How to recognize the symptoms of inflammatory bowel disease. Inflammation of the intestines: symptoms and treatment IBD symptoms
State educational institution of higher professional education "Moscow State Medical and Dental University of Roszdrav"
Medical Faculty
Maychuk E.Yu., Martynov A.I., Panchenkova L.A., Khamidova H.A.,
Yurkova T.E., Pak L.S., Zavyalova A.I.
Chronic bowel diseases
Educational and methodological manual for practical training in hospital therapy
Moscow 2012
Reviewers: Doctor of Medical Sciences Professor of the Department of Emergency Conditions at the Clinic of Internal Medicine of the Faculty of Postgraduate Education of the First Moscow State Medical University named after N.M. Sechenova Shilov A.M.
Doctor of Medical Sciences Professor of the Department of Hospital Therapy No. 2 of the State Educational Institution of Higher Professional Education MGMSU, Makoeva L.D.
Maychuk E.Yu., Martynov A.I., Panchenkova L.A., Khamidova H.A., Yurkova T.E., Pak L.S., Zavyalova A.I. Textbook for medical students. M.: MGMSU, 2012, 26 p.
The textbook describes in detail modern ideas about the classification, clinical picture, principles of diagnosis and treatment of inflammatory bowel diseases (nonspecific ulcerative colitis and Crohn's disease) and irritable bowel syndrome. The manual contains a work plan for a practical lesson, questions to prepare for the lesson, an algorithm for substantiating a clinical diagnosis; final test lessons are included, designed for students to independently assess their knowledge, as well as situational tasks on the topic.
This training manual has been prepared in accordance with the working curriculum for the discipline “Hospital Therapy”, approved in 2008 at the Moscow State University of Medicine and Dentistry on the basis of sample curricula of the Ministry of Health and Social Development of the Russian Federation and the State educational standard for higher professional education in the specialty “060101-General Medicine” "
The manual is intended for teachers and students of medical universities, as well as clinical residents and interns.
Department of Hospital Therapy No. 1
(Head of the department – Doctor of Medical Sciences, Professor Maychuk E.Yu.)
Authors: professor, doctor of medical sciences Maychuk E.Yu., academician, doctor of medical sciences Martynov A.I., professor, doctor of medical sciences Panchenkova L.A., assistant, Ph.D. Khamidova Kh.A., assistant, Ph.D. Yurkova T.E., professor, doctor of medical sciences Pak L.S., associate professor, candidate of medical sciences, Zavyalova A.I.
MGMSU, 2012
Department of Hospital Therapy No. 1, 2012
1. Definition and theoretical issues of the topic
Inflammatory bowel diseases (IBD) characterized by the presence of inflammatory-destructive processes in the intestines and a recurrent course. Crohn's disease (CD) develops segmentally in all parts of the gastrointestinal tract and affects all layers of its wall. Nonspecific ulcerative colitis (UC), on the contrary, occurs in the rectum and from there can spread to all parts of the colon, affecting only the mucous membrane.
Etiology and pathogenesis.
Currently, there is no exact information about the cause of the development of chronic inflammatory bowel diseases.
Presumable etiological factors are:
- infection (bacteria, viruses);
- disturbance of intestinal microbiocenosis (a decrease in the number of bifidobacteria while simultaneously increasing the number of pathogenic enterobacteria, anaerobic microorganisms, etc.), which has a local toxic and allergenic effect with the development of non-immune inflammation.;
- genetic determination in IBD, the connection of these diseases with antigens of the HLA system (in Russia - HLA DR3 and DR5) has been proven.
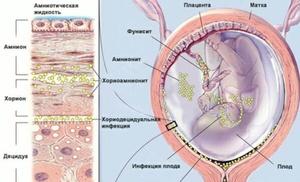
Damaging agents cause disruption of the immune response, increased permeability of the intestinal wall to antigens, antibodies are formed, as well as autoantibodies, represented by anticolon and antineutrophil antibodies. The resulting immune complexes, localized in the colon, cause immune inflammation in the mucous membrane of the colon - superficial - in UC and transmural - in CD. Nonspecific ulcerative colitis is characterized by diffuse inflammation of the intestinal mucosa, while in Crohn's disease granulomatous inflammation is observed.
In recent years, the development of the inflammatory process in the intestines
great importance is attached pro-inflammatory cytokines , especially tumor necrosis factor-α (TNF-α) , synthesized by different types of cells (macrophages, T-lymphocytes, endothelial cells). During inflammation, TNF-α behaves as an active pro-inflammatory agent. In addition, TNF-α is involved in the formation of inflammatory granuloma in CD.
Immune mechanisms cause the involvement of other organs and systems in the pathological process (extraintestinal manifestations), which include lesions of the skin, eyes, oral cavity, musculoskeletal system, and blood system.
Clinical symptoms of IBD
The main symptoms of UC are:
1.Diarrhea with blood, mucus and pus. With a pronounced clinical picture of the disease, frequent loose stools mixed with blood, mucus, and pus are characteristic. Stool up to 20 times a day, and in severe cases up to 30-40, mainly at night and in the morning. In many patients, the amount of blood in the stool is quite significant, sometimes defecation occurs almost pure blood. Diarrhea and bleeding are considered the main clinical manifestations of UC. Diarrhea is caused by extensive inflammatory damage to the mucous membrane and a sharp decrease in its ability to reabsorb water and sodium. Bleeding is a consequence of ulceration of the colon mucosa and the development of loose connective tissue with a richly developed vascular network.
