Trichomonas disease in women symptoms. The first signs and treatment of Trichomonas in women
Trichomoniasis (syn. trichomoniasis) is an infection caused by protozoan microorganisms. Currently, there are 3 known types of pathogens that affect the genitourinary system, intestinal and oral cavities; Trichomoniasis in women is caused by Trichomonas genitalis.
The pathogen feeds on red blood cells and iron ions, often contributing to the appearance of anemia. Trichomonas also absorbs other microorganisms. Thus, when the gonorrhea pathogen is ingested, gonococci continue to live inside the trichonases and, after antibacterial treatment against gonorrhea, can cause a relapse of gonococcal infection.
What it is?
Trichomoniasis - infection organs of the human genitourinary system. The causative agent is Trichomonas vaginalis. The disease ranks first in prevalence among diseases of the genitourinary system. In addition, trichomoniasis holds primacy among sexually transmitted diseases. According to the World Health Organization (1999), 10% of the world's population suffers from trichomoniasis. The disease is registered annually in about 170 million people.
Causes of the disease
Trichomoniasis is one of the diseases that do not occur just like that. The reason for its occurrence is always clear: unprotected sexual contact with a carrier of the infection. The causative agent of the disease is contained in some fluids of the human body, primarily in sperm and vaginal secretions. Therefore, the main route of transmission is sexual.
The likelihood of contracting an infection through household means is unlikely. However, this possibility cannot be completely ruled out. The bacterium can remain viable for some time in a humid environment. This should be remembered when visiting the pool and sauna. The bathhouse is safe in this regard, since Trichomonas quickly dies in the heat.
Trichomoniasis is transmitted during pregnancy from mother to child, and infection can also occur at the time of birth. Most often, the disease is diagnosed in girls whose mothers were carriers of Trichomonas during pregnancy.
Symptoms and first signs
The incubation period for trichomoniasis ranges from 5 to 20 days. In some cases, the first manifestation of the disease becomes noticeable later. Before this, the disease can proceed without discomfort. The first signs of trichomoniasis can often appear only during menstruation. In addition, the symptoms may be similar to those of a fungal infection.
As a rule, the main symptoms of trichomoniasis in women (see photo) are identical to the signs of other sexually transmitted diseases, namely:
- itching, burning, pain syndrome in the vaginal area;
- discomfort in the genitourinary area;
- pain in the pelvic area, the intensity of which increases noticeably during sexual intercourse;
- the presence of vaginal foamy discharge of a whitish or yellow-green hue with a pungent odor.
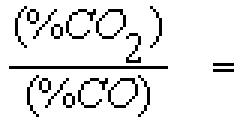
The structure of the secretions is determined in this case by the presence carbon dioxide, produced by Trichomonas. If there are similar signs of trichomoniasis, you must immediately contact a gynecologist or venereologist to determine the exact cause of the above-described phenomena.
An important point is that the course of trichomoniasis in women is often not detected due to the lack of characteristic symptoms. In order to detect infection in time, it is necessary to periodically visit a gynecologist. Especially with frequent changes of sexual partners.
What does trichomoniasis look like: photo
The photo below shows how the disease manifests itself in women.

[collapse]
Danger of the disease in pregnant women
In pregnant women, this protozoan can cause premature birth, abortion, and the birth of premature babies.
This happens because the altered microflora in the vagina of a pregnant woman destroys the lower membrane of the amniotic sac and leads to premature rupture of amniotic fluid. Trichomonas itself is not dangerous to the fetus, since it cannot penetrate the placental barrier, but it can become a transporter of other bacteria (chlamydia, gonococci, etc.) that will harm the unborn baby.
Infection of the fetus is possible when passing through the mother's birth canal. The likelihood of infection is higher in a female fetus due to the structural features of the genital organs (short urethra).
Consequences
The danger of this disease in non-pregnant women lies in unpleasant complications that cannot be corrected medically. So, the consequences of trichomoniasis in women can be the following:
- adhesions;
- female infertility;
- chronic inflammatory diseases of the genitourinary system (vaginitis, etc.).

Diagnostics
Diagnosis of the disease consists of bacterioscopic detection of Trichomonas vaginalis based on the results of Gram staining of smears. Moreover, in women, this method of identifying the disease gives more accurate results than men.
A more accurate diagnostic method in comparison with the bacterioscopic method is the bacteriological method. It is recommended in all cases of negative treatment results. In doubtful situations, methods are used that give the most accurate results - direct immunofluorescence (DIF), DNA diagnostics (PCR), and culture.
How to treat trichomoniasis in women?
Treatment of the infection is prescribed to both sexual partners, regardless of whether the man has signs or symptoms of trichomoniasis. First of all, you should avoid eating spicy food and alcohol for the period of treatment. It is also recommended to maintain sexual rest during therapy and until negative tests are obtained (to avoid reinfection).
Basic principles of treatment of trichomoniasis:
- Strengthening the body's immune defense;
- Treatment of trichomoniasis in both sexual partners at once;
- During treatment it is necessary to abstain from alcohol and sexual activity;
- Use of anti-trichomonas drugs;
- Normalization of vaginal microflora and restoration of its function;
- Carrying out general and local therapy at the same time, only local therapy (ointments, suppositories, etc.) will not give results.
For trichomoniasis, treatment in women with drugs is prescribed only by a doctor; self-medication is not allowed. Medicines must have an effect against anaerobic microorganisms. That is, agents from the 5-nitroimidazoles group are used. These include:
Treatment regimens for trichomoniasis are different:
- Trichopolum 0.5 g. (or metronidazole 0.25 g) 1 tablet twice a day (or 2 tablets 2 times a day), course duration is 7 - 10 days.
- Tinidazole 0.5 g. – single dose of 4 tablets.
- Fasizhin 150 mg twice a day for a week.
Treatment of the chronic stage of the disease is practically no different from the treatment of the acute stage. In addition to anti-trichomonas drugs, therapy involves taking adaptogens (aralia tincture, Eleutherococcus tincture, Aloe extract), vitamins and immunostimulating agents.
Control tests after suffering from trichomoniasis are taken three times after each menstruation for 3 months.

