epilepsy all her life
It happens, take your rat to the vet!
There are a lot of options: heart failure, pulmonary edema, pneumonia, bronchospasm, cerebrovascular accident, stroke.
give an injection of dexamethasone 0.2 ml intramuscularly and an antibiotic (preferably veterinary Baytril).
Dexamethasone is most often used. If brain metastases manifest themselves in any form, treatment must also be started immediately. As with the spinal cord, steroids are used first, followed by surgery...
Go to the rats website. ru read, ask a question and here they will write you all sorts of ****
Incorrect delivery....brain damage, epilepsy. Have you tried giving Philepsin to a rat?
Hello, can you tell me how to cure stage 4 lung cancer with metastases in the head?
Not if there are metastases in the brain
You can’t cure it, but recovery, including a set of measures, gives not even a chance, but an opportunity to recover. These measures include giving up bad habits, lifestyle changes, a strict anti-cancer diet and much more.
Cancer metastases to the brain are the most serious complications in the treatment of cancer and significantly affect the outcome of treatment and the patient’s life expectancy.
If we say, they will immediately give us 2 Nobel prizes.
Brain metastases are treated by neurooncologists and neurosurgeons. The goal of treatment is to maximize the patient’s life and improve his neurological functions and quality of life.
The main types of treatment for brain metastases are:
neurosurgery
radiosurgery
radiation therapy
Chemotherapy plays a very limited role in the treatment of brain metastases, mainly due to the limited ability of most chemotherapy drugs to penetrate into brain tissue.
However, in recent years there have been more and more examples of the successful use of new drugs for the treatment of metastatic brain tumors (Temodal for the treatment of melanoma metastases, Lapatinib for the treatment of breast cancer metastases, etc.). These drugs are mainly used if brain metastases recur after receiving standard treatment.
To alleviate the patient's condition, corticosteroid and anticonvulsant drugs are used. Corticosteroid drugs are prescribed in almost all cases immediately after diagnosis. As a rule, the drug Dexamethasone is used, which has the ability to reduce brain swelling caused by metastases. Dexamethasone improves the patient's condition, but does not significantly affect life expectancy.
Anticonvulsants (for example, Phenytoin or Finlepsin) are prescribed to patients in whom brain metastases are accompanied by the development of epileptic seizures (25 - 46% of all patients with brain metastases). Prophylactic administration of anticonvulsants is not recommended for patients who have not had epileptic seizures.
What should I do if my dog is bitten by a snake? (it is black and fat, most likely a viper)
Hello. Go to the regional center or district center to see a veterinarian.
Cancer of this form most often metastasizes to the soft and bone tissues of the brain. The difficulty of treating metastases in the brain lies in the presence of a primary tumor in another organ.
Take him to the vet.
To the veterinarian
The dog needs to be put down. Active actions accelerate the flow of poison into the blood. The animal should be in the shade.
It is necessary to carefully examine the dog and try to find the bite site. If the dog was bitten by a snake no more than 15 minutes ago, then you need to try to squeeze out as much blood and poison as possible through the wounds. You should not suck out the venom, because if you have ulcers, wounds or caries in your mouth, then you risk receiving a strong dose of snake venom.
Apply a 4 cm wide pressure bandage to the affected area. This will slow down the entry of poison into the blood. Proper application of the bandage (with a finger placed between the skin and the bandage) will stop blood flow in the superficial veins and lymph circulation.
Give your dog plenty of water. To do this, you need to pour milk or water into her mouth. You can administer 100-200 ml of saline solution subcutaneously.
It is advisable to apply ice to the bite area to slow down the blood flow.
Use of antihistamines (suprastin, tavegil, claritin). A small dog (3-10 kg) will need ¼ or ½ tablet, a large dog (15-30 kg) 1-2 tablets.
Taking heart medications such as validol, cordiamine. This will help support the functioning of the heart.
It is better to carry the dog to the car in your arms. During transportation, the animal must be kept in a restrained state. It is recommended to cover with a blanket or a warm blanket, since the body temperature may decrease due to the action of the poison.
After providing first aid, it is recommended to take the dog to a veterinary clinic, where it will receive qualified assistance. The animal will have an internal catheter installed and blood tests will be taken to determine the extent of the damage. Intensive fluid therapy, as well as sympathetic and anti-shock therapy, will be administered immediately. Treatment uses anticoagulants, diuretics, antihistamines, and antibiotics to prevent secondary infection.
Find a doctor, all you can do is an injection of an antihistamine and urgently go to the clinic
I run to the vet (I also live in the village and call the vet from the city)...
my cat was bitten by a viper once, but it was not possible to keep him at home before the vet arrived, he ran away.. came three days later, everything was fine, he survived.. but it was just luck, and you need to run to the vet or call at home...
In 50% of cases, brain metastases are single, in 50% - multiple. Dexamethasone is prescribed as a palliative agent. The average life expectancy of patients with metastases in the central nervous system without treatment does not exceed 3 months, with radiation...
Inject dexamethasone, suprastin, sulfocamphocaine, furosemide, preferably burdock onto the bite, give it something to drink and take it to the doctor. You don't live in the Arctic. Many also travel on call.
That's right, wrap the dog in a blanket and fly to the vet! On the way, stop at the pharmacy, buy suprastin and a syringe, and give the injection right away. How much to inject - call the vet. I had a medium-sized dog, they told me to inject an ampoule of Suprastin.
Remove the collar, the swelling may spread to the neck.
The doctors will do the rest. And you pray.
The snake can also be black, especially near a river, and they love water... Were there any light or yellow spots on the head? If there were, then it’s Already, it’s not poisonous, but it eats anything and naturally doesn’t brush its teeth, so it can cause an infection. So you still need to go to the vet
The temperature has been under 39 for a month, there is no diagnosis...
Oncology?
I took her in a wheelchair to an MRI of the brain, the result. The radiologist who was observing us prescribed depakine and dexamethasone. The therapist brushes me off, saying that metastases in the brain are the end...
Inflammatory process. Go to other doctors. And don't delay.
Didn't they test for infections, antibodies, hormones?
Have you visited any exotic countries? Have you seen an endocrinologist?
The situation looks like prostate cancer with metastases to the spine and liver. Did you consult oncologists?
Take a PET scan
Is the use of dexamethasone in oncology justified? Some doctors recommend the use of dexamezone for cancer patients, others categorically deny this. This treatment is used to combat the disease and improve the quality of life.
Is it painful to die from brain cancer?
Probably yes
With metastases to the brain, especially with metastases of melanoma, swelling around the lesions can persist for a long time, and in the present period after treatment, the swelling is most likely not associated with the radiosurgical treatment...
What did he forget there anyway?
Ask the authorities, only they can tell you about it.
But quickly.
There are only ignoramuses sitting here, look in the wiki, of course it hurts, it’s a tumor, and it puts pressure on the cerebral cortex so it not only hurts, there are also seizures and fainting and painful shocks, so maintain a healthy lifestyle
I don't think so. there are no nerve endings in the brain
Almost any cancerous tumor can metastasize to the brain. Hormonal drugs Dexamethasone, Decadron, and Prednisone are used to treat brain metastases.
This is painful
Wild headaches due to compression by a brain tumor. Poor pain relief even with large doses of narcotic analgesics.
It’s good that everyone knows everything, I have glioblastoma, this is the most terrible brain tumor of all!))
