Nuts for cholelithiasis. Diet rules during remission and during exacerbation of cholelithiasis
The discomfort and pain inherent in this disease do not allow a person to live normally, which is why the diet for stones in gallbladder It is considered the safest and gentlest way to get rid of the problem.
The pain mainly forms in the hypochondrium area on the right side. At the same time, it is easy to confuse it with the symptoms of other diseases, because it often extends to the shoulder blade, collarbone and even the heart area.
The pain is especially severe after eating junk food, salty, spicy and fatty. Such unpleasant sensations as bitterness in the mouth, burning, and dryness are no exception. Diet in this case helps reduce such symptoms and promotes recovery. Before we understand in detail all the nuances of such a diet, let’s try to understand what cholelithiasis is and for what reasons it appears.
- frequent consumption of food that contains excess animal fats;
- dysfunction of the liver, in the case when bile production is noticeably reduced;
- the presence of excess body weight, which occurs in most patients;
- reception oral contraceptives over a long period;
- the presence of other serious diseases such as diabetes, allergic reactions, cirrhosis, anemia and much more.
- the presence of such serious diseases as disorders of contractile function, consequences after surgical intervention, high blood pressure in the gastrointestinal tract, etc.;
- presence of low physical activity;
- in some cases, problems may arise during pregnancy, when the outflow of bile is complicated due to the fact that the uterus puts a lot of pressure on the abdominal organs;
- sudden weight loss, poor diet, fasting, long breaks between meals.
- 1. Primary stones. As a rule, they do not cause any discomfort, not to mention the pain. A person can live a long time, perhaps even a whole life, and never know about the presence of formations in the gallbladder. In this case, stones are formed long time in ways that have remained unchanged.
- 2. Secondary formations. Occurs when there is a violation of the outflow of bile. Most often this occurs due to a decrease in the volume of the bile component that enters the duodenum due to pressure disturbances in the biliary organ. In addition, these processes may be caused by blockage of the bile ducts with stones that arose as a result of the first causes. Ultimately, we can conclude that the fundamental reason why gallstones occur is a violation of the composition of bile. Secondary stones most often occur due to infection. They can occur both in the organ itself and in its ducts. While primary formations appear due to the fact that the consistency of the bile becomes too thick.
- 1. The first breakfast should include approximately 100-150 g of buckwheat, several slices of rye bran and weak tea with lemon, preferably without sugar.
- 2. The next breakfast consists of grated carrots, to which you need to add just a few drops of olive oil.
- 3. For lunch, you can cook low-fat borscht from beets or cabbage, adding bran if desired. For the second course, they eat porridge with dried apricots, and you are allowed to drink a rosehip decoction.
- 4. The afternoon snack should be as light as possible; a glass of apricot juice is enough.
- 5. For dinner, you can have curd pudding and wash it down with unsweetened tea.
- 6. At night, it is recommended to drink a little rosehip decoction.
- 1. For breakfast you should include some oatmeal, which is best boiled in milk, but do not add butter, but breakfast can be slightly sweetened. Be sure to wash down your food with warm tea and lemon.
- 2. After about two hours, you need to eat a small handful of soaked prunes.
- 3. Lunch should include low-fat cabbage soup. The second course is served with boiled butter without spices, as well as a salad of beets and sunflower oil. For dessert, you can eat an apple or mash it with honey.
- 4. A small amount of vegetable salad is eaten as an afternoon snack and washed down with a warm rosehip decoction.
- 5. For dinner, it is recommended to prepare buckwheat balls, eat some cottage cheese, pudding or yogurt and wash it down with sweet tea.
- 6. Before going to bed, you can drink a rosehip decoction or a glass of carrot juice.
- 7. It is important to eat several slices of bran bread throughout the day.
- 1. In this case, breakfast should consist of 250 g of millet porridge, cooked in milk. It is best to eat it together with grated carrots. Breakfast is washed down with sweet tea with lemon.
- 2. After some time, consume approximately 50-100 g of soaked dried apricots, which should be washed down with bran decoction or unsweetened tea.
- 3. For lunch, it is better to cook soup from pearl barley and vegetables. It is advisable to finely chop all the ingredients and add bran decoction. You can prepare steamed cutlets from lean chicken meat, cabbage salad with olive oil without vinegar. Lunch is washed down with rosehip decoction or compote.
- 4. The afternoon snack should be as light as possible, for example, one or two finely chopped apples.
- 5. For dinner, it is better to eat some low-fat cottage cheese and prepare cabbage cutlets and, of course, sweet tea with lemon.
- 6. Before going to bed, you need to drink a glass of tomato juice.
- 7. During the day, it is recommended to eat several pieces of bran bread and no more than 30 g of sugar in between meals.
Show all
What is gallstone disease?
Gallstone disease is a disease characterized by the formation of stones in the gallbladder and its ducts. This occurs due to disruption of metabolic processes in the body. This disease has another name - cholelithiasis.
The gallbladder plays an important role. This organ is adjacent to the liver, and is a kind of reservoir in which bile is stored. In this case, stones can be stored both in the bladder itself and in its ducts. In some cases, they can even be found in the liver. As a rule, stones differ in diameter, weight, and can have different shapes and different compositions. Quite often, gallstone disease can provoke inflammatory processes, in which case it is the gallbladder that suffers, because it is its walls that are irritated during the course of the disease.
Gallstones form from cholesterol crystals. IN in rare cases The basis can be lime salts. At the moment when one of the stones begins to block the bile duct, and pain symptom. It is through these ducts that bile enters the small intestine.
This disease is quite common, because not everyone can lead a completely healthy lifestyle and eat right. In most European and Western countries The number of adults who suffer from gallstones reaches 10%. Among people over the age of 70, this figure is even higher - approximately 30%. Currently, operations to remove stones significantly exceed the number of operations to remove appendicitis.
Gallstone disease most often occurs among the population of large cities and industrialized settlements. It is here that people are accustomed to eating junk food, processed foods and food that is rich in fats and animal proteins. According to the latest data, gallbladder disease occurs 5-8 times more often among women than among men.


Causes of pathology
Healthy bile in the human body has a liquid consistency and cannot form stones, otherwise problems arise. This can happen if its composition and properties change sharply, for example, when great content cholesterol if the outflow is disrupted and the contents of the gallbladder stagnate. An infection that develops cholecystitis can also affect such processes.
Of course, the main reason lies in a change in the composition of the contents of the gallbladder, the balance between bile and cholesterol is disrupted. In this case, there are too few bile acids in the bladder, which causes the fluid to become noticeably thicker, resulting in the formation of stones.
Excessive cholesterol levels can occur due to the following reasons:
At the same time, the reasons why congestion and difficulties with the outflow of bile may occur are:

In addition to all the listed reasons, disruption of the outflow of bile can also occur due to mechanical reasons, for example, if there are various obstacles to its movement. Such phenomena include adhesions, benign and malignant tumors, and edema. Congenital abnormalities include protrusion of the walls of the duodenum and the appearance of cysts on the bile ducts.
Of course, the possibility of developing an infection in the gallbladder cannot be denied. This usually happens through the intestines or through the blood. Gradually, the infection reaches the gallbladder.
Chronic cholecystitis is a condition in which the disease is maintained for a long period of time and becomes more complicated in the presence of other, more serious diseases.
In this case, there are two types of gallstone formation:


What size can stones reach?
The gallbladder is an organ that is designed to store bile. It is a hollow structure. Bile collects in this organ and is gradually sent to the duodenum. This substance consists of acids. It is directly involved in human digestion. If this acid is idle for a long time, it begins to precipitate and forms the so-called bile sand. Over time, this sediment begins to concentrate, thicken and collect into larger compounds. This is how stones are formed.
Gallstones are divided into two types - complex and homogeneous. Homogeneous compounds do not have any features, while complex compounds consist of a body, a cortex, and a core inside. Chemical composition Gallstones can be divided into several types: cholesterol-based, lime-based, pigment-based and mixed.