2. Abdominal pain – permanent symptom of ulcerative colitis. The pain is cramping in nature and is localized mainly in the projection of parts of the colon, most often in the area of the sigmoid, transverse colon, and rectum. Usually the pain intensifies before defecation and calms down or weakens after stool. It should be noted that extremely severe pain is not typical for UC, since the inflammatory process in this disease is limited to the mucous membrane and submucosal layer.
3. Pain on palpation. On palpation, clearly defined pain is detected in the area of the sigmoid, transverse colon and cecum. The more pronounced the inflammatory process in the large intestine, the more significant the pain when palpating its parts.
4. Intoxication syndrome. Characteristic for severe UC and acute fulminant forms of the disease. Intoxication syndrome is manifested by severe weakness, adynamia, increased body temperature (often to high levels), weight loss, decreased or even complete absence of appetite, and nausea.
Currently, various clinical activity indices have been developed to assess the severity of UC; the Truelove index is the most convenient to use (Table 1).
|
Index |
Idegree |
IIdegree |
IIIdegree |
|
Frequency of bowel movements |
Less than 4 per day |
More than 6 per day |
|
|
Detection of blood in stool using a macroscope. Research |
slightly |
Much |
|
|
Fever and in the evening b)2 out of 4 days |
Over 37.5 |
||
|
Anemia |
Not expressed |
HB level is less than 75% of normal |
|
|
Tachycardia, beats/ min | |||
|
ESR, mm/h |
Table 1. Assessment of UC severity according toTruelove.
The main clinical symptoms of CD (colon localization):
1.Stomach ache cramps that occur after eating and before defecation are localized along the large intestine.
2. Pronounced diarrhea(loose or pasty stools up to 10-12 times a day). Bleeding from the rectum is much less common than with UC.
3. In 80% of patients, anal fissures, having a multiple nature; sometimes the only manifestation of the disease may be the presence of a sluggish ulcer of the anal canal with frequent transition to the skin.
4. Also an important diagnostic sign of CD, in contrast to UC
is the formation fistulas associated with the intestines, and
infiltrates of the abdominal cavity. Fistulas can be internal
(interintestinal, enterovesical, gastrointestinal and
etc.) or open on the skin, or lead to the formation
sluggish abscesses.
Infiltrates of the abdominal cavity are stationary,
painful formations fixed to the back or front
abdominal wall, usually localized in the right iliac
The most common way to assess the clinical activity of CD and the effectiveness of therapy is Best clinical activity index:
Frequency of loose (liquid or pasty) stools over the last week x 2
Abdominal pain (by intensity) (sum of points per week) x5
moderate
General health x7
overall good
slightly below normal
very bad
Other symptoms associated with CD:
Iritis, uveitis
Erythema nodosum, pyoderma gangrenosum, aphthous stomatitis
Arthralgia, arthritis
Anal fissures, fistulas, abscesses
Other fistulas
Temperature above 37.5 degrees during the last week
Number of points x20
Symptomatic treatment of diarrhea (use of symptomatic antidiarrheal drugs). If yes, then 1x30
Resistance of the abdominal wall: 0-no; 2 – unclear; 5 – clearly defined x10
Hematocrit (Hct):
Women 42 minus Hst x 6
Men 47 minus Hst x 6
8. Body weight
Body weight / normal body weight x 100
Grade:Best index less than 150 points - remission; more than 150 – exacerbation; more than 450 points - severe exacerbation.
Extraintestinal manifestations of CIBD
The development of the syndrome of systemic manifestations is caused by autoimmune disorders and reflects the activity and severity of the pathological process in inflammatory bowel diseases. The most typical extraintestinal manifestations include:
- joint damage– polyarthritis; The ankle, knee, interphalangeal joints are usually affected; the intensity of pain and the degree of restriction of movement in the joints are usually small. A feature of articular syndrome is its complete disappearance with the onset of remission; deformations and dysfunction of the joints do not develop. Some patients develop transient spondyloarthritis and sacroiliitis, and sacroiliitis is more common and more severe with more extensive lesions of the large intestine;
- eye damage– noted in 1.5-3.5% of patients, the development of iritis, iridocyclitis, uveitis, episcleritis, keratitis is typical, and the development of retrobulbar neuritis and conjunctivitis is also possible;
- skin lesion– erythema nodosum manifests itself as multiple nodes, most often on the extensor surface of the legs. The skin over the nodes has a purple-violet color, then becomes greenish, yellowish and then acquires a normal color. The development of gangrenous pyoderma (in severe septic disease), skin ulcerations, and focal dermatitis is possible. Gangrenous pyoderma is especially difficult;
- damage to the liver and extrahepatic bile ducts are of great importance for assessing the course of the disease, treatment tactics and prognosis. The following forms of liver damage are observed: fatty degeneration, portal fibrosis, chronic active hepatitis, cirrhosis of the liver. According to various researchers, liver lesions practically do not change under the influence of conservative therapy for CIBD, but in severe forms they progress and lead to the development of liver cirrhosis. A characteristic lesion of the extrahepatic bile ducts is primary sclerosing cholangitis, which occurs more often in patients with UC (approximately 50 to 90%);
- pancreas: Currently, the relationship of acute pancreatitis, antibodies to exocrine pancreatic tissue to the true extraintestinal symptoms of CIBD remains a subject of debate;
- damage to the oral mucosa characterized by the development of aphthous stomatitis, gingivitis, glossitis; possible ulcerative stomatitis;
- autoimmune thyroiditis;
- autoimmune hemolytic anemia.
It should be emphasized that all extraintestinal manifestations regress after adequate treatment. The exceptions are: ankylosing spondylitis and diseases of the hepatobiliary system.
Complications of CIBD
Complications of chronic inflammatory bowel disease include:
Colon perforation
Toxic dilatation of the colon
Intestinal bleeding
Colon strictures
Colon cancer.