P.s. I don’t think I’m dying, but I was given radiation and chemotherapy, etc. I can tell you everything, at first your head hurts a lot, and everyone thinks that you have arthritis in your neck and there’s not enough blood in your brain, they prescribe all sorts of stimulants! Then it turns out that you shouldn’t drink them and need them for edema and tumors, and the blood stimulants only harmed you, you start drinking dexamethasone and injecting Dexalgin 25, then you go into surgery, where in 6-8 hours they remove a huge tumor of 300 grams, they leave the second one, you go to another city, there they reduce the swelling, again, in order to understand whether the tumor is operable or not, meanwhile everyone wants to know (what stage is it and is it malignant or not??? _)
and you don’t know anything, because they say, only after the operation) then you do rays for three days (then they really also say that they can’t) and they do chemistry, like you’ll be sorry) but this is nonsense, to be honest, I don’t want that to happen to me regretted it when life depended on it, for example.
Karoch:
Rays - nuclear super particle accelerator))
Chemistry is medicine that poisons everyone, but it also poisons the tumor and you are in for a terrible thing.
tablets - restore everything healthy.
gamma knife - directed nuclear particles at one point, very super strong, but only on one tumor, and not on the entire head.
What can lead to Bulimia?
Experiments with diets...
What metastases look like in the head - photo. Symptoms and exact signs, treatment of patients and how long people with this diagnosis live. Secondary malignant tumors in the brain area and other anatomical structures of the head are classified as metastases...
You can't go on strict diets. I almost got caught.
Bulimia is a feeling of excruciating hunger that occurs in the form of attacks, accompanied by severe weakness, sometimes fainting and pain in the epigastric region; observed in some nervous, mental diseases and diseases of the endocrine glands.
The causes of these diseases lie in consciousness, and only in it. Therefore, attempts to solve these problems only with the help of medications are doomed to failure. Once patients are left unattended, they return to their previous lifestyle. There is no way to do this without psychological help. Moreover, as a rule, you have to start by contacting a psychologist. There are explanations for this.
Young girls (namely, they make up the main contingent of those suffering from bulimia and anorexia) are afraid and do not want to see doctors. In addition, they hide their illness in every possible way and refuse to cooperate with doctors. Often doctors learn about the disease only by pathological changes in the body, which lead girls to other specialists. For example, one of the most characteristic manifestations of bulimia is erosion located on the palatal side of the upper front teeth, which are formed as a result of exposure to stomach acids entering the oral cavity during vomiting. Therefore, bulimia is often discovered by dentists. Or when dealing with menstrual irregularities, which indicate a serious hormonal shift, the disease is discovered by a gynecologist. But even when it is popularly explained to girls what pathological eating poses to their life, not their health, they still do not go to the doctors. Why?
The desire to be slim and graceful, the desire to please, to fit in with something or someone, to be like your ideal is SO great that it outweighs even thoughts of death. Even in hospitals, where girls end up after numerous fainting spells, with terrible weight indicators, they manage to deceive the medical staff in order to remain in their previous condition.
Behind such behavior lie very complex psychological motives. Their prerequisites were created not in one or two months, but often over decades. Because the reason for the hunger strike “to follow a certain image” is just the tip of the iceberg. And under the water lies a huge lack of self-confidence, generated by someone or something. Understanding this, removing the negative impact of all these factors - this is the painstaking, rather long, work of a psychologist and psychotherapist.
http://www.psyhealth.ru/article12.php
Bulimia (Greek bulimia, from bus - bull and limos - hunger, synonyms: “wolfish” hunger, kinorexia) is a sharp increase in appetite, usually occurring in the form of an attack and accompanied by a feeling of painful hunger, general weakness, pain in the epigastric region. Bulimia occurs in certain diseases of the central nervous system, endocrine system, and mental disorders. Bulimia often leads to obesity.
Excessive food intake is a disease that requires comprehensive examination. Most often this is the result of hidden depression.
We can talk about bulimia when bouts of gluttony with the absorption of much more food than is typical for an ordinary person to eat, repeated at least twice a week for three months. During an attack, the patient is unable to stop and control the amount and method of eating. Such gluttons suffer from feelings of guilt, hide their attacks from others and often deliberately induce vomiting or give themselves an enema to get rid of the food they have eaten. This very desire to hide a manic attitude towards food from loved ones already indicates bulimia. Often, both before and after bulimia, these people suffer from anorexia - an obsessive desire to eat as little as possible. They starve and exercise frantically.
In Russia, it is believed that this is a stage of one disease, in which anorectic self-restraint in food can easily turn into bulimia, or they coexist. Bulimia occurs due to nervousness. However, a person may be uncontrollably drawn to the refrigerator with some other diseases - deep depression, for example. Both of these diseases occur “from nerves,” but deep depression covers a person completely, causing a feeling of total dissatisfaction with the world and with oneself, which still does not happen with bulimia.
Bulimia mainly affects women. And usually it all starts in adolescence. An approximate portrait of a young bulimic: a girl of 16-18 years old, impulsive, afraid of independence and dreams of it, preoccupied with her physical attractiveness, suffering from frequent family conflicts or an indifferent and dismissive attitude in the family. Such people become gluttons in three cases out of 100. Among adult women, the risk group includes mistresses and unhappy lovers of all stripes.
In men, bulimia nervosa is 10 times less common. Partly because men are less sensitive to fashion. The fact is that this disorder (overeating plus concern about losing weight) is often, and not without reason, associated with the fashion for a slim figure and the desire to make it perfect. Indeed, how can we not get sick when a great many unattainably thin beauties look at us from TV screens and from the pages of glossy magazines!
Treatment of bulimia requires the combined efforts of doctors from different specialties. Individual psychotherapy appears to play an important role; it should be carried out by a specialist who inspires confidence in the patient. Group therapy can also be of equal benefit. Recovery is usually slow. However, patients can be cured.
Bulimia has always been considered a woman's disease. But it turns out that more and more men are suffering from eating disorders. As doctors describe, bulimia usually affects men from 15 to 35 years old who consider their body not attractive enough. To train their muscles, they often engage in bodybuilding. They starve, but their hungry days are often replaced by bouts of gluttony, during which they can eat an immense amount of food, which they then get rid of by vomiting.
These men, as a rule, have an inferiority complex and a great desire to be recognized. This illness is a reflection of the fact that the soul desires love. Bulimia is very dangerous. Due to frequent vomiting, the body loses a lot of fluid, the balance of fluid in the body is disturbed, due to the loss of water and minerals, convulsions and dysfunction of the heart, stomach, and kidneys are possible.
DIETS!! ! Damn them! Only after these DIETS, compiled by idiots or taken from the Internet from nowhere, do you get bulimia, anorexia and all sorts of schizophrenia... Nothing causes it anymore. What, already?..
Diet addiction or severe nervous breakdown
These drugs are mainly used if brain metastases recur after receiving standard treatment. Dexamethasone improves the patient's condition, but does not significantly affect life expectancy.
Anorexia)
most often occurs in adolescence, occurs as a consequence of a depressive state characteristic of this age, hypertrophied body dysmorphophobia (not liking one’s body)
A person cannot stop losing weight... he wants to be even “slimmer”.
Anorexia nervosa is a diagnosis; treatment requires psychiatric and psychological support along with medication.
Possible death.