Prevention
In the prevention of this disease, a person’s lifestyle plays a huge role: nutrition, physical activity, daily routine, bad habits or addictions, how hygienic he is, ecology environment. Lead a healthy lifestyle, understand your sexual partners (who, by the way, should never have more than one) and be healthy!
Trichomoniasis is a unique disease in the full sense of the word. On the one hand, it occurs three times more often than syphilis, chlamydia and HIV. But, on the other hand, it often remains without due attention, both from doctors and from the patients themselves.
Often a woman undergoes long-term treatment for ureaplasmosis-mycoplasmosis, chlamydia, candidiasis, dysbacteriosis, or simply “leukocytosis in smears,” which exhausts her body and suppresses its defenses, but complaints about periodic unpleasant discharge that causes discomfort continue. When communicating with such a woman, information suddenly appears that trichomonas were sometimes found in smears, which either disappear or appear again. Has the woman's partner been tested? From the answers of many women, you learn that most often sexual partners remain aloof from any examinations. And, on the contrary, where it is not rational to examine a partner, he is sent for dozens of tests and given unreasonable treatment.
Trichomoniasis is a typical infection transmitted only through sexual contact, which means it is a minor venereal disease. If a person is diagnosed with Trichomonas and the diagnosis of trichomoniasis is confirmed correctly, it is necessary to understand that the infection occurred through sexual contact, so the sexual partner(s) must be examined and treated. Most cases of trichomoniasis in men are not diagnosed! Unprotected sexual relations should be stopped during the treatment period. Most often, both partners need treatment at the same time.
Prevalence of trichomoniasis
In the world, according to WHO, trichomoniasis affects 170-180 million people annually, which significantly exceeds the incidence of gonorrhea and chlamydia. In the USA, up to 10 million people are infected with Trichomonas, and in Europe – 11 million people. More than 150 million people are infected in developing countries. These figures may be significantly higher (according to other sources, more than 270 million people are infected in the world). In fact, this is the only sexually transmitted disease that is not subject to registration and reporting in the vast majority of countries in the world.
The prevalence of the disease depends on the socio-economic conditions of the population and the availability of timely, high-quality medical care, good hygiene, level of education of people. For example, in the United States, black residents are more often infected with trichomoniasis. Around the world, the incidence of trichomoniasis among adolescents is increasing because many of them are actively sex life.
Trichomonas infection occurs in 29-84% of women (depending on the region), and half of these women have no complaints or signs of the disease. Women who have casual sex suffer from trichomoniasis 3.5 times more often than women who have one sexual partner.
Regarding trichomoniasis in men, there are many gaps in the medical literature: trichomonas infection in men has hardly been studied. The last serious publications on this topic were about 50 years ago.
Trichomonas infection
To date, more than 50 varieties of Trichomonas are known. Three species of Trichomonas live in the human body (T. intestinalis, T. elongate, T. vaginalis). Many serious studies have been carried out on the possibility of causing Trichomonas infection by these representatives of protozoa, including on female volunteers. It turned out that only Trichomonas vaginalis can be the causative agent of trichomoniasis. The species of Trichomonas living freely in reservoirs has nothing to do with the disease trichomoniasis.
Can Trichomonas infection be transmitted through non-sexual contact? There is a lot of false and speculative information on this topic. Trichomonas quickly lose their viability outside the human body. These protozoa die instantly in a 2% soap solution and very quickly when dried. It is extremely rare (less than 1% of cases) that Trichomonas can be transmitted through contact of the genitals with the wet secretions of an infected person (using washcloths, wet towels, dirty linen).
The pathogen can be viable for 24 hours in urine, semen, water and wet underwear. If there is wet discharge from an infected person on the toilet seat, then it is theoretically possible for the pathogen to be transmitted to a healthy woman, but it is practically unlikely that the woman will not notice the discharge on the toilet seat.
Trichomoniasis is more common in men and women who have a large number of sexual partners. It is also more common in combination with other pathogens.
If a healthy man has contact with a woman with trichomoniasis, he has a 70% chance of contracting this infection. If a healthy woman has contact with a sick man, the risk of infection is 80-100%. No other sexually transmitted infection does not have such a high level of pathogen transmission. Considering that trichomoniasis occurs latently for several days ( incubation period in some cases it can last more than a month, but on average it is 4-28 days), then the risk of transmission of Trichomonas is extremely high. In men, trichomoniasis occurs without symptoms more often than in women, and this also needs to be remembered.
Signs of trichomoniasis
Up to 60% of women may have no signs of Trichomonas infection. Many women are carriers of trichomonas, which in combination with other microorganisms can lead to acute inflammation appendages after a certain period of time. Most often, women complain of copious amounts of gray-yellow (purulent), sometimes foamy, vaginal discharge, with unpleasant smell, as well as painful and frequent urination, itching and burning in the external genital area. In some cases, swelling of the labia, vaginal walls and cervix may be observed.
This infection often occurs in combination with gonorrhea and/or chlamydia (only in 10.5% of cases, trichomoniasis occurs as a monoinfection, that is, one harmful pathogen), which can lead to long-term inflammation of the pelvic organs and infertility.
In men, Trichomonas infection can cause inflammation in the urethra. In 50% of cases of all urethritis, Trichomonas is the only causative agent of this disease, which can result in the formation of adhesions in the urethra, which can subsequently lead to male infertility. Trichomoniasis is often associated with chronic prostatitis(20% of cases).
In pregnant women, trichomonas infection may be one of the risk factors for the development of premature birth and premature rupture membranes. Trichomoniasis is also associated with low birth weight babies. During childbirth, in some cases, trichomonas infection can be transmitted to the child.
Trichomoniasis and other infections
The connection between trichomoniasis and other dangerous sexually transmitted infections has been noticed for a long time. Trichomonas infection is known to double the risk of long-term (persistent) viral infections caused by the human papillomavirus (HPV). In women, HPV is associated with the development of precancerous conditions and cervical cancer, so it is safe to say that trichomoniasis increases the risk of developing these pathological conditions of the cervix. Self-cleansing of the body from HPV types, which are involved in the development of cervical cancer, in healthy women occurs within 1-2 years (in 90% of cases) - on average 180 days. In women with trichomoniasis, the body’s self-cleansing of HPV is extended by 2.5 times.
Women with Trichomonas infection are at twice the risk of contracting the herpes simplex virus (HSV) than healthy women.
There is reliable evidence that the presence of trichomoniasis increases the risk of HIV infection. It is important to understand that the degree of infection with sexually transmitted viral infections depends largely on the condition of the mucous membrane of the urogenital system. Healthy epithelial cells have a greater resistance to the viral agent, so people who do not have other sexually transmitted infections become infected with viral infections (HIV infection, hepatitis, herpes, etc.) not so often, despite sexual contact with a sick person. Conversely, the level of infection increases significantly if the mucous membranes are damaged, especially with the formation of ulcers, because ulcers are an open gate for any virus. Trichomonas lead to damage to epithelial cells, so the protective forces of the mucous membranes are sharply reduced. Trichomoniasis is called a cofactor in HIV transmission.
Diagnosis of trichomoniasis
Examination of a woman’s external genitalia, vagina and cervix is not reliable method diagnosis, although discharge in the presence of trichomoniasis has a specific unpleasant odor, foaminess, or may be abundant, greenish-purulent in color. In the chronic course of Trichomonas infection, changes occur in the mucous membranes of the cervix and vagina - pinpoint reddening of the epithelium occurs, which are small hemorrhages in the tissues of the squamous epithelium. Therefore, upon examination, the color of the cervix resembles strawberries (spot colpitis), which is called the “strawberry sign.”
In men, there are even fewer signs of trichomoniasis, so in addition to a physical examination, it is important to conduct a number of laboratory tests.
All diagnostic methods can be divided into three groups – old, new and newest. Each diagnostic method has its own advantages and disadvantages. These methods are evaluated in terms of sensitivity (fewer false negatives) and specificity (fewer false positives) in relation to the detection of an infectious pathogen. The table below shows the sensitivity and specificity of available methods for diagnosing trichomoniasis.
| Method name |
Time spending |
Sensitivity (%) |
Specificity (%) |
|
Old methods: |
|||
|
Native smear |
|||
|
Painted smear |
|||
|
Cytological smear |
|||
|
Liquid-based cytological smear |
|||
|
Cultivation on agar |
|||
|
New methods: |
|||
|
Cultivation in broth |
|||
|
Smell test |
|||
|
Latest methods: |
|||
|
Rapid antigen test |
|||
|
Several hours or days |
|||
|
Non-amplification VPIII test |
|||
|
Nucleic Acid Amplification Test (NAAT) |
Few hours |
||
|
Amplification test (TMA) |
Few hours |
||
Not all of these methods are used in post-Soviet laboratories.
The sensitivity of the test often depends on the material that was taken for analysis. Advantage must be given vaginal discharge and scraping in women, and discharge and scraping from the urethra in men.
A smear of the discharge using a potassium solution can help identify the foul (fishy) odor that may occur with trichomoniasis, but is used very rarely in modern practice.
Microscopic examination of secretions(fresh native smears and stained smears) allows you to detect Trichomonas, as well as the presence of a large number of altered lymphocytes. The more lymphocytes, the more pronounced the infectious process. Often with trichomoniasis other types of microorganisms are found - coccobacilli.
Cytological smears (Papanicolaou) or liquid cytological smears are a good diagnostic method. Quite often, laboratory doctors do not indicate the presence of Trichomonas, but in the conclusion they write: “Atypical epithelial cells have been identified. Rule out trichomonas infection." This is an excellent tip for the attending physician and should be taken into account.
If the test results are negative, Trichomonas can be detected using cultivation discharge from the urethra, vagina, prostate secretion and sperm. The cultural method is of great value for recognizing atypical forms for the purpose of diagnosing trichomoniasis and for monitoring treatment; it is also considered the “gold standard” of diagnosis.
Serological methods diagnostics are becoming very popular, but they should complement, and not replace, other methods for diagnosing trichomoniasis. Trichomonas have an extremely large number of proteins on the surface of the shell (antigens), so the determination of antibodies to them is more of an experimental diagnostic method than a reliable practical method.
Having such a wide choice in diagnosing trichomoniasis, most cases of this disease remain undiagnosed in people visiting medical institutions. Most of these institutions do not have clear examination algorithms. Typically, doctors send patients for several tests at once, or only for serological tests. Test results often contradict each other, doctors do not know how to interpret them, so some prescribe treatment at random, others do not prescribe anything at all, and still others ignore the examination and treatment of their partner.
Rational approach to diagnosing trichomoniasis
Progressive medicine is guided by the principle of rationality: how to accurately diagnose a disease with the least amount of time and money.
This principle takes into account not only the sensitivity and specificity of different diagnostic methods, but also the cost of each method, speed of implementation and necessarily safety for the person undergoing examination (the less invasive the test, that is, the less needles, systems, devices, drugs, etc. are introduced into the body .p, the safer the test).
For diagnosing trichomoniasis, there is also a rational examination algorithm that allows you to avoid unnecessary expenses (no matter from whose pocket), unnecessary errors in diagnosis, unnecessary stress for a person and unnecessary waste of time (someone else’s life too). Rules for a rational approach in diagnosing trichomoniasis
the following:
1. Physical examination of the patient (gynecological in women) and collection of material for research - a native (fresh or wet) smear from the vagina in women and from the urethra in men. Why a native smear, despite its low sensitivity? Because this is the cheapest diagnostic method, as well as the fastest: examination of the discharge under a microscope must be carried out in a matter of minutes. If trichomonas are detected in the native smear, additional examination is not necessary. Of course, it is necessary to take into account complaints and inspection results.
2. If the result of the native smear is negative, a rapid antigen detection test or one of the amplification tests can be performed. Such tests are more expensive, but the result can be obtained within 10-30 minutes or several hours (in some laboratories within several days). If the result is positive, treatment can be prescribed.
Using more diagnostic methods to diagnose trichomoniasis is not recommended.
Of course, each doctor may have his own principles for diagnosing trichomoniasis, but the hobby for reinsurance should not dominate the examination and treatment.
Treatment of trichomoniasis
Until 1960, when 5-nitroimidalol (metronidazole) came onto the market, treatment for trichomoniasis was more often unsuccessful than successful. A little later, other drugs from the group of 5-nitroimidazoles appeared on the market - ornidazole, tinidazole, secnidazole, which began to be used in the treatment of trichomonas infection.
Modern post-Soviet regimens include long-term use of tablet drugs metronidazole (Trichopol), and in very high doses. In addition to this drug, doctors prescribe another additional drug from the same group of nitroimidazoles, even the same metronidazole, but under a different name (from a different manufacturer). Plus antibiotics, antifungal drugs, a whole list of vitamins and dietary supplements, suppositories, baths, douching, “rinsing” the urethra, bladder, uterus and even microenemas. Most people cannot withstand such treatment regimens, because already on the second day of taking the medications, many experience nausea, vomiting, liver pain, indigestion, and many others. side effects. Women are more resilient than men, so they persistently “finish off” the prescribed course, only to then drag themselves into a months-long struggle with other emerging health problems.