Those stones that have a pigment composition, in most cases, contain a large amount of lime salt, which is why they are most often called pigment-limestone. They can also differ in their structure and form in the form of layers or crystals. The consistency of the stones can be waxy or hard, like real rock. As a rule, in one gall bladder there are no formations that are identical in all respects; most often it contains stones with different compositions, shapes and sizes.
Stones can form within completely different limits, and sometimes the difference in comparison is very large - they can reach sizes ranging from several millimeters to several centimeters. In more severe cases, formations can reach the size walnut or even be the size of a chicken egg. Sometimes the stone can reach very large sizes and occupy the entire free cavity of the gallbladder. In this case, its weight can reach 80 g.
Small stones with an insignificant diameter can pass through the bile ducts, so they are much easier to get rid of. If there are larger formations, then big problems and a number of painful symptoms.

Rules for creating a diet
The main rule of nutrition in the case of such a serious illness is to eat in small fractional portions, about 6 times a day. The most important thing in this case is to create a certain regime and stick to it. It is important to strictly follow the meal schedule and not miss the next portion.

No matter how strange it may sound, the most effective remedy that can remove bile is regular and frequent meals, i.e. a properly organized diet for gallstones. If you constantly follow the schedule, the bile will be excreted faster, which means that the outflow will occur more often and faster. In this case, it is important not to eat a large amount of food at one time, in which case the load on the gallbladder will be too great, and the organ will contract too intensely and sharply. This may not lead to the best consequences.
As a rule, the diet of a person who suffers from gallstones should be based on animal protein, which means that there should be a lot of it on the menu.
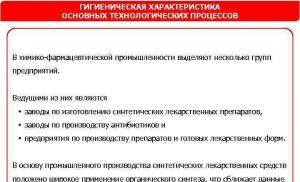
So, the diet for gallstones implies the following.
First courses. This list can include vegetarian soups and borscht. This list can include borscht made from fresh cabbage, beetroot soup, vegetable-based soups with the addition of various cereals, with pasta, and with the addition of fruits. When preparing soups, vegetables and flour are not sauteed and no oil is added; it is best to slightly dry the ingredients.
Second courses. When preparing dishes from meat ingredients and chicken, only lean meat should be used. Beef, chicken, rabbit, turkey, and young lamb are perfect for this. In this case, it is best to choose sirloin, which does not contain fat, but consists mainly of protein. When preparing poultry dishes, you need to remove the skin, as it contains a large amount of cholesterol. First, the meat should be boiled and then baked without adding oil or fat. Pilaf for cabbage rolls is also prepared with boiled meat. Cutlets and meatballs should be steamed only; the ingredients should not be fried.
As for fish dishes, it is important to consider that you can only eat those products that contain no more than 5% fat. Such fish include sea bass, cod, smelt, pike and pike perch. First, the fish is boiled and then baked. It can be served either as a whole piece or in the form of cutlets or fish balls.
Vegetable dishes. You can eat almost all types of vegetables. They can be served directly raw, as well as baked and boiled vegetables with a side dish or cheese. It is recommended to boil onions before cooking. It is best to add sour cream or vegetable oil to salads, preferably olive oil. You should not add fresh onions and vinegar to the vinaigrette. It is recommended to “lean on” fresh or sauerkraut, cucumbers, green peas, parsley, dill, and lettuce. It is allowed to eat soybean curd.
Cereals and pasta. You are allowed to eat all types of cereals. Buckwheat and oatmeal are especially useful. An excellent option is to prepare puddings with vegetables and pilaf with dried fruits. You can boil the pasta, serve and bake the noodles.

Egg dishes and sauces. If you have a disease, and especially with an exacerbation of the gallbladder, you should not eat more than two yolks with food per day. Protein can be eaten in large quantities, for example in the form of an omelet. Sauces should be prepared only from vegetables or dairy products. Fruits are used for desserts. Under no circumstances should you resort to sautéing.
Milk based products. Almost all dairy products can be consumed. The exception is some types of sharp and smoked cheeses and feta cheese, which is made from brine. Cottage cheese should not be too fatty or overly sour. Curdled milk and kefir can be included in your daily diet. This list can include all baked foods, such as lazy dumplings, various casseroles and puddings.
Snacks. These include vegetable salads with the addition of olive or sunflower oil without vinegar. It could be a vinaigrette jellied fish in jelly, which has been previously boiled. Fruit snacks, zucchini caviar, salads from lean boiled meat and seafood, cheese and ham with a low fat content.
Drinks include tea with the addition of low-fat milk, rosehip-based infusion, various vegetable juices, beetroot and carrot drinks are most recommended. Sometimes you can drink coffee with milk, but the drink should be of low concentration. When treatment is prescribed, cocoa is strictly prohibited.

Their fruits are best to stick to non-acidic berries and fruits. You can include dried fruits, mousses and jellies in your diet. You can drink compotes and jelly. Among the sweets allowed are jam, marshmallows, marmalade, candies without added chocolate, and lollipops. It is best not to consume refined sugar; sorbitol is an excellent substitute.
Flour products and fats
It is best to eat bread made from durum wheat. You can’t eat fresh, only cooked flour products; it’s better to let them be a little stale. In small quantities, you can treat yourself to lean pastries and biscuits. It is better not to eat pancakes and pancakes. From fats you can use olive, sunflower and butter. However, you should remember that you cannot use them for frying, but simply add them to dishes. It is not recommended to use spices for cooking during the treatment period.
IN dietary nutrition For gallstones, it is recommended to add olive oil to salads. The most important thing during this period is to use those products that are rich in fiber and magnesium salts. Such products stimulate the excretion of stagnant bile and help reduce the amount of cholesterol in the body. In addition, the function of the small intestine and gallbladder is enhanced.

If you have gallbladder disease, it is important that your diet be as low-calorie as possible. The diet should be calculated so that the body receives no more than 2300 calories per day. This effect is achieved by reducing carbohydrate intake and enriching the diet with proteins. Fats will also be appropriate in such a diet, but not more than 70 g per day. Weight loss has a positive effect on the course of treatment.
What is prohibited?
When dieting for gallstones, all processed foods, fast food, alcohol, carbonated drinks, spices, saltines and smoked foods are excluded. You should not eat fatty meat, smoked, cooked on charcoal, fried, or baked with oil. It is prohibited to consume canned food and offal, such as kidneys, liver, heart, gizzard, brains and much more.

Vegetables that contain large amounts of essential oils, such as radishes, garlic, onions, celery and radishes, are also contraindicated for gallstone disease. Do not add sorrel and spinach to dishes. It is advisable to limit the consumption of baked goods, chocolate, halva, and marshmallows.
Where should you start your diet?
The most effective method The fight against gallstones is a magnesium diet. The fight against the problem is based on magnesium salts, vitamins and fiber. Magnesium salts have a complex effect; they not only help remove stones, but can also eliminate inflammation and spasms. This diet excludes the consumption of fish, salt and meat.