Irritable bowel syndrome is a functional gastrointestinal disorder related to the intestines and accompanied by symptoms of abdominal pain and/or impaired bowel movements and/or abdominal distension.
Etiology and pathogenesis of IBS have not yet been sufficiently studied.
Currently, a large place in the development of IBS is given to neuropsychic factors. The relationship between the emotional sphere of a person and the functional state of the intestines has been known for a long time. Numerous studies on this issue convincingly prove that patients suffering from IBS are significantly more likely to have psychological disorders compared to the rest of the population. Disorders such as depression, anxiety, hypochondriacal conditions, and fear of closed spaces are observed in 70% of IBS individuals who seek medical help. Such patients are described as “lifelong restless.” Stressful life events (changes in social conditions, marital status, etc.) can also play an important role in the development of the disease in patients with IBS.
Among the pathogenetic factors in the development of IBS, an important role is played by disorders of intestinal motor function. In patients with IBS, disturbances in the basal motor function of the intestine, its disorders after meals and in response to emotional stress, and disturbances in the myoelectric activity of the muscle fibers of the colon are found. Increased contractile activity of the muscle layer of the intestinal wall is currently considered the main cause of pain in patients with IBS.
Of particular importance in the development of IBS is nature of the diet. Currently, the diet of the population of industrialized countries has significantly reduced the content of ballast substances - dietary fiber. Dietary fiber reduces the passage time of contents in the lower intestines, normalizes intraintestinal pressure, increases the mass of potassium, water content, and the excretion of bile acids. The exclusion or reduction of such a wide range of effects of dietary fiber on intestinal function in a low-residue diet causes a disorder in the coordination of its function.
May play a role in the development of IBS previous acute intestinal infections (“post-infectious IBS”).
According to the Rome III criteria, approved in 2006, diagnostic criteriaWITHRK are recurrent abdominal pain or discomfort on at least 3 days per month over the past 3 months associated with two or more of the following:
Improvement after defecation;
Onset is associated with a change in stool frequency;
The onset is associated with a change in the shape of the stool.
Additional symptoms are:
Pathological stool frequency (<3 раз в неделю или >3 times a day);
Abnormal stool shape (lumpy/hard stool or loose/watery stool;
Straining during defecation;
Urgency or feeling of incomplete evacuation, mucus and bloating.
These criteria must be present within the last 3 months with the onset of symptoms at least 6 months prior.
Classification of IBS
According to the criteria of the III revision, the classification of IBS is based on the predominant characteristics of the stool, for which the Bristol Stool Form Scale is used. In accordance with it, 4 types of IBS are distinguished:
1) with a predominance of constipation (IBS-C) - hard or lumpy stools in more than 25% of bowel movements and loose or watery stools in less than 25% of bowel movements; 2) with a predominance of diarrhea (IBS-D) - loose or watery stools in more than 25% and hard or lumpy stools in less than 25% of bowel movements; 3) mixed (IBS-M) – hard or lumpy stools in more than 25% and loose or watery stools in more than 25% of bowel movements; 4) unclassifiable (IBS-U) - pathological stool consistency that meets the criteria of IBSC, D or M. Since different symptoms may predominate at certain moments (over time, constipation gives way to diarrhea, and vice versa), experts suggest using the term “intermittent IBS” ( IBS-A). The absence of a disease substrate distinguishes IBS from other gastrointestinal diseases, so the diagnosis of IBS is a diagnosis of exclusion.
One of the main differential diagnostic differences of IBS is the absence of symptoms at night.
When examining patients, special attention should be paid to signs that can reliably exclude the diagnosis of IBS. Such signs are "alarm" symptoms or "red flags" of IBS, directly or indirectly indicating the possibility of an organic disease. These include:
The appearance of the first symptoms of IBS in old age;
Family history of colon cancer and inflammatory bowel disease;
Fever;
An admixture of fresh blood in the stool;
The occurrence of intestinal disorders at night;
Loss of body weight;
Leukocytosis;
Increase in ESR;
Steatorrhea and polyfecalia;
Pathological changes during an objective examination of the patient (hepatomegaly, splenomegaly, etc.).
Extraintestinal manifestations of IBS:
Non-gastroenterological symptoms (headaches, feeling of a lump when swallowing, dissatisfaction with inhalation, discomfort in the heart, chilly fingers, etc.);
- symptoms of combined gastrointestinal pathology;
Psychoneurological disorders (depression, anxiety syndrome, phobias, hysteria, panic attacks, hypochondria);
Diagnostics
IBD should be suspected in all cases of diarrhea (especially bloody), prolonged sepsis and abdominal pain. There is also an atypical clinical picture: for example, fever in the absence of intestinal symptoms, or in combination with extraintestinal manifestations (arthritis or liver damage), which precede intestinal ones or push them into the background.
The most informative methods for diagnosing chronic inflammatory bowel diseases are colonoscopy with biopsy and subsequent histological examination of the biopsy and x-ray examination of the colon (irrigoscopy).
At endoscopic examination colon with UC the following signs are found:
Swelling of the mucous membrane;
Hyperemia;
Easy bleeding;
Erosions or ulcers covered with fibrin, mucus, pus.
At morphological study The presence of inflammatory infiltrates is detected only within the mucous membrane and submucosal layer. In the early stage and period of exacerbation of ulcerative colitis, lymphocytes predominate in the inflammatory infiltrate; in the long-term course, plasma cells and eosinophils predominate.