It has been proven that the treatment of trichomoniasis has never required and does not require doubling, tripling, or multiple increases in both the dose and time of taking medications, or even a combination of any medications in general.
The most popular and fairly effective method of treating trichomonas infection for more than 30 years has been the use of metronidazole orally. Local treatment in the form of vaginal tablets and suppositories may be insufficient, since Trichomonas affects not only the vaginal mucosa, but also the Bartholin glands and urethra.
Numerous studies have shown that the use of a single dose of the drug has the same rate of complete cure as the use of other regimens (3-5-7 days of treatment), so doctors are increasingly using a loading dose of metronidazole to treat trichomoniasis. The impact single dose of metronidazole (Trichopol) is 2 grams - and no more. You can take 250 mg (1 tablet) of trichopolum twice a day for 5 days.
Many of our doctors do not know that if Trichomonas are sensitive to metronidazole, then 2 grams of the drug is quite enough for recovery. If trichomonas are not sensitive to metronidazole, then after prescribing even super-doses, there will be no effect in treatment, but the patient will experience many serious complications due to treatment. Therefore, such overreaction in the treatment of trichomoniasis is based on too outdated Soviet schemes.
Many infections in modern medicine are successfully treated with shocking single doses of drugs that are easily tolerated and are as effective as long-term courses of treatment, but have fewer side effects. Complete cure is observed in 90-95% of cases after using a single dose of metronidazole.
Within 48 hours after using metronidazole, a person should not drink alcohol due to the possible development of an antabuse (disulfiram, teturam) reaction, which manifests itself in the form of rapid heartbeat, malaise, nausea, and vomiting. Metronidazole also causes a feeling of dry mouth and often stains the urine like meat slop.
Relapses of trichomoniasis
Why doesn’t recovery occur in all people without exception? For the first time, resistance (resistance) of Trichomonas to metronidazole was discovered in 1962 - several years after the appearance of the drug. Long period of time alternative medicinal product there was no, the administration of large doses of metronidazole or repeated courses did not lead to recovery, and this caused doctors some fear and purely professional hostility towards this pathogen (just as many doctors now fight extremely aggressively with ureaplasma or chlamydia).
If the desired recovery does not occur, you need to answer several questions:
1. Has the sexual partner(s) been examined for the presence of trichomonas in his body?
2. Was the partner treated at the same time?
3. Was sexual activity limited during the treatment period and were preventive measures (condoms) used?
4. Does the patient have a resistant strain of trichomonas or is it re-infected from a partner(s)?
Resistance of trichomonas to metronidazole is not common. If it is suspected (from the moment of treatment until the moment of detection of trichomonas, the person has not had sexual intercourse again, for example), tinidazole is prescribed - a second-generation nitroimidazole, in the form of a single dose (2 grams). It is also effective in treating amoebiasis. Less commonly, repeated courses of metronidazole are prescribed, usually in a slightly higher dose and for 5-14 days.
People tend to hide important information from doctors when it comes to their intimate life, even if there is a serious danger to the person's health. In the transmission of sexually transmitted infections, a chain of relationships always occurs: pathogen-woman-pathogen-man-pathogen-woman-pathogen-male-pathogen, etc. Therefore, it is very important to interrupt this chain of transmission of the infectious agent in a timely manner. Relapses of trichomonas infection, like other sexually transmitted infections, are most often not a manifestation of ineffective treatment. The main reason for the appearance of repeated cases of trichomoniasis is the existence of the same strong chain of transmission of infection.
Treatment of trichomoniasis in pregnant women
There are now many contradictions regarding the treatment of pregnant women who are carriers of Trichomonas. Clinical studies in a number of major treatment centers around the world have shown that treatment of trichomoniasis with metronidazole does not reduce the incidence of preterm birth in women with asymptomatic trichomoniasis. Modern recommendations state that a pregnant woman, regardless of whether she has complaints and signs of trichomoniasis, should undergo treatment for this infection.
However, in 2001, a publication appeared in scientific and medical circles that claimed that women who were treated for trichomoniasis with metronidazole had a higher rate of preterm birth than those who were not treated. Therefore, other recommendations suggested the opposite: in pregnant women without complaints, there is no need to diagnose trichomoniasis.
A more detailed study of the American clinical study on which this article was published showed that doctors used 8 grams of metronidazole to treat trichomoniasis, when the standard safe dose for pregnant women is 2 grams, treatment was prescribed with a delay of 4 weeks after the diagnosis of trichomoniasis. usually in the second trimester of pregnancy. The study was not completed because doctors felt that using metronidazole to prevent preterm birth was ineffective and had side effects.
Most doctors are still of the opinion that trichomoniasis in a pregnant woman should be diagnosed and treated on time, because other factors must be taken into account Negative consequences trichomonas infection, primarily its relationship in the transmission of a number of serious sexually transmitted infections. Metronidazole is not a teratogen, that is, it does not cause developmental defects or embryo death. This is a completely safe drug and can be used if necessary in the first half of pregnancy.
Treatment of sexual partner
Should my male partner be treated if he has no signs of trichomonas infection? Correct answer: yes, the man should undergo examination and treatment immediately. During treatment, unprotected sexual intercourse should be avoided.
Taking into account the high cost and time of the examination, isn’t it easier for the sexual partner to simultaneously prescribe a loading dose of the medicine in absentia? Most doctors do this, although this contradicts the doctor’s duties not to prescribe treatment in absentia, but only after collecting complaints, examining and examining the person. And what often happens is this: a woman comes home after visiting the doctor and tells her man that he must take these pills because she is being treated for some kind of infection, and these are the treatment regimens. Whether the man takes these pills or not is unknown. He may not even ask about the name of the disease. Therefore, the seriousness of the diagnosis of trichomoniasis, which is a sexually transmitted disease, and not a cold or something else, is lost and is not properly perceived by sexual partners.
Monitoring the effectiveness of treatment
Many people are interested in the question of how to know that a person has recovered and is no longer contagious. As implausible as it may sound, trichomoniasis is a self-healing disease (like HPV infection and chlamydia). In people who are not treated, trichomoniasis usually lasts up to 4 months in men and up to 5 years in women. In women, trichomonas are found on average within 12 weeks. About one third of women will still seek help due to signs of trichomonas infection. In almost a third of women, trichomoniasis will resolve on its own without treatment. But even in such a semi-optimistic picture of getting rid of sexually transmitted infections, there are several “buts”.
Firstly, we can talk about possible self-healing only if the infected person has no sexual intercourse for a long period. Secondly, it is always important to remember that the healing process depends on the body’s defenses and a person’s lifestyle. Thirdly, in the presence of other sexually transmitted infections, spontaneous recovery is almost impossible. And fourthly, Trichomonas infection can be long-term or persistent in some cases. Therefore, it is always better to undergo treatment than to rely on the power and help of nature.
Resistance of trichomonas to metronidazole is observed in only 5% of people, but there are no clear recommendations when exactly it is necessary to undergo a follow-up examination. Most doctors suggest using PCR or TMA for control diagnosis two weeks after treatment, since a native smear and culture may be negative for several weeks or even months after treatment. This is explained by the fact that to isolate the culture, a certain concentration of trichomonas in the material is necessary, and after treatment the number of trichomonas can be significantly reduced. The number of trichomonas in a smear may also be low and therefore not noticed when viewed. Many doctors recommend performing PCR or TMA several times in a row over 3-6 months (once a month).
At the time of signs acute infection sexual intercourse is often accompanied by severe discomfort and pain, and is therefore not advisable until the inflammation subsides. Unprotected sexual intercourse, that is, without condoms, taking into account that the sexual partner is healthy, is recommended only after confirmation of complete recovery, usually no earlier than two weeks after completion of treatment (before receiving the results of a control test). Some doctors recommend using condoms for 3 to 6 weeks. Planning pregnancy during the period of treatment and recovery monitoring is not advisable.
How does trichomoniasis manifest itself and how to treat it in women?
Trichomoniasis in women is a global problem that can only be solved by increasing the popularity of condoms. This contraceptive is the only way to maintain health and reproductive function.
The frequency of infection with Trichomonas is higher than with the causative agents of gonorrhea and a number of other sexually transmitted diseases. Every year, the disease ranks 1-2 in terms of prevalence among diseases of the genitourinary system.
The disease does not manifest itself in all cases. A sluggish course with a minimum number of coming and going symptoms is more typical for the disease. A woman regards many signs of latent trichomoniasis as changes in the vaginal microflora and discharge before menstruation. This category includes:
- thicker discharge (compared to other days of the cycle);
- increased odor;
- nagging pain in the lower abdomen.
Some patients confuse trichomoniasis with inflammation of the kidneys and bladder. Signs characteristic of all these diseases:
- increased urge;
- a woman cannot hold back the process of urination for a long time;
- ailments typical of inflammatory processes in the body (short-term heat and swelling of the external genitalia are the first signs of trichomoniasis).
Important! After unprotected sexual intercourse with an untested partner, you should not wait for the first signs. It is necessary to undergo diagnostics even in their absence. The first time is examined a few days after sexual intercourse. In the second - in a month. In this way, it will be possible to detect the infection even with a long incubation period.
Other symptoms observed in women after infection:
- discomfort during bowel movements (with Trichomonas proctitis);
- sore throat (if Trichomonas has attacked the oral mucosa);
- problems with urination.
The last point implies many variants of manifestations. In some patients, pathology manifests itself as a change in the quality characteristics of urine. Others complain of burning, tingling, or shooting when emptying the bladder. Signs depend on concomitant diseases, stages of development of trichomoniasis, intimate life.
Treatment
Medication
 Therapy is based on 5-nitroimidazole derivatives. The substances have an antimicrobial effect and are characterized by quickly manifested bactericidal properties. Effective against all forms of inflammatory and purulent-inflammatory processes. Their use is advisable not only in the case of trichomoniasis, but also in the presence of several types of STDs in the body at once.
Therapy is based on 5-nitroimidazole derivatives. The substances have an antimicrobial effect and are characterized by quickly manifested bactericidal properties. Effective against all forms of inflammatory and purulent-inflammatory processes. Their use is advisable not only in the case of trichomoniasis, but also in the presence of several types of STDs in the body at once.
List of antimicrobial drugs:
- . Release form: tablets. Contraindicated in liver failure. The remedy is used with caution in case of diabetes mellitus and microcirculation disorders. The drug is incompatible with alcohol. Consequences of simultaneous use: copious discharge vomit, severe cramping pain in the abdominal area, hyperemia. It should not be used together with additional sources of lithium. Cost of packaging (6 tablets): 260-350 rubles.
- Metronidazole. A cheap antiprotozoal drug is available in the form of vaginal gel, tablets, vaginal suppositories, injection solution and intravaginal use. Prescribed separately and together with Amoxicillin. In many pharmacies it is sold only by prescription. On the Internet it is possible to purchase the drug without documents. For 10 tablets you will have to pay 7-30 rubles, for 10 candles - 50-60 rubles.
- Secnidazole. Sold only in tablet form. When taken in parallel with drugs containing disulfiram, it provokes the development of psychosis. The medication can be used in childhood. Price: 200-250 rub.
- Seknidox. Analogue of the previous medication. Cost of 2 tablets: 650-810 rub.
- Tinidazole. It ranks third in frequency of use (immediately after Metronidazole and Ornidazole). Use may lead to anorexia, dysarthria, and locomotor ataxia. Reduces psychomotor reactions. Not suitable for treating girls. Cost: 30-120 rub.
- Ornidazole. White-yellow film-coated tablets are sold along with solutions. It differs from analogues in safety: side effects occur less frequently.
- Nimorazole. Complete analogue of Naxojin.
Side effects from taking 5-nitroimidazole derivatives are of the same type. During the use of medications, the following may occur:
- changes in stool;
- metallic taste in the mouth;
- leukopenia (more often occurs in patients who have been diagnosed with hematopoietic pathologies);
- problems with coordination;
- rashes, itching;
- vomit;
- thrombophlebitis (only with intravenous administration).
When using medications, it should be taken into account that the presence of an allergy to 1 medication from the list guarantees an inadequate immune response to all other medications in the group. In addition, in women suffering from diseases of the central nervous system, antimicrobial tablets can cause an attack and deterioration of well-being.
Reception scheme
Key points:
- 3 days before the start of therapy, they resort to hepatoprotectors (Essentiale-forte, Karsil). Take 1 tablet in the morning and evening throughout the course of treatment.
- Instead of hepatoprotectors, you can use Immunal (1 tablet 3 times a day).
Use for acute forms (choose 1 drug, do not use all at once):
- Metronidazole, Nimorazole, Tinidazole, Secnidazole are taken once in a dosage of 2.0 g;
- Ornidazole is taken once (dose: 1.5 g).
Method of use for unclear clinical picture:
- Ornidazole: 0.5 g 2 times a day for 5 days;
- Tenonitrazole: 0.25-0.5 g every 12 hours for 4-7 days;
- Nimorazole: 0.5 g 2 times a day for 6 days.
Method of use for chronic, complicated, often worsening trichomoniasis:
- Secnidazole and Tinidazole are taken three times, 200 mg each (1 day should pass between doses);
- Ornidazole is taken 2 times a day, 500 mg for 10 days;
- Metronidazole is used 3 times a day for 12 days;
- Nimorazole is taken 500 mg every 12 hours for 12 days.
What else is used to treat trichomoniasis?