Most patients admit that after such treatment they actually experience noticeable relief, unpleasant symptoms disappear, pain goes away, and inflammation subsides. In addition, the intestines begin to work much better, and cholesterol levels decrease. A similar diet for gallstones is especially recommended for those whose disease is accompanied by frequent constipation.
However, for gastritis and other acute diseases of the gastrointestinal tract, such a diet, alas, is contraindicated. For prolonged exacerbations, a soft and gentle diet is recommended, with minimal stress on the digestive system. In the first days of the diet it is necessary to apply therapeutic fasting, to do this, you need to drink not too sweet drinks, teas, juices and decoctions throughout the day. You should not drink drinks very often or in large portions. Decoctions should be drunk in small portions, in small sips.
Two days later, fruits and vegetables, preferably pureed, are added to the diet for gallstones.
You can eat a light cereal-based soup once a day.

It is best to use rice or oatmeal as a base. Porridge with pureed fruit will also work. You can drink jelly, eat unsweetened mousses. Gradually, the diet includes cottage cheese with a small amount of fat and lean meat. All of the listed products can be consumed either raw or boiled and steamed. Cooked food must be divided into 6 meals and consumed in small fractional portions, chewing thoroughly. Only after this can you move on to the main diet, which lasts about 3-4 weeks.
Effective Diet Plans
With the Camper diet, you should consume only 300 g of unsweetened fresh fruit compote per day and 50 g of rice porridge. The sugar diet uses 180 g of sugar and 6 glasses of hot tea. The prepared drink lasts for the whole day and is consumed in small sips.
A diet for gallstones based on kefir and cottage cheese is very effective. 900 g of kefir and 300 g of cottage cheese are consumed per day. In addition, if desired, you can add a little sugar to both kefir and cottage cheese. If the diet is applied in the summer, you can use fruit-based fasting days from time to time. You can eat watermelons, berries, apples, grapes. After some time, the patient’s well-being improves significantly. For gallstones it is better to use easy recipes and do not use any medications.

Sample menu for the day
Option #1:
Option #2:

Option #3:
The duration of the diet for gallstones should not last more than 30 days. Before starting treatment, you should consult a doctor, otherwise the results of self-medication will be sad.
And a little about secrets...
A healthy liver is the key to your longevity. This organ performs a huge number of vital functions. If the first symptoms of a gastrointestinal or liver disease have been noticed, namely: yellowing of the sclera of the eyes, nausea, rare or frequent bowel movements, you simply must take action.
During relapses of the disease, foods with fats are excluded. All vegetables are ground before consumption.
Sample diet menu for patients with cholelithiasis:
| Days of the week | 1 breakfast | 2 breakfast | dinner | afternoon tea | dinner |
| Monday | potato pancakes, oatmeal, beet juice | 1 baked apple or fruit soufflé | boiled fillet, vegetarian cabbage soup, tea | vinaigrette | steamed meat cutlets, baked potatoes, fruit juice |
| Tuesday | steamed meat cutlets, rice porridge, tea | 100 g prunes, apple juice | rice soup, baked vegetables, green tea | bran bread, compote | sandwich with squash caviar, boiled hake, carrot juice |
| Wednesday | milk soup with noodles, 2 crackers, rosehip decoction | low-fat cottage cheese, jelly | stew with eggplant and cabbage, hake stewed with sour cream sauce, tea | baked apple with honey | baked pike perch with potatoes, sliced vegetables, jelly |
| Thursday | semolina porridge, biscuits, chamomile infusion | 100 g dried apricots, sweet apple | cream soup with potatoes and cauliflower, 2 crackers, tea | homemade yogurt without fillers | beet pancakes, biscuits, compote |
| Friday | low-fat cottage cheese with honey, oatmeal, weak coffee | baked apple with jam, jelly | cream soup with Brussels sprouts, boiled fillet, weak coffee | sandwich with zucchini caviar | cottage cheese casserole, 100 g boiled meat, tea |
| Saturday | rice porridge, soft-boiled egg, chamomile infusion | low-fat cottage cheese with dried apricots, juice | rice soup, fish cutlets, vegetable stew, vegetable juice | pumpkin porridge, compote | protein omelet, sliced vegetables, weak tea |
| Sunday | cheesecakes with jam, semolina porridge, weak coffee | sweet apple and dried fruits | borscht in vegetable broth, boiled turkey, compote | liver biscuits, fruit juice | millet porridge with boiled fillet, tea |
The diet provides for five meals a day. It is recommended to eat porridge with milk for breakfast. As a drink, weak tea or decoctions of medicinal herbs - chamomile, rose hips, St. John's wort - are suitable.
With obesity, the pH level of bile shifts to the acidic side, which stimulates stone formation. In this case, you must follow a strict diet with limited cereals and pasta.
Recipes
The diet for cholelithiasis is balanced, so it is not difficult to follow. Alternating meat, vegetable and cereal products, they create a varied menu. When digestive diseases recur, the menu includes first courses in the form of soups, and more vegetables are added to second courses.
- Oatmeal soup. Boil the oatmeal over low heat for at least 30 minutes. The strained broth is salted and aromatic herbs – celery or marjoram – are added.
- Cream soup. Boil cauliflower and potatoes. Grind in a blender or rub through a sieve. Boil the oatmeal and chop it too. Combine the ingredients and add a little vegetable broth.
- Baked pumpkin. Place the pumpkin on a baking sheet and bake for at least an hour at 180°C. Cut it into cubes, removing the skin and seeds. Pour sour cream sauce over the pieces and add a little cinnamon.
- Hake with vegetables. Patisson, green peas, carrots are grated. Place vegetables on prepared baking sheet. Place hake fillet on a vegetable bed. Season with unrefined oil and sour cream. Bake for 20 minutes at 180°C.
To restore the balance of beneficial bacteria in the intestines in case of gastrointestinal diseases, eat a moderate amount of dried fruits. By following a diet, immunity increases and problems with stool disappear.
Diet features
When preparing a diet, take into account:
- biliary inflammation phase;
- weight and age;
- bowel regularity;
- background diseases, etc.
The chemical composition of the therapeutic nutrition system must be physiological, that is, correspond to the age, degree of physical activity, and gender of the patient.
 For diseases of the gastrointestinal tract, food is taken often. If inflammation worsens, smoked and rich foods are completely removed from the menu.
For diseases of the gastrointestinal tract, food is taken often. If inflammation worsens, smoked and rich foods are completely removed from the menu. During exacerbation of cholelithiasis
The diet for gallstone disease during an exacerbation involves avoiding fried foods. To improve your well-being you should:
- exclude meat dishes for 10 days;
- grind vegetables in a blender;
- eat only boiled or baked vegetables;
- do a drinking day every 7 days;
- take soups, low-fat sour milk, and vegetables as the basis of your diet.
This diet is followed for 2 weeks after an attack of gallstone disease. After stabilization of health, they move to table No. 5.
For inflammation of the gallbladder
A well-designed diet prevents bile from thickening. In case of relapse of the disease, it is advisable to:
- refuse food for 1-2 days;
- drink up to 2 liters of Narzan, Borjomi or other mineral water per day;
- after two days, add grated vegetables and fruits to the menu;
- eat food every 2 hours.
When you need to eat slimy oatmeal soups, porridge with rice. After the symptoms of the disease subside, the menu is expanded to include cottage cheese, beef, fish, and crackers.
After stone removal
The diet after crushing stones is aimed at stimulating bile drainage. The menu includes chemically neutral products that do not irritate the gastrointestinal tract, but improve the flow of bile.
 After laparoscopy, the diet is followed for 6-10 months. Refusal of a rational nutrition system is dangerous due to complications.
After laparoscopy, the diet is followed for 6-10 months. Refusal of a rational nutrition system is dangerous due to complications. Nutrition principles:
- energy value of the daily diet – 1800-2000 kcal;
- the ratio of proteins, lipids and carbohydrates is 1:1:4;
- optimal mode heat treatment– cooking;
- the volume of one serving is no more than the size of a fist;
- the temperature of food consumed is up to 50°C.
For a week after the operation, food is taken pureed. Only from the fifth day is it allowed to eat meat dishes.
After removal of the gallbladder with stones
– a serious operation that affects the functions of the gastrointestinal tract. For a month, patients must follow a diet taking into account the following rules:
- Do not eat on the eve of cholecystectomy. You can drink up to 0.5 liters of water.
- The day after cholecystectomy, you are allowed to eat pureed vegetable soups. You can drink chamomile decoction or kefir.
- Consume after 5 days diet cutlets, meatloaves, chicken soufflé, fish.
A week later, light foods are introduced - porridge, pureed soups, boiled vegetables.
What foods dissolve gallstones?
For diseases of the hepatobiliary system, foods that have lipotropic properties are introduced into the diet. They reduce the amount of cholesterol in the blood, preventing its excretion in the bile. Due to the dispersion of triglycerides, the stones are broken down.
In case of exacerbation of diseases, the diet includes:
- beef;
- low-fat cottage cheese;
- unrefined oil;
- zander;
- shrimps;
- soy flour, etc.
These products are rich in lipotropic substances that stimulate the breakdown of stones. But gastroenterologists do not recommend resorting to such treatment on your own. If the disease is accompanied by stone formation, as the size of the stone decreases, the risk of blockage of the bile ducts increases. Therefore, a diet for diseases of the hepatobiliary system should be compiled and adjusted only by a doctor.