Endoscopic picture at BC next:
Swelling of the submucosal layer;
Lack of vascular pattern;
Small aphthous ulcers followed by the formation of deep slit-like cracks, changing the relief of the mucous membrane like a “cobblestone street” (areas of preserved mucosa alternate with deep slit-like ulcers penetrating into the submucosal and muscular layers);
Strictures and fistulas.
On histological examination biopsy for CD reveals sarcoid-like granulomas in the submucosal layer (in 30-60%), with giant epithelioid cells; the inflammatory cell infiltrate is represented by lymphocytes, plasma cells, histiocytes, and eosinophils.
X-ray examination plays an important role in the diagnosis of CIBD. At UC by using irrigoscopy reveal:
Changes in the relief (graininess) of the mucous membrane of the colon;
Lack of haustration;
Bowel rigidity;
Uniform narrowing and shortening of the intestine, the intestine takes on the appearance of a “water pipe”
Characteristic radiological signs BC are:
Segmentation of intestinal lesions;
The presence of normal sections of intestine between the affected segments;
Uneven bowel contour;
Longitudinal ulcers and a relief of the mucous membrane, reminiscent of a “cobblestone street”;
Narrowing of the affected areas of the intestine in the form of a “cord”.
The basis for diagnosing IBS is a detailed history and identification of characteristic symptoms, physical and laboratory-instrumental examination. A general blood test and biochemical tests are without significant changes; radiography (irrigoscopy) reveals signs of dyskinesia, uneven filling and emptying, alternation of spastically contracted and dilated sections of the intestine. Sigmoidoscopy and colonoscopy with biopsy are a mandatory research method, as they allow us to exclude organic pathology. These studies usually do not reveal any significant pathological changes, but accumulations of mucus and a tendency to intestinal spasms are often detected. Histological examination reveals a normal histological picture of biopsy samples of the colon mucosa.
Differential diagnosis
Differential diagnosis of acute IBD is carried out with colitis of an infectious nature, occurring with diarrhea mixed with blood, which include amoebiasis, dysentery, salmonellosis, yersiniosis. To exclude these diseases, serological tests are performed to identify the pathogen. IBD should also be differentiated from colon neoplasms, which can be diagnosed using irrigoscopy followed by endoscopic biopsy.
The cause of pseudomembranous colitis is the necrolytic toxin of Clostridium difficile, which multiplies in the intestines under certain conditions. Most often, this disease occurs when treated with antibiotics, which apparently promote the proliferation of the pathogen by inhibiting the normal intestinal microflora. The most reliable differential diagnostic sign is the detection of Clostridium difficile toxin in the stool. Abdominal pain and blood in the stool (especially in the elderly) can be manifestations of ischemic colitis. This disease can be the most difficult to differentiate from IBD, especially CD. Angiography of the mesenteric arteries is used for diagnosis.
Once IBD is diagnosed, a differential diagnosis between UC and CD must be made. The main distinguishing features of these diseases are presented in Table 2.
|
Signs | ||
|
Clinical: Bloody diarrhea Tumor-like formations in the abdominal cavity Perianal localization |
Very rarely Can not be | |
|
Sigmoidoscopy: No proctitis | ||
|
Histology: Spreading Cellular infiltrates Granulomas |
Mucous Polymorphonuclear None |
Transmural Lymphocytic Have diagnostic value |
|
X-ray: Spreading Symmetry Stricture |
Expressed Superficial Very rarely |
Localized Absent Deep |
Table 2. Differential diagnosis of UC and CD.
Treatment
|
Direction of treatment |
Methods, drugs |
Indications |
|
Anti-inflammatory therapy: 5-ASA drugs glucocorticoids topical corticosteroids |
Sulfasalazine, mesalazine up to 4 g/day Prednisolone 40-60 mg/day Budesonide up to 9 mg/day |
Mild to moderate severity, exacerbation Severe course Moderate and severe exacerbation, as an alternative to systemic corticosteroids |
|
Immunosuppressants |
Azathioprine 2 mg/kg Methotrexate Cisclosporin A |
Steroid resistance, severe and fulminant course, complications of IBD |
|
Monoclonal antibodies to TNF-α |
Infliximab Adalimumab |
Steroid resistance, complications |
|
Antibiotics |
Ciprofloxacin Imipinem |
Fever, clinical symptoms of sepsis |
|
Correction of anemia |
Blood transfusions, iron supplements |
Iron-deficiency anemia |
|
Surgical methods |
Resection Stricturoplasty |
Complications of IBD |
Treatment of IBS
|
Direction of treatment |
Methods, drugs |
Indications |
|
Psychotropic drugs |
Fluoxetine (Prozac) Tianeptine (Coaxil) |
Extraintestinal complaints of IBS, including manifestations of depression |
|
Laxatives |
Lactulose (Duphalac) orally 20-60 ml/day Macrogol (forlax) orally 10-20 g/day Mucofalk 2-3 sachets per day |
IBS with constipation predominance |
|
Selective 5-HT4 receptor agonist |
Tegaserod orally 2-6 mg twice a day |
IBS with constipation predominance |
|
Antispasmodic drugs |
Buscopan 10-20 mg Duspatalin 200 mg Dicetel 100 mg 2 times a day Trimebutine (trimedate) 100 mg 3 times a day |
IBS with predominant abdominal pain |
|
Antidiarrheals |
Loperamide (imodium) average 4 mg/day Smecta 1 sachet |
IBS with diarrhea predominance |
|
Probiotics |
Bifiform 1-2 caps. 2 rubles/day Linex 1-2 caps. 3 rubles/day |
IBS with diarrhea predominance |
What is IBD? How can you help children and adults suffering from IBD? Answers to these most important questions for our readers today will be given by one of the leading domestic specialists in the field of IBD, an expert of the Moscow Department of Health in pediatric gastroenterology, a member of the Russian group for the study of IBD, the organizer of the annual conferences “Kanshin Readings” dedicated to IBD in children, a leading pediatric gastroenterologist at GMS Clinic, Doctor of Medical Sciences Elmira Ibragimovna Alieva.