 Pelvic inflammatory diseases are successfully eliminated with new fluoroquinolones. These drugs can replace complex therapy for some genital tract infections.
Pelvic inflammatory diseases are successfully eliminated with new fluoroquinolones. These drugs can replace complex therapy for some genital tract infections.
Side effects from their use are limited to conditions and phenomena characteristic of the effects of drugs against trichomoniasis.
Undesirable manifestations from the central nervous system, hematopoietic and digestive systems, psyche, and skin are possible.
Group representatives:
- . Antibacterial drug effective against chronic trichomoniasis. Release form: tablets and solution for infusion. Dosage: 400 mg/day. Course duration: 1-3 weeks. Contraindications: tendon pathologies, lactose intolerance and congenital deficiency, excess transaminases, persistent liver dysfunction, childhood and adolescence. Toxicity to the fetus was detected. Avelox should not be used during pregnancy and breastfeeding.
- Moxifloxacin stada. The prescription medication is sold in the form of solutions for infusions and tablets. Features: effective in cases where other types of fluoroquinolones could not cope with the problem. Dosage regimen: 400 mg/day for 7 days. Treatment of trichomoniasis in elderly women with this medication should be carried out under the supervision of doctors. Reason: inflammation of the tendons may develop; adjustment of the dosage regimen is required.
- Norfloxacin. These tablets differ from their analogues in their ability to be used in the treatment of teenage girls (from the age of 15). The medication is not prescribed during pregnancy because it causes arthropathy (trophic changes in the joints). Used according to the following regimen: 400-800 mg/day once or in 2 doses. During the treatment period, the amount of fluid consumed should be increased.
Suppositories can also cure untreated trichomoniasis. For long-term infections, it is advisable to combine suppositories with oral medications.
Helps against trichomoniasis:
- Flagyl. Antimicrobial, antibacterial agent with antiprotozoal properties. 1 candle is lit per day. Duration of therapy: 10 days. At the end of the course, you should visit a doctor and get checked for vaginal candidiasis. A suppository can provoke a burning sensation in the genitals not only in a woman, but also in her sexual partner. During treatment, ethanol-containing products should be avoided. If this rule is not followed, ethanol intolerance develops.
- Genferon Light. Vaginal-rectal combination drug based on interferon. Has a positive effect on the immune system. Helps speed up the process of regeneration of damaged tissues. Effective against germs, viruses, bacteria. Approved for use in women carrying a child and schoolchildren. For children, suppositories are placed rectally (1 piece 1-2 times/day for 10 days). Women use the drug vaginally according to the following scheme: 1 suppository every 12 hours for 10 days (for initial stage development of the disease) or 1 suppository every 2 days for 2-3 months (chronic forms, advanced and aggravated cases).
Vaccination