There is also atypical anorexia... but it is a sign of other mental illnesses (for example, schizotypal diseases)
Question for neurosurgeons: what do you see in these pictures?
I won't say anything. You need to look at the person; it is useless to do dexamethasone on film.
Brain metastases are diagnosed 5 times more often than brain tumors. Most metastases penetrate the brain through the bloodstream. Treatment of metastases in the brain is carried out by neurooncologists and neurosurgeons.
Hello! Help me please! Dad has lung cancer. Stage 4. Metastases in the brain..
Who knows. My mother also had the same metastases in the brain. Through treatment, this was accelerated by the doctors themselves, who said that there was no need to follow all their instructions, and she could still live. And she died 6 months after their treatment. I came to the hospital on my feet and left on a gurney.
Brain metastases are a very serious complication that, if not properly treated, can cause death. Malignant tumors themselves are considered very dangerous and unpredictable formations in the human body.
Sorry. Sincerely. Only at this stage is it unlikely that anything will help. Radiotherapy?
Dexamethasone will not speed things up.
In order for a patient to survive cancer, a completely different worldview is needed. And so continue to treat, everyone treats like this
At stage 4 you can only prepare for leaving...
What are the signs that a rat is dying?
Doesn't move and stinks
Brain metastases and their treatment without surgical removal. Corticosteroids such as dexamethasone to reduce brain metastases.
Frequent sneezing is one of the most common symptoms
diseases. Lethargy, lack of appetite, dull or ruffled fur,
loud or wheezing breathing and shortness of breath are all signs of respiratory distress
infection, and an immediate visit to the veterinarian would be a very good idea.
Red discharge (porphryin) around the eyes and nose is sometimes a sign
illness, but can also appear due to stress or irritants,
type of dust. Hardenian (? - Hardenian) gland, which is located behind the eye
rat apple, secretes a red, porphyrin-rich secretion that lubricates
eyes and eyelids. This secretion sometimes looks like blood, but contains little or no
does not contain real blood.
Head tilt, often called torticollis, is usually caused by infection
inner ear. The rat must be examined by a veterinarian to determine
whether the eardrum is damaged and make a decision on the course
treatment. If the cause is an infection, the rat is prescribed a course of antibiotics,
but ear drops may also be prescribed, which contain the required
antibiotic, and anti-inflammatory drugs. Another possible
the cause is a pituitary tumor, which is most often observed in the elderly
females, but can also be seen in young females and even males.
There is no treatment for this disease; however, anti-inflammatory
medications such as Prednisone or Dexamethasone may slightly reduce the size
tumors and slightly prolong the life of the rat. Stroke may be another cause.
Again, it is more common in older rats, but is not impossible in older rats.
young rat. Anti-inflammatory drugs can help, but only after
After some time it will be possible to determine that the problem has been resolved. In many
In some cases, complete recovery from a stroke may occur within a short period of time
time (from several days to a week).
Hello. There was an emergency at home, a 3-4 month old kitten was hit on the nose by a door
No, but it’s better to persistently ask for the kitten to be cured
Algorithm for the treatment of patients with multiple metastases in the brain. When administering dexamethasone, weekly assessment of blood sugar levels with insulin correction is very important when blood glucose rises above normal.
Could there be a tumor or hematoma?
When you touch the nose, does it hurt the kitten? Or maybe it’s not because of the door at all... like a chronic runny nose, etc...
Change doctor
He may have a concussion or any other injury.
It is necessary to carry out anti-shock therapy, normalize blood pressure and temperature (most likely these indicators in your kitten are reduced).
This can only be done in a clinic; look for a more qualified doctor. Until this point, try to warm the kitten at home (heating pads, blanket, etc.).
Also, countercurrent agents are needed (Dexamethasone 1 mg (0.5 ml) IM), and also Cordiamine 0.1-0.2 ml s.c.
The temperature is measured rectally; normally in kittens it should be 38.7-39.3 C.
It is necessary to diagnose correctly, an X-ray or CT scan should be done, perhaps the cartilage is not positioned correctly, you cannot pull, you need a qualified doctor, and not one who will simply prescribe injections and medicine.
Mom has a brain tumor, astrocytoma
Was there chemotherapy, were there hormones?
Metastases in the brain have a probable life expectancy. A number of tumors have a tendency to spread their cells to the brain, which significantly affects life expectancy and the survival rate in the treatment of the main cancer...
Only a doctor can help you here
Well, from dexamethasone she swells and gets better, what kind of strange treatment is this?
Sorry...
My husband had an astrocytoma. 9 years ago. They couldn't help then. He lived 9 months after the operation. Now a lot of time has passed, maybe the doctors have come up with a treatment. The program “Live Healthy” not so long ago talked about the treatment of tumors. brain using a device (the tumor is removed in a targeted manner without trepanation). Maybe they will help you, you have to hope and fight.
If possible, consider reviewing the histological slides; for this you can contact UNIM (oncomorphology. RF). With tumors of the central nervous system, diagnostic errors often occur, and therefore treatment may not help.
For metastases in the brain, in most cases, radiation therapy is performed - total irradiation of the brain with metastases or stereotactic targeted irradiation. In these cases, symptomatic treatment is carried out using dexamethasone and diuretics.
Can intracranial pressure be cured?
Why treat it? It’s either there, or it’s not, or it’s normal.
in general, his deviations are treated
Risk groups for brain metastases. Although any cancer can metastasize to the brain, certain tumors are more likely to metastasize to the brain than others.
Intracranial hypertension (ICH) (ancient Greek ὑπερ- - super- + lat. tensio - tension) - increased pressure in the cranial cavity. May be caused by brain pathology (traumatic brain injury, tumors, intracranial hemorrhage, encephalomeningitis, etc.). It occurs as a result of an increase in the volume of intracranial contents: cerebrospinal fluid (CSF), tissue fluid (cerebral edema), blood (venous stagnation) or the appearance of foreign tissue (for example, with a brain tumor).
Treatment of intracranial hypertension should be approached with caution until its cause is determined. The cause of hypertension determines the doctor’s tactics. To quickly reduce intracranial pressure, osmotic diuretics are used (for example, mannitol 0.25-1 g/kg IV drip over 10-15 minutes, if necessary, again every 6 hours for 1-2 days with gradual withdrawal over 2 -4 days) and loop diuretics (furosemide 20-40 mg IV or IM 3 times a day). Corticosteroids (dexamethasone 8-12 mg IV, then 4 mg IV or IM 3-4 times a day) are indicated mainly for brain tumors, but are ineffective for traumatic brain injury or strokes. Their effect manifests itself no earlier than 12 hours later. In critical situations, when there is a threat of herniation in the intensive care unit, they resort to artificial ventilation of the lungs in the hyperventilation mode, the use of barbiturates, and ventricular puncture. The acid-base state should be monitored and the administration of solutions containing large amounts of free liquid (for example, 5% glucose solution) should be avoided. .
You need to drill a hole.
The main reason for this phenomenon (oddly enough) is a spasm of the internal lobes of the liver, which disrupts normal blood filtration.
By eliminating the cause (liver spasm), a cure can be achieved.
If you treat the consequence - ICP - you can turn this disease into a chronic form.
And yet (oddly enough), spasm of the internal lobules of the liver is relieved not by medicine, but
spice (seasoning) Nutmeg (ground or crushed).