Elmira Ibragimovna, good afternoon! Tell us about IBD. What does this pathology refer to and what kind of diagnosis is it?
Inflammatory bowel diseases (IBD) are a group of chronic inflammatory progressive diseases of the gastrointestinal tract. These include Crohn's disease and ulcerative colitis. Crohn's disease can affect any part of the gastrointestinal tract from the mouth to the anus.
Ulcerative colitis affects the mucous membrane of the colon, on which bleeding ulcers appear due to the inflammatory process.
How easy is it to distinguish IBD from such a common disease of civilization as irritable bowel syndrome (IBS) and various intestinal dysbiosis?
IBS can have symptoms similar to IBD, especially in older children. But there are warning signs, sometimes called “red flag” symptoms, that make you think you have IBD. These symptoms include:
- unmotivated weight loss;
- the appearance of symptoms at night;
- constant, intense abdominal pain;
- presence of fever;
- the presence of blood in the stool;
- changes in tests (inflammatory syndrome, anemia, etc.).
Therefore, invasive diagnostic studies (gastroscopy and colonoscopy) in children are an important step in the diagnosis of IBD. What symptoms (intestinal and extraintestinal) suggest IBD? Intestinal symptoms of IBD include:
- stomach ache;
- diarrhea;
- the presence of blood, mucus, pus in the stool.
To extraintestinal:
- joint damage;
- aphthous stomatitis;
- growth retardation, etc.
With ulcerative colitis, given that the mucous membrane of the colon is affected, intestinal symptoms are usually present. With Crohn's disease, the picture depends on which area is affected, and diagnosis can be complicated.
- What research needs to be done to be absolutely sure of the presence of IBD?
The examination should always be comprehensive in order to identify the prevalence of the process, extraintestinal manifestations and complications. For ulcerative colitis, in addition to general laboratory tests and ultrasound, colonoscopy with scalene biopsy is very important.
In case of Crohn's disease, in addition to endoscopic examinations (colonoscopy and esophagogastroscopy), additional x-ray examinations, including CT (computed tomography) or MRI (magnetic resonance imaging), are required to clarify the extent of the inflammatory process.
What are the causes of IBD? Why does IBD most often affect not children in the first years of life, but mainly adolescents? And why has IBD started to become steadily “younger” in recent years?
The cause of these diseases is not clear. No theory that explains the development of these diseases has been successful. But one thing is clear: IBD is an abnormal immune response of the body to some trigger (infection, stress, etc.). Very often it is not possible to isolate this moment of the disease, since it appears gradually and develops gradually. Genetic predisposition to diseases (IBD in parents) is of great importance. Therefore, if we keep in mind the most powerful theory - the immunogenetic one, then it becomes clear why diseases are more common in adolescents.
In young children, the immune status is just developing, and internal malfunctions of the body and the external environment have not yet had time to leave their “imprints.” But recently, more and more often, diseases are diagnosed in children under 5 years of age, and I want to note that they have a persistent, severe course. It should also be borne in mind that in children at an early age, IBD, especially Crohn's disease, may go undiagnosed for a long time. In recent years, the diagnosis of IBD has improved, which has directly affected the incidence of the disease.
As you know, IBD can be treated, but complete cure is usually impossible. What features in a child’s diet, behavior, and lifestyle will allow him to experience exacerbations of IBD as rarely as possible?
With ulcerative colitis, cure is possible only after complete removal of the colon (but this also has its moments), and it is impossible to cure a patient with Crohn's disease. Our goal is long-term remission, which allows the child to lead a normal life. Diet restrictions are required during an exacerbation of the disease, including limited physical activity. If the patient has a good effect from therapy, he continues to take medications (maintenance therapy) to avoid exacerbations of the disease. An interesting fact: among IBD patients there are a lot of gifted children.
What is the prognosis for patients with IBD? Is surgical treatment always necessary and what determines the success of treatment in such patients?
The prognosis depends on the course of the disease, on the response to drug therapy (there are often resistant forms), on the frequency of exacerbations, and on complications of IBD. The need for surgical treatment often occurs with Crohn's disease. The emergence of new drugs (genetic engineering or biological therapy) has significantly changed the course of IBD and reduced the frequency of surgical treatment. Success undoubtedly depends on the time of diagnosis of the disease. Late diagnosis is associated with serious complications and, naturally, increases the frequency of surgical interventions.
Chronic inflammatory bowel disease is considered to be any long-term enteritis - both infectious and immunoallergic etiology, which leads to a chronic inflammatory process in the intestine.
In addition to celiac disease, these diseases include ulcerative rectocolitis, Crohn's disease and other rarer diseases: colitis in Behçet's disease, necrotizing enterocolitis in young children. All these diseases are characterized by:
— unknown etiology (except celiac disease);
- inflammatory nature of the lesions;
— chronic course and possible relapses;
- association with other non-intestinal diseases;
- good response to corticosteroid therapy;
— the possibility of surgical resolution (treatment).
- Epidemiology
Both geographical (more common in Northern Europe) and genetic factors play an important role in the occurrence of these diseases.
Crohn's disease is more common in Western countries and among urban populations.
- Etiology and pathogenesis
The etiology is unknown, we can only assume the influence of infectious diseases and nutrition. The pathogenesis is associated with a violation of the immune response from the intestinal mucosa, the nature of which is not well understood; it is only known that T- and B-lymphocytes are activated, and the production of cytokines and complement increases.