Some doctors prefer to treat trichomoniasis with vaccines. They are used for indolent infections, when there are no pronounced symptoms of the disease. They are also contacted when the disease systematically recurs.
Group representative: Solcotrichovac. It is prescribed in medicinal and for preventive purposes with recurrent vaginosis and trichomoniasis. Reduces the chance of reinfection by 80%.
Available in 2 forms: lyophilisate for primary vaccine and lyophilisate for revaccination. The vaccination course includes 3 injections. There should be exactly 14 days between injections.
Special instructions:
- treatment of acute trichomoniasis requires parallel use of etiotropic drugs;
- the medication is administered only after confirmation of the absence of gonorrhea and syphilis;
- the drug is incompatible with methods of treating cancer tumors;
- the prepared suspension is used immediately after dissolving the lyophilisate (takes 30 seconds);
- injections are not given during menstruation;
- method of administration: intramuscular.
Why you can’t self-medicate
Consequences of incorrectly structured therapy:
- Trichomonas become insensitive to antimicrobial medications;
- the likelihood of false negative test results increases;
- the disease becomes chronic, progresses sluggishly, but still poses a threat to health.
The absence of signs of acute inflammation does not mean that the disease has receded and will not return. Against the background of weakened immunity or hormonal imbalance, a dormant infection can become more active. It is for this reason that situations arise when both partners remained faithful to each other, but after a long period of time after treatment for trichomoniasis they became infected with the disease again.
To avoid unpleasant consequences, a woman should make an appointment with a gynecologist or venereologist. The specialist will create an individual treatment program for trichomoniasis.
Pregnancy and trichomoniasis