Take on an empty stomach, on the tip of a knife, with 1/4 glass of hot water.
It is possible to lower intracranial pressure.
I’m dying of pain, help (Endocrinologists, Neuropathologists)
Lord Jesus the hell knows, go to church if the doctors don’t help
Cyberknife metastases to the brain. Metastasis is the spread of the primary tumor to other organs and tissues. In most cases, however, treatment with high doses of corticosteroids dexamethasone and others can help avoid surgery.
Cancer is not always the correct diagnosis, as a doctor friend of mine said, such a diagnosis is often made when they cannot find the cause. What you describe is more like a violation of energy exchange, I won’t go into details, but if these are not metastases, then you either need a strong energy therapist (who sees the flows), or there is an independent path - together with throwing off the rings (that’s how they are visible), plus through pain (in reasonable) movements, this is a long way, but it works in many cases. There is a computer at hand, see the *curse* reset, although it looks different, it works according to many people’s assurances. If they ask you for money for this, then the wrong person. The statement that desire breaks all obstacles is true, and the release is carried out through the head and gradually. Try to play with the word *faith* for yourself without religious connotations, there is a key to many things
Listen... if there is even one clinic in your city, there is a head doctor. Contact him directly... he must react. There is a Department of Health above him... This is all, of course, going through the authorities... let your relatives help
Try Lasix as a diuretic, and Acupan as a pain reliever, if that doesn’t help, then Nalbuphine. A neurologist prescribed it to me for severe neuropathic pain. Helps. But you need to look for the cause, not eliminate the symptoms. You definitely need to see a doctor, let him give you a referral to some institute in another city for examination. Let your friends help with the car. Don't sit back and good luck.
Lasix is often not allowed, it removes trace elements. Indapamide is possible. The painkiller is Ketanov, but under the cover of Omeprazole, otherwise it’s not far from a stomach ulcer. Have you taken Dexamethasone? or do you accept?
What is dexamethasone in ampoules prescribed for and what to take it with.
Now she is undergoing symptomatic treatment with dexamethasone, Manitol 20% drips, chemotherapy. What caused this? The chemotherapist said that this happens with metastases to the brain, but I am confused by the fact that it started very abruptly. Can...
It is a hormone and anti-inflammatory. well, it relieves swelling, etc.
It is administered during an attack of bronchial asthma.
with an allergic reaction such as Quincke's edema, urticaria, and in general with allergic shock
administered for drowning, suffocation, lightning strike, electric shock, any shock, head injury
Depending on the disease, other drugs are injected. And the dex itself is never taken to physical health. solution and do not mix with other drugs. Injected in its pure form - intravenously or intramuscularly.
Dexamethasone is a synthetic glucocorticosteroid drug (GCS) containing fluoride and having a wide range of actions characteristic of all GCS. It has anti-inflammatory, anti-allergic, anti-shock and anti-toxic effects, suppresses the immune system. . It is used in acute periods for various diseases: cancer, pulmonary, allergic reactions, etc. It is often used together with other drugs strictly as prescribed by the doctor!
What do you mean "what to do with it"??? The doctor prescribed it and will tell you.
Glucocorticosteroid hormone.
Application of the substance Dexamethasone For systemic use (parenteral and orally)
Shock (burn, anaphylactic,
post-traumatic, postoperative, toxic, cardiogenic,
blood transfusion, etc.); cerebral edema (including with tumors,
traumatic brain injury, neurosurgical intervention, hemorrhage
to the brain, encephalitis, meningitis, radiation injury); bronchial asthma,
status asthmaticus; systemic connective tissue diseases (incl.
systemic lupus erythematosus, rheumatoid arthritis, scleroderma,
periarteritis nodosa, dermatomyositis); thyrotoxic crisis;
hepatic coma; poisoning with cauterizing liquids (in order to reduce
inflammatory phenomena and prevention of cicatricial contractions); spicy and
chronic inflammatory diseases of the joints, including gouty and
psoriatic arthritis, osteoarthritis (including post-traumatic),
polyarthritis, glenohumeral periarthritis, ankylosing spondylitis
(Bechterew's disease), juvenile arthritis, Still's syndrome in adults,
bursitis, nonspecific tenosynovitis, synovitis, epicondylitis;
rheumatic fever, acute rheumatic carditis; acute and chronic
allergic diseases: allergic reactions to drugs and food
products, serum sickness, urticaria, allergic rhinitis,
hay fever, angioedema, drug exanthema; diseases
skin: pemphigus, psoriasis, dermatitis (contact dermatitis with lesions
large skin surface, atopic, exfoliative, bullous
herpetiformis, seborrheic, etc.), eczema, toxicoderma, toxic
epidermal necrolysis (Lyell's syndrome), malignant exudative
erythema (Stevens-Johnson syndrome); allergic eye diseases:
allergic corneal ulcers, allergic forms of conjunctivitis;
inflammatory eye diseases: sympathetic ophthalmia, severe
sluggish anterior and posterior uveitis, optic neuritis;
primary or secondary adrenal insufficiency (incl.
condition after removal of the adrenal glands); congenital hyperplasia
adrenal glands; kidney diseases of autoimmune origin (including acute
glomerulonephritis), nephrotic syndrome; subacute thyroiditis;
diseases of the hematopoietic organs: agranulocytosis, panmyelopathy, anemia
(including autoimmune hemolytic, congenital hypoplastic,
erythroblastopenia), idiopathic thrombocytopenic purpura,
secondary thrombocytopenia in adults, lymphoma (Hodgkin,
non-Hodgkin's), leukemia, lymphocytic leukemia (acute, chronic); diseases
lungs: acute alveolitis, pulmonary fibrosis, sarcoidosis II–III stage. ;
tuberculous meningitis, pulmonary tuberculosis, aspiration pneumonia
(only in combination with specific therapy); berylliosis, syndrome
Loefflera (resistant to other therapy); lung cancer (in combination with
cytostatics); multiple sclerosis ; gastrointestinal diseases (to remove
critically ill patient): ulcerative colitis, Crohn's disease,
local enteritis; hepatitis; prevention of rejection reaction
transplant; tumor hypercalcemia, nausea and vomiting with
carrying out cytostatic therapy; multiple myeloma; carrying out a test
in the differential diagnosis of hyperplasia (hyperfunction) and tumors
adrenal cortex.
Dexamethasone instructions for use, reviews, analogs and release forms (tablets 0.5 mg, injections in ampoules (solution for injection), eye drops oftan) drugs for the treatment of inflammation in adults, children and pregnancy.
Compound
- Active substance - dexamethasone sodium phosphate (in terms of dexamethasone phosphate) - 4.0 mg/8.0 mg;
- Excipients - glycerin, disodium phosphate dihydrate, disodium edetate, water for injection.
Release forms
- Tablets 0.5 mg;
- Solution in ampoules for intravenous and intramuscular administration (injections for injections) 4 mg/ml;
- Oftan eye drops 0.1%;
- Ophthalmic suspension 0.1%
DEXAMETHASONE instructions for use of the drug
Oral administration of Dexamethasone in the form of tablets involves the administration of 10-15 mg of the drug per day at the initial stage of treatment, followed by a reduction in the daily dose to 2-4.5 mg during maintenance therapy. The instructions recommend dividing the daily dose of Dexamethasone into 2-3 doses (after or during meals).