Literature
- Cherenkov, V. G. Clinical oncology: textbook. manual for the postgraduate system. education of doctors / V. G. Cherenkov. – Ed. 3rd, rev. and additional – M.: MK, 2010. – 434 p.: ill., table.
- Ilchenko A.A. Diseases of the gallbladder and biliary tract: A guide for doctors. - 2nd ed., revised. and additional - M.: Publishing House "Medical Information Agency", 2011. - 880 p.: ill.
- Tukhtaeva N. S. Biochemistry of biliary sludge: Dissertation for the degree of candidate of medical sciences / Institute of Gastroenterology of the Academy of Sciences of the Republic of Tajikistan. Dushanbe, 2005
- Litovsky, I. A. Gallstone disease, cholecystitis and some diseases associated with them (issues of pathogenesis, diagnosis, treatment) / I. A. Litovsky, A. V. Gordienko. - St. Petersburg: SpetsLit, 2019. - 358 p.
- Dietetics / Ed. A. Yu. Baranovsky - Ed. 5th – St. Petersburg: Peter, 2017. - 1104 p.: ill. - (Series “Doctor’s Companion”)
- Podymova, S.D. Liver diseases: A guide for doctors / S.D. Podymova. - Ed. 5th, revised and additional - Moscow: Medical Information Agency LLC, 2018. - 984 p.: ill.
- Schiff, Eugene R. Introduction to Hepatology / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray; lane from English edited by V. T. Ivashkina, A. O. Bueverova, M.V. Mayevskaya. – M.: GEOTAR-Media, 2011. – 704 p. – (Series “Liver diseases according to Schiff”).
- Radchenko, V.G. Fundamentals of clinical hepatology. Diseases of the liver and biliary system. – St. Petersburg: “Dialect Publishing House”; M.: “Publishing house BINOM”, – 2005. – 864 p.: ill.
- Gastroenterology: Handbook / Ed. A.Yu. Baranovsky. – St. Petersburg: Peter, 2011. – 512 p.: ill. – (National Library of Medicine Series).
- Lutai, A.V. Diagnosis, differential diagnosis and treatment of diseases of the digestive system: Tutorial/ A.V. Lutai, I.E. Mishina, A.A. Gudukhin, L.Ya. Kornilov, S.L. Arkhipova, R.B. Orlov, O.N. Aleutian. – Ivanovo, 2008. – 156 p.
- Akhmedov, V.A. Practical gastroenterology: A guide for doctors. – Moscow: Medical Information Agency LLC, 2011. – 416 p.
- Internal diseases: gastroenterology: A textbook for classroom work of 6th year students in specialty 060101 - general medicine / comp.: Nikolaeva L.V., Khendogina V.T., Putintseva I.V. – Krasnoyarsk: type. KrasSMU, 2010. – 175 p.
- Radiology (radiation diagnostics and radiation therapy). Ed. M.N. Tkachenko. – K.: Book-plus, 2013. – 744 p.
- Illarionov, V.E., Simonenko, V.B. Modern methods of physiotherapy: A guide for general practitioners (family doctors). – M.: OJSC “Publishing House “Medicine”, 2007. – 176 p.: ill.
- Schiff, Eugene R. Alcohol, drug, genetic and metabolic diseases / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray: trans. from English edited by N.A. Mukhina, D.T. Abdurakhmanova, E.Z. Burnevich, T.N. Lopatkina, E.L. Tanashchuk. – M.: GEOTAR-Media, 2011. – 480 p. – (Series “Liver diseases according to Schiff”).
- Schiff, Eugene R. Liver cirrhosis and its complications. Liver transplantation / Eugene R. Schiff, Michael F. Sorrell, Willis S. Maddray: trans. from English edited by V.T. Ivashkina, S.V. Gauthier, J.G. Moysyuk, M.V. Mayevskaya. – M.: GEOTAR-Media, 201st. – 592 p. – (Series “Liver diseases according to Schiff”).
- Pathological physiology: Textbook for medical students. universities / N.N. Zaiko, Yu.V. Byts, A.V. Ataman et al.; Ed. N.N. Zaiko and Yu.V. Bytsya. – 3rd ed., revised. and additional – K.: “Logos”, 1996. – 644 p.; Ill. 128.
- Frolov V.A., Drozdova G.A., Kazanskaya T.A., Bilibin D.P. Demurov E.A. Pathological physiology. – M.: OJSC Publishing House “Economy”, 1999. – 616 p.
- Mikhailov, V.V. Fundamentals of pathological physiology: A guide for doctors. – M.: Medicine, 2001. – 704 p.
- Internal medicine: Textbook in 3 volumes - Vol. 1 / E.N. Amosova, O. Ya. Babak, V.N. Zaitseva and others; Ed. prof. E.N. Amosova. – K.: Medicine, 2008. – 1064 p. + 10 s. color on
- Gaivoronsky, I.V., Nichiporuk, G.I. Functional anatomy of organs digestive system(structure, blood supply, innervation, lymphatic drainage). Study guide. – St. Petersburg: Elbi-SPb, 2008. – 76 p.
- Surgical diseases: Textbook. / Ed. M.I. Kuzina. – M.: GEOTAR-Media, 2018. – 992 p.
- Surgical diseases. Guide to examining a patient: Textbook / Chernousov A.F. and others - M.: Practical Medicine, 2016. - 288 p.
- Alexander J.F., Lischner M.N., Galambos J.T. Natural history of alcoholic hepatitis. 2. The longterm prognosis // Amer. J. Gastroenterol. – 1971. – Vol. 56. – P. 515-525
- Deryabina N.V., Ailamazyan E.K., Voinov V.A. Cholestatic hepatosis in pregnant women: pathogenesis, clinical picture, treatment // Zh. obstetrics. and wives disease 2003. No. 1.
- Pazzi P., Scagliarini R., Sighinolfi D. et al. Nonsteroidal antiinflammatory drug use and gallstone disease prevalence: a case-control study // Amer. J. Gastroenterol. – 1998. – Vol. 93. – P. 1420–1424.
- Marakhovsky Yu.Kh. Gallstone disease: on the way to diagnosing early stages // Ros. magazine gastroenterol., hepatol., coloproctol. – 1994. – T. IV, No. 4. – P. 6–25.
- Higashijima H., Ichimiya H., Nakano T. et al. Deconjugation of bilirubin accelerates coprecipitation of cholesterol, fatty acids, and mucin in human bile–in vitro study // J. Gastroenterol. – 1996. – Vol. 31. – P. 828–835
- Sherlock S., Dooley J. Diseases of the liver and biliary tract: Trans. from English / Ed. Z.G. Aprosina, N.A. Mukhina. – M.: GEOTAR Medicine, 1999. – 860 p.
- Dadvani S.A., Vetshev P.S., Shulutko A.M., Prudkov M.I. Gallstone disease. – M.: Publishing house. House “Vidar-M”, 2000. – 150 p.
- Yakovenko E.P., Grigoriev P.Ya. Chronic diseases liver: diagnosis and treatment // Rus. honey. zhur. – 2003. – T. 11. – No. 5. – P. 291.
- Sadov, Alexey Cleansing the liver and kidneys. Modern and traditional methods. – St. Petersburg: Peter, 2012. – 160 pp.: ill.
- Nikitin I.G., Kuznetsov S.L., Storozhakov G.I., Petrenko N.V. Long-term results of interferon therapy for acute HCV hepatitis. // Ross. magazine gastroenterology, hepatology, coloproctology. – 1999, vol. IX, No. 1. – p. 50-53.
The principles of nutrition are as follows:
- Refusal of very fatty and fried foods.
- Eating only warm food.
- Avoid overeating.
- The daily fluid intake is 2000 ml.
- There are two ways to cook food: steamed and boiled.
- The menu should include products from both animals and plant origin. The diet is based on fruits and vegetables.
Pay attention! You need to eat food 5-6 times/24 hours.
Calcium rich foods
Diet for gallstone disease and diabetes mellitus includes foods rich in calcium. This element prevents the formation of stones.
Particular emphasis should be placed on the consumption of dairy and fermented milk products. Diabetics suffering from cholecystitis need to take into account the glycemic index.
Table 2. “Milk” enriched with calcium.
| Product | Daily value (g) |
|
|
150-200 |
|
|
150-200 |
|
|
150-200 |
|
|
50-70 |
|
|
200-220 |
|
|
200-250 |
|
|
100-120 |
The daily norm for adults is 800-100 mg. Older people need up to 1200 mg of calcium.