Key points:
- the fetus in the womb is protected from infection, but it can occur during natural childbirth;
- detection of the disease is not a reason to terminate pregnancy;
- in newborn girls who have received an infection from their mother, acute vulvovaginitis is observed in the first months of life (even to the point of the formation of erosions and the impossibility of carrying out intimate hygiene of the child without the risk of skin damage);
- the disease increases the risk of miscarriage, premature birth, and disruption of the integrity of the membranes of the membranes before the onset of labor.
Every third case of premature rupture of water is explained by the inflammatory process of the mother’s genital organs. For women who have a history of several spontaneous abortions, it is advisable to undergo high-precision tests for trichomoniasis and other sexually transmitted infections.
A comprehensive diagnosis is necessary, since in approximately half of the cases, patients have several diseases of the genitourinary system. It is better to undergo the examination simultaneously in 2-3 clinics that are not associated with each other.
If a pathology is detected, the pregnancy specialist and sexual partner should be notified. The first will determine whether it is worth starting taking medications against trichomoniasis (usually abstain from therapy in the first trimester). The second is obliged to make an appointment with a urologist-venereologist and undergo a course of treatment even if the diagnosis does not reveal the presence of Trichomonas in the body.

Important! For some time, the married couple will have to give up intimacy. The duration of abstinence directly depends on the results of control tests for trichomoniasis, which are taken immediately after the end of treatment.
Starting from the 12th week of pregnancy, Metronidazole can be taken. A woman is prescribed 2 g of the drug (tablets) or suppositories (local drugs are practically ineffective and are not suitable for monotherapy). The medication is taken orally once, at night. Candles are placed for 5-7 days, sometimes 10.
The consequences of using the drug in the 2nd and 3rd trimester have not been sufficiently studied. Tests were carried out only on animals. However, most doctors, based on available clinical data, define Metronidazole as the best remedy against trichomoniasis for women preparing to join the family. Others call Ornidazole a first-line drug. The dosage of this drug is determined based on the woman’s body weight: for each kg there should be 25 mg of the drug.
Attention! Refusal drug therapy In addition to direct health consequences, it also entails childbirth in a special department. People call it "dirty".
After delivery, the child is examined for the presence of Trichomonas. They can be found not only in the tissues of the genital organs, but also in other parts of the body. Quite often the disease attacks the oral cavity and eyes.
After giving birth, the mother herself is obliged to ask for a control test for the disease. Reason: Repeatedly obtained negative results during pregnancy are not so indicative. At the same time, the birth of a child can provoke the activation of chronic infections that were temporarily dormant.
Regimen during therapy
In order for the signs of trichomoniasis not just to fade away, but to disappear forever, you should adhere to certain rules. First of all, the recommendations are suitable for women who take 5-nitroimidazole derivatives.
| What do you need | What not to do |
| Perform intimate hygiene daily. | Alcoholic drinks (with the exception of Ornidazole, all other drugs, when used together with alcohol, provoke hot flashes, chills, tachycardia, and panic attacks). |
| Take pills and suppositories at the same time. | Exposure to ultraviolet light. Consequences: acute pancreatitis, chest pain. |
| Prepare for the introduction of suppositories. Needs to be emptied bladder and wash with warm soapy water. | Use other people's towels. Use a shared bath. Wash yourself immediately after using the medicinal gel or vaginal suppositories. |
| Change bed linen daily. | Use suppositories during menstruation. |
Go to the toilet in the first 30 minutes after inserting the suppository. Try to wash the candle when it burns (the side effect does not require discontinuation of therapy). |
|
| Sleeping in the same bed with someone else. The rule must be followed even if the spouse is also undergoing treatment. |
Note! Spouses have different timing for testing at the end of treatment. Earlier, materials for research are taken from women (approximately 7-10 days). You should not engage in sexual relations until the results of your husband’s therapy are announced.
Trichomoniasis is difficult to determine on your own. Only a systematic visit to the gynecologist preserves the opportunity for a woman to detect the disease in a timely manner. When an infection is detected, it is worth taking note of recommendations on daily routine and behavior. Following the advice will help prevent the pathology from becoming chronic.
Trichomoniasis is one of the urogenital infections that, if not properly treated, can lead to the development of serious complications. In most cases, this disease is diagnosed in females, since women undergo routine examinations more often than men, and also because the signs of infection are more pronounced in them.
Trichomoniasis can only be transmitted during direct sexual intercourse. The household route of infection with this infection through washcloths, wet swimsuits, bed linen, and shared towels is almost impossible. For optimal existence of the infectious agent, it is necessary that the pH level of the vaginal environment (in women) be 5.5-6.6.

Causes of trichomoniasis in women:
sexual intercourse (at the moment of orgasm, Trichomonas penetrates the uterine cavity);
abortion (consequence) or childbirth (natural disruption of the mechanical protection of the uterine cavity due to expansion of the muscles covering the cervix);
the period of menstruation and the period after its end (the acidity of the vaginal environment changes).
Based on the duration and symptoms of the disease, three forms of infection are distinguished:
Trichomonas carriage (the course of the disease is asymptomatic, and Trichomonas is found in the vaginal leucorrhoea);
chronic trichomoniasis (minor clinical manifestations are present) – the duration of the presence of the disease is 2 or more months;
fresh trichomoniasis (asymptomatic, subacute and acute form).
In general, in 10.5% of infected people the infection proceeds independently, and all other cases of the disease are combined with gonorrhea, ureaplasmosis, chlamydia and other pathologies. This behavior of the infection is explained by the fact that Trichomonas is a kind of base for other microorganisms. The frequency of Trichomonas carriage is 2-41%, which is associated with the degree of immunity.

Diagnosis of the disease:
immunological methods (RIFA and PCR diagnostics);
cultural method (sowing material on a special nutrient medium);
microscopic examination of the stained preparation (Romanovsky-Giemsa method, methylene blue, Gram);
microscopy of an unstained (native) smear.
When several diagnostic methods are combined, the detection of trichomoniasis increases significantly.
The first symptoms of trichomoniasis after direct infection
The incubation period of infection is 4-14 days, with the first signs of the disease beginning to appear 4-5 days after infection. With trichomoniasis, the symptoms directly depend on the place of introduction and spread of the infectious agent. In most cases, the infection affects the cervix, urethra, and vagina.

A pathognomic sign of infection is the presence of copious amounts of leucorrhoea discharged from the vagina.
This discharge is yellowish or greenish in color, profuse, foaming.
In addition, vaginal leucorrhoea in the case of trichomoniasis has an unpleasant odor, which, when gardnerella is added, leads to the appearance of a fishy odor.
Quite often the disease is accompanied by dyspareunia (pain during sexual intercourse).
When the infection spreads to the urethral mucosa, urinary disorders (burning, pain, cramping) may appear, and frequent urge to urination, which may indicate the development of urethritis.
Also, almost all patients complain of burning and itching in the vagina, swelling and redness.
Quite rarely, but there are complaints of pain in the lower abdomen.
During a vaginal examination, hyperemia of the vaginal mucosa is observed, with vulvovaginitis present, the cervix is in a softened state and bleeds easily when a speculum touches it. In addition, the contact of vaginal leucorrhoea on the inner surface of the thighs and the skin of the perineum causes irritation of the skin and its ulceration; abrasions and sores of various sizes appear. Trichomonas cervicitis is characterized by a colposcopic conclusion - strawberry cervix. The cervix is visualized by a large number of capillary hemorrhages.
Signs of chronic trichomoniasis
The chronic form of trichomoniasis is a consequence of the neglect of the disease, or its transition from an acute to a chronic form, due to the lack of treatment for this disease in a woman or her sexual partner. Characteristic feature chronic trichomoniasis is the presence of periodic exacerbations and the duration of the course.
Relapses of the disease are promoted by:
ovarian hypofunction;
decreased immunity (hypothermia, general diseases);
alcohol consumption;
sexual intercourse;
menstruation;
non-compliance with the rules of personal intimate hygiene and other factors.

The course of trichomoniasis outside of exacerbation is characterized by mild symptoms. Patients complain of an increase in the number and volume of vaginal leucorrhoea, a feeling of discomfort in the vagina, which intensifies during sexual intercourse. The period of exacerbation of the disease has similar symptoms to the acute form of trichomoniasis.
Complications of trichomoniasis
Chronic trichomoniasis can cause the following consequences:
formation of a malignant process in the cervix;
complications of pregnancy (antenatal and intrapartum fetal death, chorioamnionitis, antenatal rupture of water, premature birth, miscarriage);
sexual disorders (anorgasmia, frigidity);
female infertility - obstruction of the fallopian tubes, chronic inflammation of the uterine appendages.
Today, researchers claim that Trichomonas can cause many diseases, including: oncology of the female reproductive organs, mastopathy, allergic manifestations, diabetes. Some of the statements have been confirmed through research.