DEXAMETHASONE injections in ampoules, eye drops, tablets - instructions for use
Maintenance small doses should be taken once a day, preferably in the morning. Dexamethasone in ampoules is intended for intravenous (drip or stream), intramuscular, perarticular and intra-articular administration. The recommended daily dose of Dexamethasone for these routes of administration is 4-20 mg. Dexamethasone in ampoules is usually used 3-4 times a day for 3-4 days, followed by switching to tablets.
Dexamethasone drops are used in ophthalmology: in acute conditions, 1-2 drops of the drug are instilled into the conjunctival sac every 1-2 hours, when the condition improves - every 4-6 hours. Chronic processes require the use of Dexamethasone drops 2 times a day.
The duration of treatment depends on the clinical course of the disease, so Dexamethasone drops can be used from several days to four weeks.
Indications for use of Dexamethasone
Diseases requiring the administration of fast-acting corticosteroids, as well as cases when oral administration of the drug is impossible:
- Shock (burn, traumatic, surgical, toxic) - when vasoconstrictors, plasma replacement drugs and other symptomatic therapy are ineffective;
- Severe allergic reactions, anaphylactic shock;
- Blood diseases: acute hemolytic anemia, agranulocytosis, idiopathic thrombocytopenic purpura in adults;
- Endocrine diseases: acute adrenal insufficiency, primary or secondary adrenal insufficiency, congenital adrenal hyperplasia, subacute thyroiditis;
- Local application (in the area of pathological formation): keloids, discoid lupus erythematosus, granuloma annulare;
- Rheumatic diseases - Dexamethasone instructions for use;
- In ophthalmological practice (subconjunctival, retrobulbar or parabulbar administration): allergic conjunctivitis, keratitis, keratoconjunctivitis without damage to the epithelium, iritis, iridocyclitis, blepharitis, blepharoconjunctivitis, scleritis, episcleritis, inflammatory process after eye injuries and surgical interventions, sympathetic ophthalmia, immunosuppressive treatment after transplantation corneas;
- Acute severe dermatoses;
- Malignant diseases: palliative treatment of leukemia and lymphoma in adult patients; acute leukemia in children; hypercalcemia in patients suffering from malignant tumors when oral treatment is not possible;
- Severe infectious diseases (in combination with antibiotics);
- Brain edema (with a brain tumor, traumatic brain injury, neurosurgical intervention, cerebral hemorrhage, encephalitis, meningitis, radiation injury);
- Systemic connective tissue diseases;
- Asthmatic status; severe bronchospasm (exacerbation of bronchial asthma, chronic obstructive bronchitis).
Why are Dexamethasone tablets prescribed?
Dexamethasone - tablets
- For hypothyroidism (a condition caused by a persistent lack of thyroid hormones);
- With rheumatoid arthritis in the acute phase;
- With congenital adrenogenital syndrome (hyperfunction of the adrenal cortex and increased levels of androgens in the body);
- With Addison-Beermer disease (loss of the adrenal glands' ability to produce hormones in sufficient quantities);
- For pemphigus (a skin disease manifested in the form of blisters on the hands, genitals, mouth, etc.);
- For acute and subacute thyroiditis (inflammation of the thyroid gland);
- For acute erythroderma (redness of the skin);
- With progressive ophthalmopathy (increase in the volume of eye tissue) associated with thyrotoxicosis (intoxication with thyroid hormones);
- For acute eczema;
- For connective tissue diseases;
- For malignant tumors (symptomatic therapy);
- For autoimmune hemolytic anemia;
- With cerebral edema;
- With agranulocytosis (decrease in the level of neutrophils in the blood);
- For bronchial asthma;
- Serum sickness (immune reaction to foreign serum proteins).
Why are Dexamethasone drops prescribed?

Dexamethasone eye drops
- With scleritis (inflammation of the deep layers of the sclera of the eye);
- For keratitis (inflammation of the cornea of the eye);
- With sympathetic ophthalmia (inflammatory lesions of the eye);
- For non-purulent and allergic conjunctivitis (inflammation of the mucous membrane of the eye);
- For iritis (inflammation of the iris);
- For blepharitis (inflammation of the edges of the eyelids);
- In inflammatory processes after eye injuries or operations;
- With iridocyclitis (inflammation of the iris and ciliary body);
- With episcleritis (inflammation of the connective tissue between the conjunctiva and sclera);
- For keratoconjunctivitis (simultaneous inflammation of the conjunctiva and cornea of the eye) without damage to the epithelium.
Why are injections in Dexamethasone ampoules prescribed?

Dexamethasone injections (ampoules)
- For acute hemolytic anemia;
- In case of acute insufficiency of the adrenal cortex;
- For status asthmaticus;
- For acute lymphoblastic leukemia (a malignant disease that affects the bone marrow, spleen, lymph nodes, thymus gland and other organs). Dexamethasone instructions for use;
- With cerebral edema;
- For severe infectious diseases;
- With shock of various origins;
- For joint diseases;
- With thrombocytopenia;
- For severe allergic reactions;
- For acute croup (inflammation of the larynx and upper respiratory tract);
- With agranulicytosis.
Contraindications
For short-term use for health reasons, the only contraindication is hypersensitivity to dexamethasone or the components of the drug.
In children during the growth period, GCS should be used only according to absolute indications and under the particularly careful supervision of the attending physician.
Carefully the drug should be prescribed for the following diseases and conditions:
The therapeutic and toxic effects of Dexamethasone are reduced by barbiturates, phenytoin, rifabutin, carbamazepine, ephedrine and aminoglutethimide, rifampicin (accelerate metabolism); somatotropin; antacids (reduce absorption), enhance - estrogen-containing oral contraceptives. Concomitant use with cyclosporine increases the risk of developing seizures in children.
The risk of arrhythmias and hypokalemia is increased by cardiac glycosides and diuretics, the likelihood of edema and arterial hypertension is increased by sodium-containing drugs and nutritional supplements, severe hypokalemia, heart failure and osteoporosis is increased by amphotericin B and carbonic anhydrase inhibitors; the risk of erosive and ulcerative lesions and bleeding from the gastrointestinal tract - non-steroidal anti-inflammatory drugs. Dexamethasone instructions for use.
When used simultaneously with live antiviral vaccines and against the background of other types of immunization, it increases the risk of viral activation and the development of infection.
Concomitant use with thiazide diuretics, furosemide, ethacrynic acid, carbonic anhydrase inhibitors, amphotericin B can lead to severe hypokalemia, which can enhance the toxic effects of cardiac glycosides and non-depolarizing muscle relaxants.
Weakens the hypoglycemic activity of insulin and oral antidiabetic agents; anticoagulant - coumarins; diuretic – diuretic diuretics; immunotropic – vaccination (suppresses antibody formation).
Worsens the tolerance of cardiac glycosides (causes potassium deficiency), reduces the concentration of salicylates and praziquantel in the blood. It may increase the concentration of glucose in the blood, which requires dose adjustment of hypoglycemic drugs, sulfonylurea derivatives, and asparaginase.
GCS increase the clearance of salicylates, therefore, after discontinuation of Dexamethasone, it is necessary to reduce the dose of salicylates. When used concomitantly with indomethacin, the Dexamethasone suppression test may give false negative results.
Directions for use and doses
Intended for intravenous, intramuscular, intraarticular, periarticular and retrobulbar administration. The dosage regimen is individual and depends on the indications, the patient’s condition and his response to therapy.