- Pathological anatomy
Histopathological observations reveal two main and many intermediate types of disorders in chronic intestinal inflammation.
Crohn's disease. It is characterized by clearly demarcated transmural segmental lesions, separated from each other by externally unchanged mucosa. The lesion spreads to the mesenteric lymph nodes. Any part of the gastrointestinal tract can be affected, but the intestinal ileum is most often affected. The formation of stenoses, abscesses and fistulas is typical. Characterized by swelling of the mucous membrane, ulceration, atrophy and thickening of the intestinal wall, hyperplasia of the lymph nodes.
Granulomatous lesions are observed. In 60-70% of cases, granuloma is detected on surgical material and only in 30-40% during biopsy. Granuloma consists of epithelioid and giant cells. Despite the tendency towards necrosis, caseous necrosis is not observed. Ulcers and fistulas form easily.
Ulcerative rectocolitis. This is a disease of the colon. Starts at the rectal level and spreads upward. The process is superficial, affecting the submucosa, mucosa and rarely deeper layers. The acute stage is characterized by mucosal hyperemia, swelling, easily bleeding erosions and ulcers. In the intervals between ulcerative lesions, the mucous membrane is hypertrophied, and pseudopolyps are often formed. The described lesions can be combined with perianal fissures. Histologically, the formation of crypts and abscesses is characteristic, in which lymphocytes, eosinophils, neutrophils, and plasma cells accumulate. Granulomatous tissue is absent.
Variations of the two main types of chronic inflammatory bowel disease described above are:
1.
Ulcerative enterocolitis. Some authors consider it a congenital form of Crohn's disease. Lesions affect the entire digestive tract but are predominantly located in the terminal ileum and the initial colon.
2.
Behcet's syndrome, in which intestinal lesions are accompanied by retinitis, blindness, painful ulcerative and necrotic lesions of the oral and genital mucosa.
3.
Necrotizing enterocolitis in infants is often fatal. Clinical manifestations of the disease occur in the first week of life: diarrhea mixed with blood, signs of peritonitis and shock. Multiple ulcerative lesions with perforation are characteristic.
- Clinic
Classically, chronic intestinal diseases are characterized by both gastrointestinal (diarrhea, abdominal pain, blood in the stool) and general (fever, weight loss, delayed physical development) symptoms.
Crohn's disease: against the background of anorexia, typical of this disease, general symptoms predominate. Abdominal pain resembles attacks of appendicitis. Blood in stool is rarely found. On examination, tenderness is noted in the right iliac region, and a mass is sometimes palpated there.
Ulcerative rectocolitis: intestinal symptoms predominate - tenesmus, diarrhea mixed with blood. When palpating the abdomen, pain is noted along the colon.
- Complications
Stenoses, abscesses and fistulas, fissures, megacolon, perforations with massive bleeding, colon carcinoma, protein-losing enteropathy. Common complications such as inflammation of the iris, choroid, aphthous stomatitis, arthritis, pericholangitis, sclerosing cholangitis are typical.
- Diagnosis
Chronic diarrhea with abdominal pain, feces mixed with blood suggest chronic inflammatory bowel disease.
To confirm the diagnosis, it is necessary to evaluate laboratory test data: general blood test; sideremia; transferinemia; immunoglobulins; blood clotting time; blood levels of calcium, phosphorus, zinc, copper; bone age; C-reactive protein, a1-antitrypsin; stool analysis. Contrast radiography with barium has acquired a particularly important role in making the diagnosis. Double-contrast radiography is widely used, which notes:
- reduction of the lumen of the intestinal wall;
— heterogeneity of the pattern;
- cyst-like areas.
The presence of these three signs in the terminal ileum forms the Bodart triad, typical of Crohn's disease.
The spread of the inflammatory process can be judged by areas filled with leukocytes labeled with radioactive iodine I111. Computed tomography is indispensable for identifying complications (fistulas, abscesses).
The final diagnosis is made based on a biopsy.
Differential diagnosis is carried out with
- allergic colitis;
- nodular lymphoid hyperplasia;
— chronic granulomatous disease;
- appendicitis;
- polyposis and intestinal lymphoma;
- Schonlein-Henoch disease.
- Forecast
Has improved significantly in recent years. Child mortality has practically disappeared (from 15 to 2%).
Ulcerative rectocolitis has a greater tendency to relapse. Supervision of children consists of
— growth control;
— monitoring indicators of the inflammatory process;
- for therapy.
- Treatment
Dietary therapy plays an important role, especially in Crohn's disease, which is characterized by weight loss and growth retardation.
A new approach to therapy is the ability to achieve remission using a diet without hormonal therapy.
Pharmacotherapy is based on the use of corticosteroids, sulfasalazine, salazopyrine, metronidazole. Immunosuppressants are of little use due to their toxicity.
Surgical treatment is possible for severe complications (megacolon, stenoses, abscesses, fistulas) and in cases of growth retardation in the pubertal and prepubertal periods.