Magnesium rich foods
The diet for gallbladder stones includes foods rich in magnesium. This mineral helps accelerate the flow of bile and relieve pain. Magnesium also has a powerful anti-stress effect.
Table 3. What to include on the menu?
| Product | Daily value (g) |
|
|
200-250 |
|
|
200-250 |
|
|
50-100 |
|
|
30-60 |
|
|
30-60 |
|
|
150-200 |
The daily requirement of magnesium is 400-500 mg. When following a diet for gallstone disease, it is recommended to pay special attention to nuts.

Pay attention! The daily portion of nuts should not exceed 50 grams.
Meat products
What foods can you eat if you have gallstones? You should not give up eating meat. Before preparing the dish, you must carefully trim off the fat and remove the skin from the chicken.
Information about meat allowed in the diet for gallstones is presented in the table.
Table 4. Meat products.
| Product | Daily value (g) |
|
|
200-300 |
|
|
200-250 |
|
|
200 |
|
|
200-250 |
|
|
250-300 |
Allowed fish
What can you eat if you have gallstone disease? It is recommended to eat more fish. It can be either river or sea. Fish should not be fatty. The leaner the product, the more benefits it will bring to the body.
Table 5. What fish can you eat?
| Product | Daily value (g) |
|
|
250-300 |
|
|
300-320 |
|
|
250-350 |
|
|
200-250 |
|
|
200-220 |
|
|
250-300 |
|
|
200-250 |
What fruits can you eat if you have gallstones? Detailed information presented on the plate.
Table 6. Allowed fruits.
| Fruit | Daily value (g) |
|
|
150-200 |
|
|
Up to 350 |
|
|
100-120 |
|
|
Up to 300 |
|
|
150-200 |
|
|
150-250 |
|
|
200 |
You should avoid sour fruits. If cholecystitis is adjacent to pancreatitis, it is necessary to avoid eating grapes.
What can you eat from vegetables if you have gallstones? Recommended products are presented in the plate.
Table 7. Allowed vegetables.
| Vegetable | Daily value (g) |
|
|
20-30 |
|
|
50-100 |
|
|
60-120 |
|
|
100-150 |
|
|
50-100 |
|
|
150-250 |
Is it possible to eat tomatoes if you have gallstone disease? For pathologies of the digestive system, the benefits of tomatoes are very controversial.
Pay attention! Tomatoes are allowed to be eaten only during remission of cholecystitis.
Otherwise, the vegetable can aggravate the situation: provoke the outflow of liver secretions, or dilute the bile, increasing its fluidity. Rushing into the channels, it helps to block them with large stones. Against this background, there is a risk of death.
Other products
Table 8. Other products.
| Product | Recommendation |
|
|
It is recommended to refuse freshly baked bread in favor of yesterday's, slightly dried bread. Bread doesn't have to be rich. |
|
|
Eating spicy mushrooms, chicken and meat broths. It is recommended to eat only vegetable soups. If a person cannot completely give up meat broths, then they need to be prepared from lean varieties and diluted with water. |
|
|
They can be used in making omelettes. Soft-boiled eggs are also allowed. The permissible number of eggs per day is 1. |
|
|
It is recommended to avoid sorrel, radish, garlic, and green onions. It is allowed to use bay leaf, parsley, and dill. |
|
|
They should be crumbly, semi-viscous. The emphasis should be on eating buckwheat and oatmeal porridge. Cereal casseroles are also allowed. |
Nutrition for gallstone disease in women and men is almost no different. The only difference is that the stronger sex requires more calories. Their portions should also be a little larger.
How to eat during the week?
The main goal of the diet in the presence of gallstones is to normalize cholesterol metabolism and improve bile outflow.
Table 9. Menu for gallstone disease for a week.
| Day of the week | Breakfast | Lunch | Dinner | Afternoon snack | Dinner |
| Mon. | Steam omelet with herbs, apple and carrot salad, dressed with liquid honey. | Cottage cheese casserole + glass of yogurt. | Wheat and vegetable soup, beet caviar, 1 slice of bread. | 1 meat cutlet, steamed, 1 peeled cucumber. | 150 grams stewed cabbage, 120 grams of boiled fish. |
| Tue | Cottage cheese mixed with prunes, 150 ml berry jelly. | Vinaigrette + slice of bread. | Lenten borscht, 120 grams of boiled veal. | Vegetable salad, dressed linseed oil. | A large sweet apple baked with honey, 2 biscuits + 1 glass of fermented baked milk. |
| Thurs. | Sweetened oatmeal, 1 large sweet apple baked with honey, 150 ml kefir or fermented baked milk. | Beet salad with nuts, prunes and apples, dressed with Greek yogurt. | Potato soup, generously sprinkled with fresh herbs, a slice of bread, 120 grams of boiled or baked lean fish. | 100-150 grams of chicken fillet. | Cucumber salad dressed with flaxseed oil, 2 small baked potatoes. |
| Fri. | Grated buckwheat boiled in milk, 2 boiled eggs, 50 grams of feta cheese. | Fruit and berry salad dressed with yogurt. | 100 grams of yellow lentils, chicken fillet, 1 slice of bread. | Eggplant baked with Adyghe cheese. | Rice milk soup. |
| Sat. | Millet-apple porridge with dried apricots, 1 cup of tea with a slice of lemon. | 220 grams of pumpkin baked with honey. | Mashed potatoes, 100 grams of steamed fish. | Protein omelet generously sprinkled with herbs. | Stewed cabbage, 1 steamed turkey cutlet. |
Pay attention! Wednesday is the 1st fasting day of the week. It is recommended to drink 1% kefir throughout the day. The entire volume (1000-1500 ml) should be distributed into 5-6 servings. The second fasting day of the week is Sunday. On this day you need to “destroy” 1500 g of sweet apples, dividing the entire volume into 6 servings.
How to eat during an exacerbation
During exacerbation, severe colic is observed in the hypochondrium. This condition is relieved by a magnesium diet. Magnesium helps relieve spasms and inflammation.
The amount of magnesium should exceed the standard regime by 4 times. Table salt should be avoided. Recommendations for diet for gallstone disease during an exacerbation are presented in the table.
Table 10. How to eat during an exacerbation?
| Period | Recommendations | What can you eat? |
|
|
It is recommended to avoid solid foods. You should only eat liquid, thoroughly pureed foods. In case of exacerbation of cholelithiasis, special attention should be paid to porridge recipes. | Liquid oatmeal boiled in water. You should drink natural fruit juices diluted with boiled water in a 1:1 ratio. You can also drink warm rosehip decoction. |
|
|
Slimy soups with semolina or rice. | Fruit mousse, jelly, fruit jelly. |
|
|
Low-calorie foods are allowed. All products must be ground through a strainer or crushed in a blender. | Cottage cheese, steamed fish, beef or veal. |
Nutrition after surgery