To prepare a solution for intravenous drip infusion, you should use an isotonic sodium chloride solution or a 5% dextrose solution. Administration of high doses of dexamethasone can be continued only until the patient's condition has stabilized, which usually does not exceed 48 to 72 hours.
For adults in acute and emergency conditions, it is administered intravenously slowly, in a stream or drip, or intramuscularly at a dose of 4-20 mg 3-4 times a day. The maximum single dose is 80 mg. Maintenance dose – 0.2-9 mg per day. The course of treatment is 3-4 days, then switch to oral administration of Dexamethasone. Children - IM at a dose of 0.02776-0.16665 mg/kg every 12-24 hours.
- Soft tissue: 2 to 6 mg;
- Large joints (eg knee joint): 2 to 4 mg;
- Joint capsules: from 2 to 3 mg;
- Small joints (eg, interphalangeal, temporal joint): from 0.8 to 1 mg;
- Nerve ganglia: 1 to 2 mg;
- Tendons: from 0.4 to 1 mg.
The drug is re-prescribed at intervals from 3 days to 3 weeks as needed; The maximum dose for adults is 80 mg per day. For shock, adults - 20 mg intravenously once, then 3 mg/kg over 24 hours as a continuous infusion or intravenously 2-6 mg/kg once, or iv 40 mg every 2- 6 hours.
For cerebral edema (adults) – 10 mg IV, then 4 mg every 6 hours IM until symptoms disappear; the dose is reduced after 2-4 days and gradually - over 5-7 days - treatment is stopped. For adrenal insufficiency (children), IM 0.0233 mg/kg (0.67/mg/m2) per day in 3 injections every third day, or daily 0.00776-0.01165 mg/kg (0.233 - 0.335 mg/m2) per day.
In case of an acute allergic reaction or exacerbation of a chronic allergic disease, dexamethasone should be prescribed according to the following schedule, taking into account a combination of parenteral and oral administration: dexamethasone instructions for use injection solution 4 mg/ml: 1 day, 1 or 2 ml (4 or 8 mg ) intramuscularly; dexamethasone tablets 0.75 mg: second and third days, 4 tablets in 2 divided doses per day, 4th day, 2 tablets in 2 divided doses, 5th and 6th days, 1 tablet every day, 7th day - without treatment, 8th day - observation.
Side effects
Dexamethasone instructions for use are usually well tolerated. It has low mineralocorticoid activity, i.e. its effect on water-electrolyte metabolism is small. As a rule, low and medium doses of Dexamethasone do not cause sodium and water retention in the body or increased potassium excretion.
The following side effects are described:
- From the senses: posterior subcapsular cataract, increased intraocular pressure with possible damage to the optic nerve, a tendency to develop secondary bacterial, fungal or viral eye infections, trophic changes in the cornea, exophthalmos, sudden loss of vision (with parenteral administration in the head, neck, nasal shells, scalp, possible deposition of drug crystals in the vessels of the eye);
- From the skin and mucous membranes: delayed wound healing, petechiae, ecchymoses, thinning of the skin, hyper- or hypopigmentation, steroid acne, stretch marks, tendency to develop pyoderma and candidiasis;
- From the endocrine system: decreased glucose tolerance, steroid diabetes mellitus or manifestation of latent diabetes mellitus, suppression of adrenal function, Itsenko-Cushing syndrome (moon-shaped face, pituitary-type obesity, hirsutism, increased blood pressure, dysmenorrhea, amenorrhea, muscle weakness, stretch marks) , delayed sexual development in children;
- From the metabolic side: increased excretion of calcium, hypocalcemia, increased body weight, negative nitrogen balance (increased breakdown of proteins), increased sweating. Caused by mineralocorticoid activity - fluid and sodium retention (peripheral edema), hypsarnatremia, hypokalemia syndrome (hypokalemia, arrhythmia, myalgia or muscle spasm, unusual weakness and fatigue);
- From the musculoskeletal system: slower growth and ossification processes in children (premature closure of epiphyseal growth plates), osteoporosis (very rarely - pathological bone fractures, aseptic necrosis of the head of the humerus and femur), rupture of muscle tendons, steroid myopathy, decreased muscle mass (atrophy). Dexamethasone instructions for use;
- From the cardiovascular system: arrhythmias, bradycardia (up to cardiac arrest); development (in predisposed patients) or increased severity of heart failure, changes in the electrocardiogram characteristic of hypokalemia, increased blood pressure, hypercoagulation, thrombosis. In patients with acute and subacute myocardial infarction - the spread of necrosis, slowing down the formation of scar tissue, which can lead to rupture of the heart muscle;
- From the digestive system: nausea, vomiting, pancreatitis, steroid ulcer of the stomach and duodenum, erosive esophagitis, gastrointestinal bleeding and perforation of the wall of the gastrointestinal tract, increased or decreased appetite, indigestion, flatulence, hiccups. In rare cases, increased activity of liver transaminases and alkaline phosphatase;
- From the nervous system: delirium, disorientation, euphoria, hallucinations, manic-depressive psychosis, depression, paranoia, increased intracranial pressure, nervousness or anxiety, insomnia, dizziness, vertigo, pseudotumor of the cerebellum, headache, convulsions.
Allergic reactions: skin rash, itching, anaphylactic shock, local allergic reactions.
Local for parenteral administration: burning, numbness, pain, tingling at the injection site, infection at the injection site, rarely - necrosis of surrounding tissues, scarring at the injection site; atrophy of the skin and subcutaneous tissue with intramuscular injection (injection into the deltoid muscle is especially dangerous).
Others: development or exacerbation of infections (the appearance of this side effect is facilitated by jointly used immunosuppressants and vaccination), leukocyturia, “flushing” of blood to the face, “withdrawal” syndrome.
Price of the drug DEXAMETHASONE
- Dexamethasone, tablets 0.5 mg, 10 pcs. - 45 rub.;
- Dexamethasone, eye drops 0.1%, 5 ml - 34 rubles;
- Dexamethasone, ampoules 4 mg, 1 ml, 25 pcs. - 202 rub.;
- Dexamethasone solution for injection 4 mg/ml 1 ml ampoule, 25 pcs. 144 rub.;
- Dexamethasone eye drops, 10 ml - 82 rub.
special instructions
- It should be used with caution in acute and subacute myocardial infarction - the necrosis focus may spread, the formation of scar tissue may slow down and the heart muscle may rupture;
- During treatment with Dexamethasone, vaccination should not be carried out due to a decrease in its effectiveness (immune response).
When prescribing Dexamethasone for intercurrent infections, septic conditions and tuberculosis, it is necessary to simultaneously treat with bactericidal antibiotics; - In patients with latent infectious diseases of the kidneys and urinary tract, Dexamethasone can cause leukocyturia, which may have diagnostic value;
- With sudden withdrawal, especially in the case of previous use of high doses, the development of withdrawal syndrome (anorexia, nausea, lethargy, generalized musculoskeletal pain, general weakness) is possible, as well as an exacerbation of the disease for which Dexamethasone was prescribed;
- During treatment with Dexamethasone (especially long-term), observation by an ophthalmologist, monitoring of blood pressure and water-electrolyte balance, as well as peripheral blood patterns and blood glucose levels are necessary;
- In children during long-term treatment with Dexamethasone, careful monitoring of the dynamics of growth and development is necessary. Children who during the treatment period were in contact with patients with measles or chickenpox are prescribed specific immunoglobulins prophylactically.