From clinical practice |
Liver damage, although without obvious clinical manifestations, is quite common in chronic intestinal diseases. In adults, pericholangitis with the portal triad develops in 70% of cases. 50% have fatty liver changes. 10% acquire liver disease. Liver cirrhosis develops in 5%. Other, more severe and rare complications are chronic active hepatitis, sclerosing cholangitis and biliary tract carcinoma. It should be noted that in children, chronic active hepatitis is a common complication, while pericholangitis and sclerosing cholangitis are very rare and are asymptomatic. We present a clinical case of ulcerative colitis in a three-year-old girl. The initial phase of the disease was asymptomatic. Subsequently, pronounced hepatomegaly developed. The girl was hospitalized at the age of three. 8 months before hospitalization, irritability, loss of appetite, intermittent abdominal pain, and stool mixed with scarlet blood were noted. With the symptoms described above, the girl was hospitalized. On examination, significant hepatomegaly was noted (+4 cm from below the costal arch along the right midclavicular line). In the blood test, ESR is 104 mm per hour; total blood protein 9.9 g%; albumin 2.5 g%; a1-globulin 0.3; a2-globulin 1.1; b-globulin 1.0; g-globulin 5.0; IgG 4810 mg%; alkaline phosphatase 1273 IU; Antinuclear and anti-smooth muscle antibodies are absent. During hospitalization, the girl complained of frequent abdominal pain. There is an admixture of mucus and scarlet blood in the stool. Analysis of stool mucus revealed many neutrophilic leukocytes. Endoscopically revealed an extensive inflammatory process throughout the colon with swelling of the mucous membrane. Upon contact with the instrument, the mucous membrane bled easily. With multiple biopsies, histological analysis was performed, which revealed thinning of the glandular ducts with mono- and polynuclear infiltration. Percutaneous liver biopsy revealed inflammatory and granulomatous changes predominantly in the portobiliary spaces. Moreover, an inflammatory process such as pericholangitis and initial cholangitis in the interlobular ducts was noted. Initial treatment with prednisone and subsequent salazopyridine (SAZP) resulted in complete remission of intestinal symptoms. Clinical remission with complete regression of hepatomegaly (the liver was palpated at the costal arch) was confirmed histologically. Laboratory parameters were also normalized (IgG 997 mg%). It is known that ulcerative colitis is often accompanied by intolerance to cow's milk protein, so a skin test and a test to determine specific IgE were performed. IgE levels were significantly increased. Rapid clinical remission was due to two factors: the administration of salazopyridine (SAZP) and the simultaneous exclusion of cow's milk from the diet. |
Literature
1.
Walker Smith J., Crohn's Disease. In: Diseases of the small intestin in children. 1989.
2.
Booth I. W. Chronic inflammatory bowel disease // Arch. Dis. Chid. 1991; 66:742.
3.
Elewaut D., De Keyser F., Culvelier C., Lazarovits A. I., Mielants H., Verbruggen G., Sas S., Devos M., Veys E. M. Distinctive activated cellular subset in colon from patients with Chron’s disease and ulcerative colitis 1998.
4.
Casini-Raggi V., Kam L., Chong Y. J. F., Fiocci C., Pizarro T. T., Cominelli F. Mucosal imbalance of IL-1 and IL-1 receptor antagonist in inflammatory bowel disease. A novel mechanism of chronic intestinal inflammation // J. Immunol. 1995; 154: 2434-2440.
5.
Olafsdottir E. J., Fluge G. and Hanf K. Chronic inflammatory bowel disease in children in Western Norway // J. Ped. Gastroen. North. 1989; 8:454.
6.
Castro M., Ansaldi N., Bianchi E. et al. Malattie inflammatorie chroniche intestinali: studio multicentrico italiano // Riv. Ital. Ped. 1991; 17:137.
7.
Blaser M. J., Miller R. A., Singleton J. W: Patients with active CD have elevated serum antibodies of seven enteric bacterial pathogens // Gastroenterology 1984; 87: 88-95.
8.
Shanahan F., Duerr R., Rotter J. et al.: Neuthrophil autoantibodies in ulcerative colitis: familial aggregation and genetic heterogenety // Gastroenterology. 1992;103:456-461.
9.
Halstensen T., Mollnes T., Garred et al. Surface epithelial related activation of complement differs un Crohn’s disease and ulcerative colitis // Gut. 1992; 33: 902-908.
10.
McNeish A. S. La diagnosi e la terapia della m. Di Crohn in eta pediatrica // Prospettive in Pediatria. 1988; 71:245.
11.
Shurmann G., Bretzler M., Meuer S. et al. Soluble IL-2r, IL-6 and IL-1 beta in patients with CD and US: preoperative levels and postoperative changes in serum concentrations // Digestion. 1991; 51: 51-59.
12.
Sciumert R., Towner J., Zipser R.: Role of eicosanoids in human and experimental colitis // Dis. Sci. 1988; 33: 58-64.
13.
McLain B.I., Diridson P.N., Stokes K.B. et al. Growth after gut resection for Crohn disease // Arch. Dis. Child. 1990; 65:760.
14.
Davies G., Evans C. M., Shand W. S., Walker Smith J. Surgery for Crohn’s disease in childhood: influence of sites of disease and operative procedure on outcome // Br. J. Surg. 1990; 77:91.
15.
Booth I. W. The nutritional concequences of gastrointestinal disease in adolescence // Acta Pediatr. Scand. Suppl. 1991; 373:91.
16.
Layden T., Rosenberg J., Neuncharnsky B. Reversal of growth arrest in adolescents with Chron’s disease after parental alimentation // Gastroenterology. 1979; 70:101.
17.
Hunter J. O. Nutritional factors in inflammatory bowel disease.
18.
Morin C. L., Rulet M., Roy C. C., Webwn A. Contnous elemrntal enteral alimentation in children with Crohn’s disease and growth failure // Gastroenterology. 1980; 79: 1205. Belli D. C., Seiduman E., Bouthiller L. et al. Chronic intermittent elemental diet improves growth failure in children with Crohn’s disease // Gastroenterology. 1989; 97:905.
19.
Aiges H., Mancovitz J., Rma J. et al. Home nactural sullplemental naso-gastric feedings in growth retarded adolescents with Crohn’s disease // Gastroenterology. 1989; 97:905.