After removal of gallstones, a gentle diet is prescribed.
The instructions look like this:
- 1 day – complete abstinence from food. It is recommended to hold a small amount of mineral water or rosehip decoction in your mouth and then spit it out. You can also periodically moisten your lips with a damp cloth.
- Day 2 – fluid intake is allowed. You need to drink slowly, in small sips. It is advisable to drink mineral water after releasing the gas from it.
- 3 days after removal of gallstones - the diet includes pureed vegetable soups. It is allowed to add 1 tsp there. sour cream or butter.
- Day 4 – steamed curd pudding, mashed potatoes.
- 5-6 days – pureed porridge, dried white bread.
Pay attention! For 8 days after surgery, you need to eat up to 8 times/24 hours, including at night. Portion sizes are up to 200 grams. In the morning, before meals, it is recommended to drink 100-150 ml of unsweetened compote. At night, you can take 3-5 sips of rosehip decoction.
Doctors recommend eating pureed food for 1.5-2 months after surgery. You can expand your diet only six months after surgery. New dishes should be introduced gradually, not forgetting to analyze the state of your health.
How to eat with cholecystitis and pancreatitis?
Nutrition for gallstone disease and pancreatitis necessarily includes:
- fiber;
- ascorbic acid;
- vitamin A;
- vitamin B9;
- vitamin PP.
Products with fiber
It helps remove waste and toxins from the body. Also, due to the activity of fiber, the concentration of harmful fats is reduced. This leads to healthier liver and pancreas. As metabolic processes accelerate, body weight decreases.
The daily fiber intake is 25-35 grams.

During an exacerbation of pancreatitis, the need for fiber decreases.
Products with ascorbic acid
It is a powerful antioxidant and cofactor for several important reactions. Also called vitamin C. The daily requirement ranges from 95 to 110 mg. Persons who abuse tobacco products require 35 mg more.

Ascorbic acid promotes better absorption of iron contained in the liver. The following combination is recommended: artichoke + red pepper, spinach + sweet strawberries.
Products with vitamin A
This is a fat-soluble vitamin and a powerful antioxidant. Combines well with vitamins C and E, thereby helping to protect the body from oxidation. The daily requirement for this vitamin varies from 350 to 950 mcg.

Pay attention! It is advisable to combine products with vitamin A with “healthy” fats.
Spinach goes well with avocado, carrots with lettuce.
Vitamin B9 Products
This vitamin helps normalize the functioning of the digestive system, has beneficial influence on fat metabolism in the liver. B9 also helps accelerate cholesterol metabolism. The daily requirement for this vitamin is 1000 mcg.

The beneficial effect on the body is enhanced by the combination of this vitamin with B12.
Products with vitamin PP
Also called niacin. Promotes the release of energy from fats and carbohydrates for protein metabolism. Part of the enzymes that provide cellular respiration.
Normalizes the functioning of the stomach and pancreas. The daily requirement is 16-28 mg in men and 14-20 mg in women.