Treatment of trichomoniasis
To get rid of the infection, both sexual partners must undergo treatment, even if one of them has no signs of the disease. First of all, during the period of treatment it is necessary to stop drinking alcohol and spicy foods. It is also necessary to maintain sexual rest during the period of therapy and until laboratory confirmation of a negative result, in order to avoid reinfection.
For trichomoniasis, drug treatment in a woman should only be prescribed by a doctor, since self-medication is not allowed. Medicines must have a spectrum of action against anaerobic organisms. In other words, the use of agents belonging to the group of 5-nitroimidazoles is required. Such drugs include:
"Metronidazole" and its analogues ("Ornidazole", "Ternidazole", "Tinidazole", "Flagyl", "Trichopol").
All drugs against trichomoniasis are effective only when administered internally in combination with local therapy (Metrogil gel, vaginal). Invaginal therapy is also carried out using suppositories, one per day for 7-10 days. These can be: “Betadine”, “Klion-D”, “Terzhinan”.
Various treatment regimens for trichomoniasis are used:
"Fasigin" 150 mg 2 times a day for a week;
“Tinidazole” 0.5 grams – 4 tablets at once, single dose;
"Trichopol" 0.5 grams or 1 tablet 2 times a day. Course duration is 7-10 days.

Treatment of the chronic stage of the disease is practically no different from the treatment of the acute stage. In addition to anti-trichomonas drugs, therapy involves taking adaptogens (aralia tincture, Eleutherococcus tincture, Aloe extract), vitamins and immunostimulating agents.
Control tests after a negative response to trichomoniasis are taken for another 3 months during each menstruation.
Prevention measures
Prevention of trichomoniasis infection is practically no different from other urogenital infections and consists of the following:
undergoing regular gynecological examinations (at least twice a year);
compliance with the rules of intimate hygiene;
use of barrier contraceptives (condoms);
confidence in the health of the sexual partner;
presence of a permanent sexual partner (one).
In case of unprotected sexual intercourse, as an emergency measure to prevent infection, you can use the following drugs: “Betadine”, “Miramistin”, which reduce the risk of infection by 70%, provided that the genitals are treated and the vagina is washed no later than after 2 hours after intercourse.

To do this, you need to inject a Betadine or Miramistin solution into the vagina (no more than 5 ml using a urological attachment) or douche with a weak solution of potassium permanganate. The external genitalia must be thoroughly treated with an antiseptic - Miramistin or Chlorhexidine. Such procedures can only be carried out as an emergency protection, since they are not a way to protect against sexually transmitted infections.
Most frequently asked questions from patients
Do people who successfully survive trichomoniasis develop lasting immunity?
No, infection with Trichomonas can occur repeatedly.
Why is it prohibited to drink alcohol during treatment?
How to use vaginal suppositories during menstruation if they are prescribed as a treatment for trichomoniasis?
If, according to your calculations, menstruation will begin soon or has already begun, the use of vaginal suppositories should be postponed until the end. Suppositories can be administered only if there is no bleeding.
Is it possible to treat trichomoniasis during pregnancy and should it be interrupted due to the presence of such a disease?

It is necessary to treat trichomoniasis during pregnancy, and therapy will depend on the trimester of pregnancy. The doctor will prescribe the appropriate treatment option. If the pregnancy is desired, then there is no need to terminate it.
Trichomonas were found in the smears, but the sexual partner’s tests were “clean” and there were no complaints. Is it necessary for him to undergo treatment too?
Treatment of the disease must be carried out without fail for both, regardless of the test results of the sexual partner.
- This parasitic disease, known since ancient times, is sexually transmitted and causes inflammation of the mucous membrane of the genitourinary organs of women and men.
The disease is caused by a special type of microorganism called protozoa. There are many types of protozoan microorganisms found in nature. Some of them live in water and soil, others are parasites in animals and humans.
Who are Trichomonas, types of Trichomonas
Protozoa– single-celled organisms, unlike other single-celled organisms, are capable of movement due to the presence of flagella and independent existence outside the infected organism. In their structure, the simplest are similar to ordinary cells, the totality of which makes up an entire organism. The difference is that protozoa, despite the simplicity of their structure, exist as a separate integral organism.The name trichomoniasis comes from the simplest organisms called trichomonas, which cause specific local pathological phenomena.
Trichomonas, which parasitize the human body, are of three types:
Trcihomonas elongata - lives in the oral cavity.
Trichomonas hominis - lives in the human intestine, feeds on various bacteria, red blood cells (blood cells).
Trichomonas vaginalis – found in the lower genitourinary tract:
- Urethra
- Vagina
- Prostate
Routes of infection with Trichomonas
Trichomoniasis is a very common disease. There is no place on earth where this microorganism does not exist. According to some data, trichomoniasis occurs in both men and women, young and mature, who are sexually active. The disease is transmitted primarily sexually, that is, through unprotected sex.Trichomonas colpitis (vaginitis)
Colpitis– inflammation of the superficial layers of the vaginal mucosa. The term colpitis is borrowed from Greek language. There is also a second name characterizing inflammation of the vaginal mucosa, of Latin origin - vaginitis
Acute trichomonas colpitis is characterized by:
- Unbearable itching, burning in the vaginal area, around the labia. Itching is explained by the irritating effect of trichomonas on the vaginal walls and foamy discharge (secretion).
- Redness and scratching of the skin in the perineal area, labia majora and minora. Appear due to itching in these areas.
- Foamy discharge with a characteristic unpleasant odor. The volume of discharge depends on the phase of the disease. From copious leucorrhoea (discharge) of yellow color, with an acute progressive course, to scanty discharge of gray color, with a chronic, sluggish process. Foaminess and an abundance of secretion appears as a result of vital activity in parallel with Trichomonas, a special type of bacteria that produces gas.
Trichomoniasis in the menopausal period.
In menopausal women, the incidence of trichomoniasis varies widely. Lack of estrogen causes atrophy (decreased functions, thinning of the walls) of the mucous membrane of the vaginal walls. Accordingly, the microflora of the inner surface of the vagina is disrupted, local immunity is reduced, and favorable conditions are created for the growth and development of not only Trichomonas, but also many pathogenic microorganisms. The main clinical symptoms are expressed as:
- Mucopurulent discharge, sometimes streaked with blood
- Itching in the area of the vaginal vestibule
- Rarely, minor bleeding after sexual intercourse
Pregnancy and trichomoniasis
As a rule, trichomoniasis causes inflammatory changes at the local level, that is, at the level of the genital organs. Thus, negatively affecting the course and course of pregnancy. Can cause complications such as: spontaneous abortion and premature birth. The essence of abortion is that Trichomonas cause inflammatory changes, during which special substances called prostaglandins are released into the blood. Prostaglandins cause increased contractions of the uterine muscles, thereby promoting the expulsion of the fetus from the uterine cavity.Disorders of the central nervous system (CNS) 
Inflammatory damage to the mucous membrane, the addition of a secondary purulent infection and profuse foul-smelling vaginal discharge affect the quality of sexual intercourse. Sexual intercourse becomes painful and impossible. Long-term chronic course of the disease can ultimately cause frigidity not only due to pain, but also emotional discomfort, causing in some cases a disturbance in the psycho-emotional state of a woman.
Microscopic method
For diagnosis confirming the presence of trichomonas in the genital tract, it is necessary to take smears from the vaginal mucosa. It is preferable to take swabs from three different places:
Among women
- Posterior vaginal vault
- Cervical canal
- Urethra
- Scraping from the urethra
- Prostate fluid
- Sperm
A gentle massage is usually used to collect prostate fluid. prostate gland.
Laboratory research should be carried out no later than 30 minutes after taking smears, since Trichomonas are very unstable in the external environment and die quickly.
The taken material is placed on a glass slide, a 0.9% sodium chloride solution is dropped, covered with a cover glass and placed under a microscope. In some cases, to better identify trichomonas, smears are pre-stained. Microscopic examination is the most rapid method for diagnosing trichomoniasis and makes it possible to make a diagnosis only 15-20 after taking the starting material.
Cultivation of Trichomonas
As one of the three modern methods for determining a pathological pathogen, it has a number of advantages, such as:
- Allows you to determine the initial amount of Trichomonas in the test material. Indirectly reflects the degree of the inflammatory process.
- It reveals which drugs Trichomonas are sensitive to, which is very important when prescribing the correct and optimal treatment. It also allows you to adjust treatment that has already begun.
PCR method in the diagnosis of trichomoniasis
A very valuable method for detecting Trichomonas. The advantage of this method is that in the chronic course of the disease the pathogen is very difficult to detect using conventional microscopic methods. In addition, any biological fluid body, be it blood, saliva, scraping of the urethral or vaginal mucosa.
The method is based on the fact that Trichomonas DNA, that is, genetic material, can be easily detected in the material being studied. Analysis accuracy is 100%. Results appear the very next day, which allows you to start effective treatment in a timely manner.
Treatment of trichomoniasis
To fully recover from trichomoniasis, the following conditions must be met:- It is necessary to treat both sexual partners at the same time
- During the course of treatment, any sexual contact is excluded
- Use special anti-trichomonas drugs (metronidazole, tinidazole)
- In parallel with treatment, hygiene rules for caring for the genitourinary organs are observed:
- Daily washing of the genitals using antiseptics (a weak solution of potassium permanganate, furatsilin solution) or detergents, that is, ordinary toilet soap.
- All movements when washing are carried out from front to back, that is, from the side of the vagina to anus. This is necessary in order to avoid infection in the urethra.
- Individual use of toiletries (soap, washcloths, towels).
- Daily change of underwear
- Mandatory treatment of other concurrent diseases of the genitourinary organs of infectious and inflammatory origin.
Scheme using metronidazole (Trichopol)
On the first day, take 1 tablet 4 times orally with water.
From the second to the seventh day inclusive, take 1 tablet 3 times a day, also taken orally with water.
Metronidazole– antiprotozoal, antimicrobial drug.
Mechanism of action consists of an inhibitory effect on the genetic apparatus of bacteria. In this case, all biological processes of the cell gradually cease and the microorganism dies.
Contraindication pregnancy and hypersensitivity to the drug.
Tinidazole regimen
Take 4 tablets of 500 mg each at once. Or
For 7 days, 1/3 tablet 2 times a day
Tinidazole
The drug is from the same group as metronidazole with a similar mechanism of action and side effects.
Contraindications –
- hematopoietic disorders
- pregnancy and lactation
- hypersensitivity to the drug
Klion – D- a combination drug that contains equal parts of metronidazole and miconazole (an antifungal drug). Medicine very effective for mixed infections of the genitourinary system of bacterial and fungal origin.
Prescribed in the form of vaginal suppositories, 1 piece at night for 10 days.
Monitoring the effectiveness of treatment antitrichomonas drugs are carried out as follows:
- For 2-3 months after treatment, smears of the contents of the vagina and urethra are taken for microscopic examination for the presence of vaginal trichomonas
- Smears should be taken 1-3 days after menstruation
Prevention of trichomoniasis