20.
Sanderson I. L., Udeen S., Davies P. S. W. et al. Remission induced by elemental diet in small bowel Crohn disease // Arch. Dis. Child. 1987; 62, 1223.
21.
Giaffer M. N., Nath G., Holdsworth C. P. Controlled trial of Polvmenic versus elemental diet in the treatment of active Crohn’s disease // Lancet. 1990; 335:816.
22.
Seidman E., Leleiko N., Ament M. et al. Nutritional issues in pediatric inflammatory bowel disease // J. Ped. Gastroenterol. Nutr. 1991; 12:424.
23.
O’Sullivan M. A, O’Mora C. A. Nutritional therapy in Crohn’s disease. 1998.
24.
Zoli G., Care M., Parazza M., Spano C., Biagi P. L., Bernardi M., Gasbarrini G. A randomized controlled study comparing elemental diet and steroid treatment in Crohn’s disease. 1997.
25.
Malchow H., Ewe K., Brandes J. W., Coebell H., Ehms H., Sommer H., Jesdinsky H. European cooperative Crohn’s disease study (ECCDS): results of drug treatment // Gastroenterology. 1984; 86: 249-266.
26.
Prantera C., Pallone F., Brunetti G., Cottone M., Meglioli M. The Italian IBD study group: Oral 5-Aminoswlieye acid (Asacol) in the maintenance treatment of Crohn’s disease // Gastroenterology. 1992; 103: 363-368.
27.
Steinhart A. H., Hemphill D. J., Greenberg G. R. Sulphasalazine and mesalazine for the maintenance therapy for Crohn’s disease. A meta-analysis. D.D.W. Abstract Book. 1994. A-2842.
28.
Tremaine W. J. Maintenance of remission in Crohn’s disease: is 5-fminosalicylic acid the answer? // Gastroenterology. 1992; 103: 697-704.
29.
Bernstein I. H., Frank M. S., Brandt L. G. et al.: Healing of perineal Crohn’s disease with metrondazolo // Gastroenterology. 1980; 79: 357-365.
30.
Markovitz J., Grancher K., Mandel F., Daum F. Immunosopressive therapy in pediatric inflammatory bowel disease: results of a survey of the North American Society of Pediatric Gastroenterology an Nutrition // A J. Gastroenterol. 1993; 88(1): 44-48.
31.
Lloyd-Still J. D. Azathioprine and the treatment of chronic inflammatory bowel disease // J. Pediatr. 1990; 117(5):732-735.
32.
Verhave M., Winter H. S., Grand R. J. Azathiopine in the treatment of children with inflammatory bowel disease // J. Pediatr. 1990; 117(5): 809-814.
33.
Feldman M., Achord J. M., Chang E. B. Cyclosporine in Crohn’s disease - low doses won’t do it // Gastroenterology. 1990; 98 (5): 1383-1384.
34.
Balfour R. B. Cyclosporine therapy for inflammatory bowel disease // N. Eng. J. Med. 1994; 330(26): 1897-1898.
35.
Sachar D. B. Cyclosporine treatment for inflammatory bowel disease. A Step Backward or a Leap forward? // N. Eng. Med. 1995; 321(13):894-896.
36.
Geagan B. G., Rochon J., Fedorac R. N., Irvine E. J., Wild G. et al. Metrotrexate for the treatment of Crohn’s disease // N. Eng. J. Med. 1995; 332(5):292-297.
37.
Martin L. W., Torres A. L., Fisher J. E., Alexandre F. The critical level for preservation of continuity in the ileo-anal anastomosis // JPS 1985; 20:664
Chronic inflammatory bowel diseases
E. Tsalikova, L. Principessa, F. Scalercio,V. Guidi, O. Bederti
Department of Pediatrics,
University of Rome "La Sapienza"
Summary
Chronic inflammatory bowel diseases are commonly believed to be present in the form of two diseases with aetiologies of unknown origin, Ulcerative Rectocolitis and Chron’s Disease, which are characterized by important inflammatory events affecting the normal structure of the intestinal wall, with a tendency to relapse.
Both diseases share a variety of common characteristics and are thus considered by many as one single clinical entity.
The common features are the following:
- unknown aetiology
- inflammatory aspect of the lesions
- chronicity of the course of disease, with possible relapses
- association with extra-intestinal symptoms
- good response to corticosteroid therapy
- recourse to surgery (for a limited number of cases).
The aforenamed two paradigmatic pictures constitute the essentials of a spectrum comprising an indefinite number of intermediate pictures, for example Behcet's Colitis, similar to Ulcerative Colitis but where ulcers can be found in the area of the mouth and the genitals, or Ulcerative Enterocolitis of the infant , thought to be a congenital form of Chron's Disease.
Both pictures display gastrointestinal symptoms such as diarrhoea, tenesmus and bloody stools, usually prevailing in Ulcerative Colitis, and are accompanied by general symptoms such as fever and weight loss, usually found in Chron’s Disease.
One of the recent and most interesting aspects of Chron’s disease is the possibility to induce remission as well as restoration of the patient’s growth by administration of an elementary diet. The administration of a hypercaloric diet has also proven useful in correcting growth speed and in reducing the need of steroids, which also play an important role in inducing disease remission.
In order to further maintain remission, the administration of salazopirina (sulfosalazina) and corresponding salacylates, as well as of immunosoppressors such as azathioprine and cyclosporins, have proven useful. The administration of metronidazolo is indicated in the case of perineal injuries only. The use of surgery should be limited to complications and, in the presence of failure to thrive, only if the lesions are well delimited.