Conclusion
The diet must be followed for 12 months. It must not be violated, otherwise gallstone disease will return. In this case, removal of stones from the bile ducts will be required.
The video in this article will tell you more about what diet is prescribed for gallstone disease.
In the section Diet for gallstones describes the characteristics of the diet, recommended and excluded foods and dishes, diet, cooking products and also presents recipes for a variety of dishes recommended by leading nutritionists for a diet for gallstones.
Causes of gallstones formation:
Stones in the gall bladder, and sometimes in biliary tract, arise due to the presence of infection in the biliary tract, stagnation of bile and a disorder of cholesterol metabolism.
Chemical composition of the diet for gallstones:
A complete diet for gallstones contains:
The normal amount of protein is 100g (animal proteins should be 50-75%),
Limited amount of fat 80-70g,
The normal amount of carbohydrates is 400-450g (sugar - 70-80g),
The calorie content of the diet is 2800-2900 kcal.
Characteristics of the diet for gallstones:
Of particular importance is the introduction of vitamin A with food (up to 10 mg per day), which prevents the formation of stones.
Exclusion of foods containing a lot of cholesterol (brains, liver, kidneys, lungs, heart, fatty meats and fish, pork, beef, lamb fats, cream, cod liver oil, halibut), since most often stones with stagnation of bile are formed from cholesterol .
Including an increased amount of foods containing fiber (fruits, vegetables) and helping to remove cholesterol from the body.
Inclusion of products containing lipotropic substances - methionine and choline, which are components of protein that prevent fatty liver (cottage cheese, buckwheat, oatmeal, lean meats and fish).
Diet for gallstones foods and dishes excluded:
Meat and fish broths, fried foods, alcohol, smoked meats, offal, sausages, canned food, spinach, sorrel, radishes, green onions, garlic, marinades, mustard, horseradish, pepper, chocolate, creams, pork are excluded from the diet for gallstones. , beef, lamb fats.
Diet for gallstones diet:
Food must be taken 5 times a day, meals in fractions to enhance the outflow of bile.
Culinary processing of foods for a diet for gallstones:
Food is given unprocessed; only stringy meat and fiber-rich vegetables are pureed. Products are boiled or baked (not fried), sometimes stewed. Avoid very cold foods.
1.First courses: vegetarian cabbage soup and borscht, beetroot soup, vegetable soups, vegetable broth soups with cereals, pasta, dairy, fruit soups. Flour and vegetables for preparing first courses are not sauteed, but dried.
2.Main courses:
-Meat and poultry dishes: lean beef, rabbit, lean chicken, turkey, pork, lean young lamb are used (veal and chicken are undesirable). The bird is cooked without skin. The meat is first boiled and then baked, served in pieces or chopped. Milk sausages. Pilaf and cabbage rolls are prepared with boiled meat. Dishes made from cutlet mass are allowed: steamed cutlets, meatballs, quenelles.
-Fish dishes: Fish with a fat content of no more than 5% is allowed (pike perch, pike, navaga, silver hake, smelt, cod, freshwater and sea bass). The fish is boiled, baked after boiling, served in pieces or in the form of meatballs, steamed cutlets, quenelles, and soufflés.
-Vegetable dishes: various types vegetables (except those excluded), vegetables are given raw, boiled, baked, stewed. Onions are added after boiling, vinaigrettes without vinegar and fresh onions, raw grated carrots with sour cream or vegetable oil (preferably olive), fresh cucumbers, white cabbage, finely shredded, non-acidic sauerkraut, greens, green pea puree. Legumes allowed include green peas and soybean curd.
- Dishes from cereals and pasta: porridge from various cereals, especially buckwheat and oatmeal, krupeniki, puddings with carrots and cottage cheese, pilaf with dried fruits, vermicelli, boiled or baked pasta.
- Egg dishes:. for cholelithiasis - up to 1/2 yolk per day in dishes, baked egg white omelet.
- Sauces For second courses only milk, sour cream with vegetable broth, fruit and berry sauces. Flour for sauces with butter is not sautéed.
- Dairy products: milk and all dairy products, except salty, sharp cheeses, feta cheese, non-acidic and low-fat cottage cheese and sour cream, curdled milk, kefir, Dutch cheese. All dishes are boiled and baked (puddings, casseroles, lazy dumplings).
3.Snacks: vegetable salads with vegetable oil, vinaigrettes, squash caviar, fruit salads, low-fat, soaked herring, jellied fish with gelatin after boiling, stuffed fish, salads from boiled meat and fish, seafood salads, low-fat ham, low-fat cheese, pressed caviar once a week.
4.Third courses:
-Drinks: regular brewed tea with milk, rosehip infusion, vegetable juices (carrot and beetroot), very weak natural coffee with milk or completely excluded, cocoa is contraindicated.
- Fruits: various non-acidic fruits and berries, raw, boiled, baked, dried fruits, compotes, jelly, mousses, jelly, sambuca.
- Sweets: snowballs, meringues, non-chocolate candies, marmalade, honey, jam, pastille. Sugar can be partially replaced with sorbitol or xylitol.
5.Flour products: stale wheat and rye bread, small quantities of uneatable pastries with boiled meat, fish, apples, cottage cheese, cookies, dry biscuits. Pancakes and pancakes are not recommended.
7.Fats: butter, refined sunflower oil, olive. Do not fry the oil, but add it to dishes.
Diet for gallstones Olive oil is recommended with salads, vinaigrettes, increased content fiber from fruits and vegetables, increasing the content of foods rich in magnesium salts. This stimulates the secretion of bile, promotes the removal of cholesterol from the body (with stagnation of bile, gallstones are most often formed from cholesterol), and enhances the motor function of the gallbladder and small intestine.
For gallstones and concomitant obesity it is necessary to reduce the calorie content of the diet to 2200-2300 kcal by reducing the amount of carbohydrates to 250-300 g (primarily sugar, bread, butter) and fats to 70 g. Weight loss has a beneficial effect on the course of gallstone disease.
For gallstones with constipation a magnesium diet is recommended, which is based on diet No. 5. Bran bread or wholemeal flour, millet and buckwheat, increased amount fresh fruits and dried fruits, vegetables.
Dear readers, if you have cholelithiasis (GSD), you cannot do without nutritional therapy. A proper diet for gallstones helps not only to maintain lightness and excellent health, but also prevents complications, among which the most dangerous.
Particular attention to nutrition should be paid to people whose stones have already led to disruption of the functionality of the biliary tract. If the gallbladder contracts poorly, is inflamed, and secretes bile rarely and in small portions, the health of the entire digestive system is at risk.
Many people believe that the diet for cholelithiasis of the gallbladder is too strict, but this is not entirely true. Yes, the list of prohibited foods is impressive, but you should focus primarily on your body’s reaction. The most important thing is to avoid those foods that increase pain, cause nausea and colic attacks. Usually these are fatty and fried foods, alcohol, pungency and spices.
Diet goal
Proper nutrition for gallstones (diet No. 5) has the following goals:
- reducing the load on the organs of the biliary tract;
- prevention of bile stagnation and dysfunction of the gallbladder;
- prevention of complications of cholelithiasis, which often disrupt the functioning of the pancreas, liver, stomach and intestines;
- reducing the clinical manifestations of cholelithiasis, combating nausea and pain;
- prevention of biliary colic and other complications requiring urgent surgical interventions and severe traumatic operations.
A proper diet for gallstones involves a varied diet as much as possible. Daily calorie content should not exceed 2000-2500 kcal. Restrictions apply primarily to animal fats and simple carbohydrates. With cholelithiasis, a lot of cholesterol accumulates in the bile, and sweets and baked goods contribute to the destruction of blood vessels and the active development of atherosclerosis against the background of elevated lipid levels.
Therefore, gallstone disease is considered a socially significant problem today. Against the background of stone formation, other pathological changes occur in the body. But if you start following a diet in time if you have gallstones, you can minimize the negative impact of the disease on other internal organs and the gastrointestinal tract.
Ideally, you should consult a professional nutritionist or at least a hepatologist. The doctor will tell you in detail about the importance and rules of nutrition for your disease, and will select an approximate diet menu for gallstones, so that at first it will be easier for you to create a diet, avoiding monotony and vitamin deficiencies.