Preventive measures imply an integrated approach aimed at protecting against possible infection not only with trichomoniasis, but also with all sexually transmitted diseases, be it gonorrhea, chlamydia, syphilis and many others.
- Prevention should begin with educational activities about healthy way life, the importance of contraceptive methods, routes of transmission of infections that cause inflammatory diseases of the genital tract. These measures are primarily aimed at preventing the occurrence of infectious inflammatory diseases of the genitourinary organs in categories of people of adolescence. Medical workers, teachers in schools, professors in lyceums and universities are required to carry out educational activities in this direction among high school students, students of universities and vocational schools.
- Categories of young and middle-aged people who are sexually active should be careful when choosing a sexual partner. Promiscuous sexual intercourse is not encouraged. The ideal option is an intimate relationship with one sexual partner. The use of condoms plays an important role as a means of preventing unwanted pregnancy and the transmission of Trichomonas infection during sexual intercourse.
- Preventive control by a gynecologist at least once a year, with taking smears from the urethra, posterior vaginal fornix, and cervical canal. The contents from these places are subjected to microscopy, thereby determining the presence of a possible infection and at the same time determining the degree of cleanliness of the vagina.
- Treatment of concomitant diseases of the genitourinary organs caused by other types of pathogenic microorganisms that reduce local immunity and increase the risk of Trichomonas infection.
- An incomparably significant role in the spread of Trichomonas vaginalis is played by the simultaneous use of toiletries (washcloth, towel) by two or more people, one of whom suffers from trichomoniasis. Therefore, it is necessary for each person to have their own body care products and use them individually.
- When preparing for pregnancy, both women and men should be tested for the possible presence of a latent urinary tract infection. And also consult your doctor about this. When planning a pregnancy, it is necessary to cure all possible foci of infection in the woman’s body.
What are the possible consequences of trichomoniasis?
Most often, trichomoniasis causes complications during pregnancy:- premature birth;
- low birth weight of the baby;
- transmission of infection to the child when he passes through the birth canal.
How to eat properly if you have trichomoniasis?
 Dietary habits are more related not to the disease itself, but to the use of anti-trichomoniasis drugs that have antibacterial activity. As with any antibiotics, the diet must be complete, otherwise nausea, indigestion and other side effects may occur. You need to have a hearty breakfast, preferably porridge.
Dietary habits are more related not to the disease itself, but to the use of anti-trichomoniasis drugs that have antibacterial activity. As with any antibiotics, the diet must be complete, otherwise nausea, indigestion and other side effects may occur. You need to have a hearty breakfast, preferably porridge. It is useful to take pancreatic enzyme preparations during the course of treatment, for example Mezim-Forte. You can also take medications containing bifidobacteria, since antibiotics can cause dysbacteriosis. For more detailed advice, contact your healthcare provider.
Do not drink alcohol within 24 hours of taking it metronidazole and within 72 hours after administration tinidazole. These drugs may cause a reaction to ethanol, like “coding” from alcoholism. Nausea, vomiting and other unpleasant symptoms occur.
Is it possible to have sex with trichomoniasis?
 During treatment of trichomoniasis, sex is completely contraindicated for two reasons:
During treatment of trichomoniasis, sex is completely contraindicated for two reasons:- Trichomoniasis is a sexually transmitted infection. This means there is a risk of infecting your partner.
- Sexual intercourse reduces the effectiveness of treatment.
Does a condom protect against trichomoniasis?
 Condoms are one of the simplest, most accessible and effective means of protection against unwanted pregnancy and sexually transmitted infections. But they do not completely protect against either one or the other.
Condoms are one of the simplest, most accessible and effective means of protection against unwanted pregnancy and sexually transmitted infections. But they do not completely protect against either one or the other. Condoms only prevent trichomoniasis by 90%. With constant contact with one sick partner, the likelihood of transmission of infection increases even more.
Do not forget that during sexual intercourse the condom can break and slip off the penis.