Due to the weak mineralocorticoid effect, Dexamethasone is used in combination with mineralocorticoids for replacement therapy for adrenal insufficiency; - Dexamethasone increases the content of 11- and 17-hydroxyketocorticosteroid metabolites;
- In order to reduce side effects, antacids can be prescribed, and the intake of K+ into the body should be increased (diet, potassium supplements). Food should be rich in proteins, vitamins, with limited fat, carbohydrates and table salt;
- In patients with diabetes mellitus, blood glucose levels should be monitored and therapy adjusted if necessary.
X-ray monitoring of the osteoarticular system is indicated (images of the spine, hand); - The effect of the drug is enhanced in patients with hypothyroidism and liver cirrhosis. The drug may worsen existing emotional instability or psychotic disorders. If a history of psychosis is indicated, Dexamethasone in high doses is prescribed under the strict supervision of a physician;
- In stressful situations during maintenance treatment (for example, surgery, trauma or infectious diseases), the dose of the drug should be adjusted due to an increased need for glucocorticosteroids. Patients should be carefully monitored for a year after the end of long-term therapy with Dexamethasone due to the possible development of relative insufficiency of the adrenal cortex in stressful situations. Dexamethasone instructions for use.
Video review of the drug DEXAMETHASONE
Dosage form: injection Compound:active substance: dexamethasone sodium phosphate 4.37 mg(corresponding to 4.00 mg dexamethasone phosphate):
Excipients : glycerol 22.50 mg, disodium edetate dihydrate 0.10 mg, sodium hydrogen phosphate dihydrate 0.80 mg, water for injection q.s. up to 1.00 ml.
Description: Transparent, colorless or slightly yellowish liquid.
H.02.A.B Glucocorticoids
S.01.B.A Corticosteroids
Pharmacodynamics:Dexamethasone is a synthetic hormone of the adrenal cortex with glucocorticosteroid action (GCS). It has anti-inflammatory and immunosuppressive effects, and also affects energy metabolism, glucose homeostasis and
(via negative feedback) on the secretion of hypothalamic activating factor and adrenocorticotropic hormone from the pituitary gland.GCS are fat-soluble substances and therefore easily penetrate into target cells through cell membranes. The binding of a hormone to a receptor causes conformational changes in the receptor and increases its affinity for DNA. The hormone-receptor complex enters the cell nucleus and binds to the regulatory region of the DNA molecule, also known as the glucocorticoid response element (GRE).
The activated receptor binds to GREs or specific genes and regulates messenger RNA (mRNA) transcription. The newly formed mRNA is transported to ribosomes, which then participate in the formation of new proteins. Depending on the type of target cells and cellular processes, the formation of new proteins can be either enhanced (for example, the synthesis of tyrosine transaminase in liver cells) or suppressed (for example, the synthesis of IL-2 in lymphocytes). Since receptors for GCS are found in all tissues, their action is realized in most cells of the body.
Effect on energy metabolism and glucose homeostasis: , along with insulin, glucagon and catecholamines, regulates the accumulation and expenditure of energy. In the liver, it stimulates the formation of glucose from pyruvate and amino acids and the formation of glycogen. IN peripheral tissues, particularly in muscles, reduces glucose consumption and mobilizes amino acids (from proteins), which are a substrate for gluconeogenesis in the liver. Direct effects on fat metabolism include central redistribution of adipose tissue and increased lipolysis in response to catecholamines.
Through receptors in the proximal tubules of the kidneys, it stimulates renal blood flow and glomerular filtration, suppresses the formation and secretion of vasopressin and improves the ability of the kidneys to excrete acids.
Increases the sensitivity of blood vessels to pressor agents.
In patients who have received long-term dexamethasone therapy and are exposed to stress after its discontinuation, dexamethasone use should be resumed due to the fact that induced adrenal insufficiency may persist for several months after discontinuation of the drug.
Dexamethasone therapy may mask signs of infectious processes and signs of intestinal perforation.
Dexamethasone may aggravate the course of fungal infections, latent amoebiasis or pulmonary tuberculosis. Patients with acute pulmonary tuberculosis can be prescribed (together with anti-tuberculosis drugs) only in the case of a fulminant or severe disseminated process. Patients with inactive pulmonary tuberculosis receiving Dexamethasone therapy or patients with positive tuberculin tests should simultaneously receive therapy with anti-tuberculosis drugs.
Particular attention and careful medical supervision is necessary for patients with osteoporosis, hypertension, heart failure, tuberculosis, glaucoma, liver or kidney failure, diabetes mellitus, active peptic ulcers, fresh intestinal anastomoses, ulcerative colitis and epilepsy. Caution should be used in the first weeks after acute myocardial infarction, as well as in patients with thromboembolism, myasthenia gravis, glaucoma, hypothyroidism, psychosis or psychoneurosis, as well as in elderly patients.
During dexamethasone therapy, decompensation of diabetes mellitus or transition from latent to clinically manifest diabetes mellitus is possible.
With long-term use, monitoring of serum potassium levels is necessary.
Vaccination with live vaccines is contraindicated during dexamethasone therapy.
Immunization with killed viral or bacterial vaccines does not give the expected increase in the titer of specific antibodies and therefore does not have the necessary protective effect. usually not used 8 weeks before vaccination and 2 weeks after vaccination.
Dexamethasone may increase susceptibility to or mask symptoms of infectious diseases. Chickenpox, measles and other infections can be more severe and even fatal in non-immunized individuals. Immunosuppression often develops with long-term use of GCS, but can also occur with short-term treatment.
Patients taking high doses of dexamethasone for a long time should avoid contact with infectious patients; If accidental contact occurs, prophylactic treatment with immunoglobulin is recommended.
Caution should be exercised when treating patients who have recently undergone surgery or bone fractures as it may delay the healing of wounds and fractures.
The effect of glucocorticosteroids is enhanced in patients with liver cirrhosis or hypothyroidism.
Intra-articular use of glucocorticosteroids may be accompanied by local and systemic effects.
Frequent use leads to destruction of articular cartilage and necrosis of bone tissue.
Before intra-articular injection, it is necessary to pump out and examine (for the presence of an infectious process) the synovial fluid from the joint. Injection of corticosteroids into the infected joint should be avoided. If septic inflammation develops in the joint after injection, appropriate antibiotic therapy is necessary. Patients should avoid putting stress on the joint into which the injection was made until the inflammatory process has completely resolved.
Glucocorticosteroids may alter the results of skin allergy tests.
Dexamethasone is used in children and adolescents only under strict indications. During treatment, strict monitoring of the growth and development of the child or adolescent is necessary.
Special information about some components of the drug
The drug contains less than 1 mmol (23 mg) sodium per dose.
Impact on the ability to drive vehicles. Wed and fur.:Dexamethasone does not affect the ability to drive vehicles or operate other technical devices that require increased concentration and speed of psychomotor reactions.
Release form/dosage:Solution for injection, 4 mg/ml.
Package:1 ml in dark glass ampoules (type
I). A colored dot is applied to the ampoule indicating the break line of the ampoule and a color coding ring.5 ampoules per blister made of PVC-aluminum foil.