General principles of nutrition for gallstones
Diet has a huge impact on the condition of the gallbladder and can both promote the formation of new stones and reduce their number. Food stimulates the motor functions of the biliary tract and increases the secretion of bile.
Many people take the recommendation to give up fat too literally. But exactly fatty foods and cause the outflow of bile. When a person follows a strict diet, severely limits fats or completely abandons them, bile stagnates, its lithogenic properties increase and the stage of stone formation begins.
We need fats, but they can be beneficial, for example, when we eat certain types of meat or fish or dress salads with flaxseed oil. Or they can be harmful if, instead of boiled chicken, rabbit, turkey, we eat sausage, hot dogs or fast food. From harmful fats, the gallbladder becomes inflamed and stops working properly.
Principles of proper nutrition for gallstones:
- refusal is clear harmful products for the gallbladder: from everything fried and excessively fatty, spicy, smoked;
- a complete ban on alcoholic drinks;
- fractional meals in small portions, without overeating (for digestion large quantity food lacks bile and enzymes);
- eating at the same hours, at short intervals (no more than 3 hours);
- daily consumption of plant fiber;
- a varied diet that includes fish, meat, and dairy products;
- limiting simple carbohydrates, looking for alternatives to store-bought sweets (can be replaced with honey, homemade marmalade, jelly).
If you have gallstones, diet alone may not be enough to prevent complications. Do not ignore the recommendations of your doctor. Most often, experts prescribe long-term use of ursodeoxycholic acid, which can not only dissolve stones, but also reduce the lithogenicity of bile.
If, in addition to stones, there is biliary sludge in the bladder, it is recommended to consume oatmeal more often, drink an infusion of oats (small sips throughout the day) with the addition of magnesium (a teaspoon per 0.5-1 liter of product). This will also help dissolve and remove stones. It also has similar properties. Let's take a closer look at what you can and cannot eat if you have gallstones.

What can you eat if you have gallstones? You need to eat not only what you are used to (with the exception of prohibited dishes), but the maximum variety of permitted foods. Then you will not feel constant hunger and dissatisfaction from a meager diet.
- lean meat: you can eat veal, beef, rabbit, turkey, domestic chicken;
- lean fish;
- dried rye and wheat bread;
- soups in vegetable broths using vermicelli, vegetables and cereals, cabbage soup and borscht without fried dressing;
- low-fat dairy products, including kefir and homemade unflavored yogurt, low-fat cottage cheese in lazy dumplings and casseroles;
- egg white omelettes;
- any boiled or baked vegetables, except radishes, spinach, garlic, sorrel, radish;
- non-acidic berries and fruits;
- vegetable oils;
- vegetable juices, diluted non-acidic fruit juices, homemade compote;
- rosehip infusion, still mineral water(have a slight choleretic effect).
The diet for cholelithiasis should contain a lot of fiber. It prevents constipation, which has an extremely negative effect on the functionality of the gallbladder. Plant fibers are found mainly in vegetables and fruits. They are recommended to be baked, boiled or stewed. The amount of fat per day is no more than 80 g; it must contain vegetable oils (olive, corn, flaxseed).

Prohibited Products
If you have gallstones, you should exclude the following foods from your diet:
- fatty meats and fish;
- egg yolks;
- offal;
- meat broths;
- garlic, onion, radish, radish, spinach and sorrel;
- fatty dairy products;
- fresh bread;
- pastries, pastries, fried pies and cakes, any baked goods;
- legumes;
- strong coffee, chocolate, alcoholic drinks, sparkling water;
- sour berries;
- mushrooms;
- instant products, fast food;
- salo;
- any sausages and smoked meats;
- canned fish.
When following a diet for gallstones, it is important to avoid gas formation. Gallstone disease is often accompanied by flatulence. This is due to a lack of bile and enzymes that are involved in the breakdown of food. Food is poorly digested and begins to remain in the intestines for a long time, causing pain and discomfort. Strong gas formation is provoked by legumes, cabbage, corn, and grapes. Limit or completely avoid these foods.
When removing a gallbladder with stones, the diet will be the same - treatment table No. 5. Cholecystectomy relieves a person of a diseased organ, but does not solve the main reason for the formation of stones - a disorder of lipid metabolism. Maintaining a diet helps avoid the formation of stones in the ducts, fatty degeneration of the liver and other disruptions in the functioning of the gastrointestinal tract.

Monday
Breakfast. Buckwheat porridge on water, steamed turkey cutlet or egg white omelet.
Lunch. Low-fat cottage cheese, green tea or rosehip infusion, fresh apple.
Dinner. Vegetable soup with the addition of any cereal, fish cutlets with a spoonful of low-fat sour cream as a dressing. Vegetable stew, rosehip infusion.
Afternoon snack. baked apple, a glass of fermented baked milk or kefir.
Dinner. Fish casserole. Vegetable salad dressed with flaxseed oil.
Tuesday
Breakfast. Oatmeal with milk, low-fat cottage cheese with homemade jam without flavorings. Green tea.
Lunch. Grated apples without skin with a spoon of honey. Rose hip decoction.
Dinner. Vegetable cauliflower soup, steamed turkey cutlets. Pumpkin juice.
Afternoon snack. Curd casserole.
Dinner. Boiled fish, mashed potatoes. Green tea or rosehip decoction.
Wednesday
Breakfast. Protein omelet, oatmeal cookies. A small piece of low-fat cheese with green tea and toasted bread.
Lunch. Cottage cheese casserole, rosehip juice.
Dinner. Noodle soup with a second broth (homemade turkey, rabbit or chicken) with the addition of boiled meat. Vegetable cabbage rolls, homemade jelly.
Afternoon snack. carrot juice. Bran bread.
Dinner. Marine or river fish baked with vegetables. Diluted peach juice.
Thursday
Breakfast. Milk buckwheat porridge with the addition of a small piece of butter. Green tea.
Lunch. Low-fat cottage cheese with honey or jam.
Dinner. Vegetable pilaf. Steamed turkey cutlets. Rose hip decoction.
Afternoon snack. Baked apples. Any fruit non-acidic juice.
Dinner. Potatoes with baked pike perch. Vegetable salad (carrots, beets) with a spoon of low-fat sour cream or vegetable oil.
Friday
Breakfast. Millet porridge on water with pumpkin pieces. Oatmeal cookies. Tea with milk.
Lunch. Curd casserole.
Dinner. Stewed rabbit meat with vegetables. Dried fruit compote.
Afternoon snack. A glass of homemade yogurt with oatmeal cookies.
Dinner. Vegetable stew with fish cutlets.
Saturday
Breakfast. Protein omelet with buckwheat porridge and a piece of low-fat cheese. Green tea with oatmeal cookies.
Lunch. Baked apple. Cottage cheese with jam. Apple juice.
Dinner. Buckwheat soup with potatoes and other vegetables, adding boiled lean meat. Vegetable salad of peeled cucumbers, tomatoes and parsley.
Afternoon snack. A glass of kefir or low-fat homemade yogurt.
Dinner. Steamed turkey cutlets. Salad of boiled beets and fresh carrots with the addition of low-fat sour cream. Rose hip decoction.
Sunday
Breakfast. Curd casserole. Homemade low-fat yogurt. Tea with milk.
Lunch. Protein omelet. Grated carrots with a spoonful of sugar and honey.
Dinner. Cabbage soup without fried dressing. Boiled chicken meat. Rosehip juice.
Afternoon snack. Tea with milk, a piece of cheese and dried bread.
Dinner. Boiled fish with baked vegetables. Chamomile decoction.
Follow the basic rules of the diet and be healthy, dear readers!
You may be interested in the following topics:
This video describes the principles of nutrition for gallstones, as well as the features of diet No. 5.