5 blisters along with instructions for use are placed in a cardboard pack.
Storage conditions:At a temperature not higher than 25 °C.
Keep out of the reach of children.
Best before date:Do not use the drug after the expiration date.
Conditions for dispensing from pharmacies: On prescription Registration number: P N012237/02 Registration date: 28.04.2011 / 14.05.2015 Expiration date: InstructionsGood afternoon
Unfortunately, the information provided is not enough for consultation. Such cases require personal observation of the patient and detailed study of medical records. Formally, interferon and dexamethasone can be prescribed simultaneously (although with caution regarding possible overlapping side effects). You need to understand that interferon and dexamethasone are prescribed for different purposes. Dexamethasone is prescribed to reduce swelling of the brain around the metastasis. It does not have antitumor activity, i.e. It is prescribed to reduce the symptoms caused by the tumor, but does not affect the tumor itself. It makes no sense to replace dexamethasone, because In terms of toxicity/efficacy ratio, it is the most acceptable of the drugs in a similar group. Interferon is prescribed to influence the tumor itself (in order to slow down its progression). To prescribe the drug, certain conditions are necessary (it is not effective in patients with an unfavorable prognosis of the disease), but it is impossible to assess their presence/absence based on the information provided. In some cases, unfortunately, with kidney cancer, a decision is made to refuse antitumor treatment altogether, because it does not increase patient survival compared with simple maintenance therapy.
Sincerely, Zhukov N.V.
Re: Brain metastasis
Date: 03/21/12 15:39
Answered by: Olga Nevostrueva
Hello. Thanks for your reply. I am writing about the disease in more detail. In 2008, the left kidney was removed. In the operation protocol T3NxM0 - stage II. The results of the histological conclusion are G2 renal carcinoma with invasion of the capsule and fiber. In May 2011, a brain metastasis was discovered (accidentally). On June 15, 2011, Gamma Knife treatment was performed at the MIBS Medical Center in St. Petersburg. I took Dexamethosone. He felt satisfactory, his arm and leg functioned normally, he stuttered a little, and the fingers on his left hand functioned a little worse. Ultrasound of internal organs from 06/06/2011. revealed a mass formation in the left lobe of the thyroid gland, a puncture was performed - papillary carcinoma. In July, an operation was performed to remove the left lobe of the thyroid gland. My arm and leg began to work worse after this operation. Last entry in the chart: Bl of the left kidney pT3aN0M0 grade 3 after surgical treatment in 2008. Progression in 2011 Mts of the right parietal lobe. Condition after radiosurgical treatment after 06.2011 Mts in the liver. Bl of the thyroid gland pT1N1aM0 grade 3 after surgical treatment on July 27, 2011.
CT results from 10.27.11: Rv Bl in the bed of the removed kidney with ingrowth into the iliopsoas muscle and descending colon. There is a connection with the tail of the pancreas. Multiple space-occupying lesions (mts) of the liver.
In November 2011, a blood clot formed in my leg and underwent treatment.
Currently he has undergone a course of immunotherapy. They did a CT scan of the abdominal cavity - negative dynamics of Mts. We live in Izhevsk, we don’t have good specialists. My father did not fall into depression, he intends to continue to fight. They did an encephalogram of the brain, everything was fine there. Visits a neurologist. He really wants the use of his arms and legs to be restored. The neurologist prescribed a drug that blocks brain function - Convulex. Attends physical therapy classes. They did not prescribe dexamethosone, since the inflammation around the tumor did not increase, they say that it should go away soon. Now we will ask for the prescription of targeted drugs for the treatment of relapse and metastases of kidney cancer. Tell me, which drug is better to use so as not to harm the brain? After the Gamma Knife procedure, they said that the use of chemotherapy was not advisable; there were cases of unfavorable outcomes, including deaths. Do we have the right to insist on the allocation of a quota for the provision of high-tech medical care in your center? You yourself wrote that it is better to observe in person. So far we have been denied a quota. What should we do? I beg you to answer!!! Thank you in advance.
Re: Brain metastasis
Dear Olga!
I apologize for the long wait for an answer. Alas, the main work takes up almost all of my time. The situation is this: existing drugs for the treatment of kidney cancer do not have a curative potential (i.e. you must understand that it is impossible to cure your father). The purpose of these drugs is to restrain the progression of the tumor and prolong the life of patients. In this regard, when prescribing them, the risks and benefits of treatment are always weighed. Any of the available drugs (sunitinib, pazopanib, bevacizumab + interferon) can potentially be prescribed to the patient - so far they have been found to be equally effective. However, the issue of prescribing drugs lies more in the social than in the medical plane. Without going into medical details, I can only say one thing - unfortunately, the state does not provide drugs for everyone with an approximate cost of 100,000 rubles per month (and which do not cure, but only prolong life). And therefore, the chance of receiving or not receiving such treatment depends mainly on the activity of the patient and/or relatives. The presence of brain metastases (in itself) is not a reason to refuse treatment (there is no such contraindication in the instructions). The refusal to provide drugs must be somehow motivated and based on this motivation it will be possible to judge whether it occurred for a medical or social reason. If according to the second, it makes sense to fight for the provision of drugs, if according to the first, alas, the most suitable method of treatment will be symptomatic therapy (fighting the symptoms, but not the tumor). Regarding “coming for high-tech treatment” - alas, these are drugs for daily use until progression, i.e. for months, sometimes for years. Nothing high-tech is required to take them, so a personal visit is impractical (none of the central clinics will be able to provide you with the drug for treatment for the entire period; you will have to “knock out” these drugs at your place of residence.” Sincerely, Zhukov N.V.
Dexamethasone is used for brain tumors as one of the principles of treatment.
If a patient has signs of increased ICP on CT, and MRI reveals an intracranial formation with edema, then dexamethasone is prescribed without waiting for the results of histological examination.
Dexamethasone in brain oncology reduces perifocal edema, this leads to a partial reduction in focal symptoms and a decrease in ICP. In patients with brain tumors, symptoms of intracranial hypertension and focal disorders decrease within two days after dexamethasone therapy. After five days, patients show complete improvement.
But, it is prohibited to prescribe it for a long term, this can lead to complications: facial edema or proximal myopathy. It is recommended to gradually discontinue the drug over the course of a month. However, if the medication is abruptly discontinued, an increase in ICP with characteristic symptoms may be observed. In such cases, it is necessary to increase the dose of the medicine again.
The reaction to drug withdrawal may vary, with some people responding faster and others slower.

Contraindication for the drug: diabetes, severe hypertension, bleeding ulcer of the digestive tract.
Other treatments
- The use of osmotic agents. To urgently reduce ICP, mannitol is prescribed. The administration of the drug reduces the water content in the brain tissue.
- Radiation therapy. Recommended for patients with secondary brain tumors.
Patients who may benefit from radiation therapy include those with radiosensitive tumors and multiple secondary tumor sites and those who benefit from dexamethasone. - Surgical method. This method can be recommended for young patients if they have single metastases and in the absence of signs of an extensive tumor process.
- Chemotherapy. To carry out this method, drugs of natural origin, synthetic and semi-synthetic drugs, antibiotics, and antimetabolites are used. This method consists of using one or more drugs according to a regimen.
- Endoscopic intervention. Recommended for pathological diseases, after traumatic brain injuries. The method avoids injury to nerves and blood vessels.
In contact with
Classmates